Pathophisiology of Sickle Cell Disease and New Drugs for the Treatment
Lucia De Franceschi
Dept of
Clinical and Experimental Medicine, University of Verona, Italy
Correspondence
to:Lucia
De Franceschi, MD. Policlinico GB Rossi, P.le L Scuro 10, 37134 Verona,
Italy. Tel: +390458124918; FAX: +390458027473; E-mail: lucia.defranceschi@univr.it
Published: December 20, 2009
Received: December 23, 2009
Accepted: December 26, 2009
Medit J Hemat Infect Dis 2009, 1(1): e2009024 DOI 10.4084/MJHID.2009.024
This article is available from: http://www.mjhid.org/article/view/5239
This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited
Abstract:
A
homozygous mutation in the gene for b globin, a subunit of adult
hemoglobin A (HbA), is the proximate cause of sickle cell disease
(SCD). Sickle hemoglobin (HbS) shows peculiar biochemical properties,
which lead to polymerizing when deoxygenated. HbS polymerization
is associated with a reduction in cell ion and water content (cell
dehydration), increased red cell density which further accelerate HbS
polymerization. Dense, dehydrated erythrocytes are likely to undergo
instant polymerization in conditions of mild hypoxia due to their high
HbS concentration, and HbS polymers may be formed under normal
oxygen pressure.
Pathophysiological studies have shown that the dense, dehydrated red cells may play a central role in acute and chronic clinical manifestations of sickle cell disease, in which intravascular sickling in capillaries and small vessels leads to vaso-occlusion and impaired blood flow in a variety of organs and tissue. The persistent membrane damage associated with HbS polymerization also favors the generation of distorted rigid cells and further contributes to vaso-occlusive crisis (VOCs) and cell destruction in the peripheral circulation. These damaged, dense sickle red cells also show a loss of phospholipid asymmetry with externalization of phosphatidylserine (PS), which is believed to play a significant role in promoting macrophage recognition with removal of erythrocytes (erythrophagocytosis), cell apoptosis and activation of coagulation. Vaso-occlusive events in the microcirculation result from a complex scenario involving the interactions between different cell types, including dense, dehydrated sickle cells, reticulocytes, abnormally activated endothelial cells, leukocytes, platelets and plasma factors such as cytokine and oxidized pro-inflammatory lipids Hydroxycarbamide (hydroxyurea) is currently the only drug approved for chronic administration in adult patients with sickle cell disease to prevent acute painful crises and reduce the incidence of transfusion and acute chest crises. Long-term use of hydroxycarbamide has been demonstrated to produce dramatic reductions in mortality and morbidity in patients with sickle cell disease.
We will focus here on therapeutic strategies currently being considered for the treatment of sickle cell disease, which are not based on Hb F modulation. They include:
Pathophysiological studies have shown that the dense, dehydrated red cells may play a central role in acute and chronic clinical manifestations of sickle cell disease, in which intravascular sickling in capillaries and small vessels leads to vaso-occlusion and impaired blood flow in a variety of organs and tissue. The persistent membrane damage associated with HbS polymerization also favors the generation of distorted rigid cells and further contributes to vaso-occlusive crisis (VOCs) and cell destruction in the peripheral circulation. These damaged, dense sickle red cells also show a loss of phospholipid asymmetry with externalization of phosphatidylserine (PS), which is believed to play a significant role in promoting macrophage recognition with removal of erythrocytes (erythrophagocytosis), cell apoptosis and activation of coagulation. Vaso-occlusive events in the microcirculation result from a complex scenario involving the interactions between different cell types, including dense, dehydrated sickle cells, reticulocytes, abnormally activated endothelial cells, leukocytes, platelets and plasma factors such as cytokine and oxidized pro-inflammatory lipids Hydroxycarbamide (hydroxyurea) is currently the only drug approved for chronic administration in adult patients with sickle cell disease to prevent acute painful crises and reduce the incidence of transfusion and acute chest crises. Long-term use of hydroxycarbamide has been demonstrated to produce dramatic reductions in mortality and morbidity in patients with sickle cell disease.
We will focus here on therapeutic strategies currently being considered for the treatment of sickle cell disease, which are not based on Hb F modulation. They include:
- Use of agents which reduce or prevent sickle cell dehydration
- Use of agents which reduce sickle cell-endothelial adhesive events
- Use of nitric oxide (NO) or NO-related compounds
Introduction
Conclusion
A
homozygous mutation in the gene for b globin, a subunit of adult
hemoglobin A (HbA), is the proximate cause of sickle cell disease
(SCD). Sickle hemoglobin (HbS) shows peculiar biochemical properties,
which lead to polymerizing when deoxygenated. Studies of the kinetics
of HbS polymerization following deoxygenation have shown it to be a
high order exponential function of haemoglobin concentration, thus
highlighting a crucial role for cellular HbS concentration in
sickling [1, 2]. HbS polymerization is associated with
a reduction in
cell ion and water content (cell dehydration), increased red cell
density which further accelerate HbS polymerization [1-3].
Dense,
dehydrated erythrocytes are likely to undergo instant polymerization in
conditions of mild hypoxia due to their high HbS concentration, and HbS
polymers may be formed under normal oxygen pressure.
Pathophysiological studies have shown that the dense, dehydrated red cells may play a central role in acute and chronic clinical manifestations of sickle cell disease, in which intravascular sickling in capillaries and small vessels leads to vaso-occlusion and impaired blood flow in a variety of organs and tissues [2, 4]. The persistent membrane damage associated with HbS polymerization also favors the generation of [5]distorted rigid cells and further contributes to vaso-occlusive crisis (VOCs) and cell destruction in the peripheral circulation. These damaged, dense sickle red cells also show a loss of phospholipid asymmetry with externalization of phosphatidylserine (PS), which is believed to play a significant role in promoting macrophage recognition with removal of erythrocytes (erythrophagocytosis), cell apoptosis and activation of coagulation. Although the percentage of dense erythrocytes does not predict the severity of the disease, it has been shown to increase prior to or during the first phase of the painful crisis and to decrease thereafter [4, 6, 7]. Vaso-occlusive events in the microcirculation result from a complex scenario involving the interactions between different cell types, including dense, dehydrated sickle cells, reticulocytes, abnormally activated endothelial cells, leukocytes, platelets and plasma factors such as cytokines[8,9] and oxidized pro-inflammatory lipids [6, 10, 11].
Hydroxycarbamide (hydroxyurea) is currently the only drug approved for chronic administration in adult patients with sickle cell disease to prevent acute painful crises and reduce the incidence of transfusion and acute chest crises.[12] Long-term use of hydroxycarbamide has been demonstrated to produce dramatic reductions in mortality and morbidity in patients with sickle cell disease. [13] Clinical use of hydroxycarbamide in pediatric and adult patients with sickle cell disease is discussed in the next chapter on clinical management (13.2). Decitabine has also been shown to be a promising agent for the modulation on Hb F in sickle cell disease.[14]
We will focus here on therapeutic strategies currently being considered for the treatment of sickle cell disease, which are not based on Hb F modulation. They include:
One of the distinguishing characteristics of sickle cell disease is the presence of dense erythrocytes, formed as a result of cell dehydration and loss of potassium (K+). These dense red cells generally have a lower HbF content and include both reticulocytes and red cells.[15] Usually, the dense fraction of erythrocytes has a high percentage of irreversible sickle cells (ISCs), cells that maintain their sickle shape even when fully oxygenated. An inverse correlation has been demonstrated between percentage of ICSs and erythrocyte survival. In vitro and in vivo studies in animal models for sickle cell disease have suggested a crucial role of dehydrated red cells in the pathogenesis of vaso-occlusive events; in fact, the dense, dehydrated red cells might be easily trapped in post capillary venules, promoting micro-vascular obstruction [16].
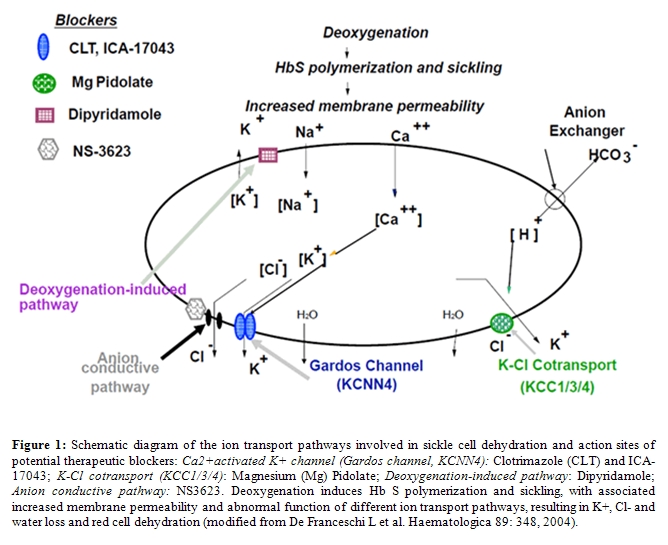
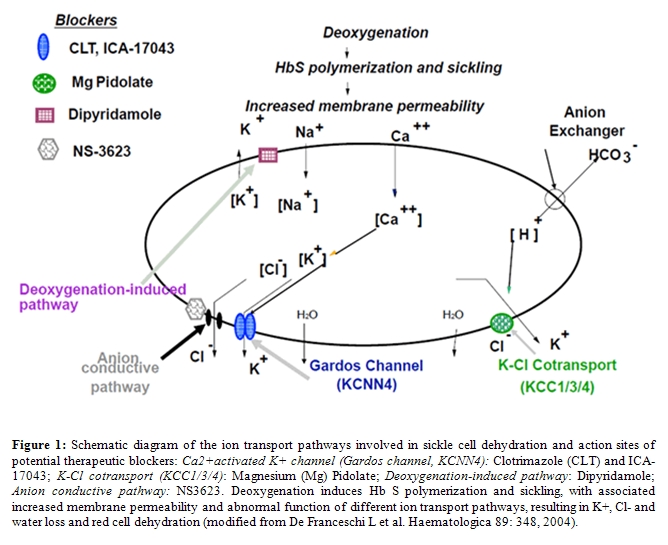
Thus, prevention of red cell dehydration represents an exciting possible new therapeutic strategy. Studies on membrane permeability in sickle cell disease have shown abnormalities in different specialized membrane-embedded transporters that carry cations, anions and water across the erythrocyte membrane. In the last two decades, studies on the nature and properties of the pathways mediating K+ loss in sickle cell erythrocytes have led to the development of new therapeutic tools to block K+ loss and dehydration. The major pathways for K+ loss during sickle cell dehydration events are the Ca2+-activated K+ channel, known as Gardos channel, operating in parallel with the conductive Cl- pathway and the electroneutral K-Cl cotransport (Figure 1) [17-22].
Ca2+-activated K+ channel (Gardos channel, KCNN4)
Sickle red cells are characterized by increased amounts of calcium, which is functionally and physically sequestered into intracellular vesicles, but maintained in normal concentration in the steady state. The cyclic deoxygenation and HbS polymerization that occurs in sickle red cells has been shown to produce transient increase in free intracellular calcium, which is responsible for large K+ loss with associated Cl- and water loss. This effect is due to activation of a specific Ca-gated K+ channel that was first described by Gardos.[23]
The imidazole antimycotic clotrimazole (CLT) has shown to be a specific inhibitor of the Gardos channel and to prevent sickle cell dehydration in vitro.[18] In a transgenic mouse model of sickle cell disease, oral administration of CLT was reported to specifically block the Gardos channel, increase the red cell K+ content and reduce red cell dehydration.[24] The compound was further tested in normal humans (AA) and in sickle cell volunteers (SS), and was shown to be a powerful and effective inhibitor of the erythroid Gardos channel and of sickle red cell dehydration.[25, 26] Further studies led to the development of a novel class of compounds based on the back-bone structure of CLT, which have conserved Gardos channel inhibitory power, but are devoid of the imidazole moiety of CLT, and thus of cytochrome P450 inhibitory effects.[27] One of these compounds (ICA-17043) has been shown to have 10-fold greater potency than CLT in blocking the Gardos channel in vitro and in vivo to specifically inhibit Gardos channel and prevent K+ loss and red cell dehydration[28]. Phase I studies in normal human subjects and in sickle cell patients, showed significant blockade of the Gardos channel, in absence of any significant side-effects. [29] A phase II study showed that ICA-17043 reduced haemolysis and the percentage of dense cells, with a significant amelioration of anaemia in patients with sickle cell disease.[30] However, a Phase III clinical trial showed no effect of ICA-17043 on the rate of painful events in SCD patients, most likely related with some effects on blood viscosity of red cells displaying an increase survival. No other studies have been planned with this molecule.
Another therapeutic agent, which has been recently shown to modulate the Gardos channel activity, is L-Arginine. Patients with SCD show a state of relative depletion of arginine, which is part of the nitric oxide pathway. L-Arginine supplementation of transgenic sickle cell mice resulted in inhibition of erythrocyte Gardos channel activity and amelioration of red cell dehydration [16]. A phase II study to test the effect of arginine supplementation have shown no major effects on Gardos channel function and erythrocyte hydration in patients with sickle cell disease [31, 32].
K-Cl cotransport (KCC1/3/4)
Several forms of K-Cl cotransport have been described in various human and mouse tissues. KCC2 expression seems to be limited to brain cells, while human and mouse erythrocytes seem to possess KCC1, KCC3 and KCC4 isoforms in different and still undetermined ratio. The K-Cl cotransport mediates red cell dehydration in SCD. Studies on K-Cl cotransport function have identified different triggers of activation, such as cell swelling, cell acidification, reduced cell magnesium (Mg2+) content, membrane oxidative damage and urea. Franco et al. [22] have also shown that K-Cl cotransport mainly contributes to dehydration of sickle reticulocytes and that deoxygenation of sickle red cells also stimulates K-Cl cotransport in isotonic solutions at pH 7.4 (Figure 1). The relative contribution of the Gardos channel and of the K-Cl cotransport pathway in generating dehydrated, dense sickle red cells is a complex and still unresolved issue. K-Cl cotransport activity is modulated by red cell Mg content and low Mg2+ levels are associated with abnormal activation of K-Cl cotransport. Some small studies have reported a reduction in red cell Mg2+ content in SCD patients. Thus, oral Mg supplementation with the aim of increasing red cell Mg2+ levels and inhibiting K-Cl cotransport activity may represent a possible therapeutic strategy for ameliorating SCD red cell dehydration [16, 17]. Dietary magnesium supplementation in transgenic sickle cell mice has demonstrated that increasing erythrocyte Mg2+ content can ameliorate red cell dehydration. Two uncontrolled trials of oral supplementation with Mg pidolate have been carried out in sickle cell patients, showing a reduction in K-Cl cotransport activity, an increase in red cell K+ and Mg2+ content, an improvement in red cell dehydration and a reduction in the number of painful events.[17, 33] A double-blind, placebo controlled crossover study with Mg pidolate supplementation in children with sickle cell disease did not demonstrate any significant changes in the haematological parameters studied; however, the Mg-pidolate dosage used was markedly lower than that proposed in the previous studies. In a phase I study, the therapeutic association of Mg-pidolate with hydroxyurea have been evaluated in patients with HbSC disease, showing a significant reduction in the activity of the K-Cl cotransport after 3 months of supplementation [34].
Recently, it has been reported that infusion of Mg sulfate reduces the length of stay of sickle cell patients hospitalized during vaso-occlusive crises [16].
Cl- permeability pathway
Studies on the conductive Cl- pathway indicate that for red cell dehydration the movement of K+ must be accompanied by that of chloride (or other monovalent anions) to maintain electroneutrality (Figure 1). Elegant sets of studies demonstrate that movement of K+ and dehydration via the Gardos channel can be blocked if the Cl- conductive pathway is inhibited. A specific inhibitor of Cl-conductance has been recently developed (NS3623). NS3623 has been tested in transgenic sickle cell mice and was found to reduce in vivo sickle cell dehydration, with a mild echinocytosis at the highest doses. Unfortunately, NS3623 was not further developed for clinical use because of undesirable side effects observed in human subjects [16, 19].
2) Anti-adherence therapy in sickle cell disease
Vaso-occlusive episodes are central events in the pathophysiology of sickle cell disease, causing the clinical manifestations and leading to acute and chronic organ damage. The abnormal adhesive interactions between erythrocyte, reticulocytes, endothelial cells, platelets or soluble mediators may represent a possible new therapeutic target. In addition, SCD patients showed abnormally activated circulating endothelial cells that increase during acute vaso-occlusive crisis suggesting the presence of chronic vascular endothelial damage further worsening during acute events [4, 35-37]. The end-point of anti-adherence therapy is to interfere with the initialization and/or amplification of adhesive events. Although anti-adherence therapy has been mainly studied during acute painful events, its mechanisms of action are only partially known [4, 6, 38-40]
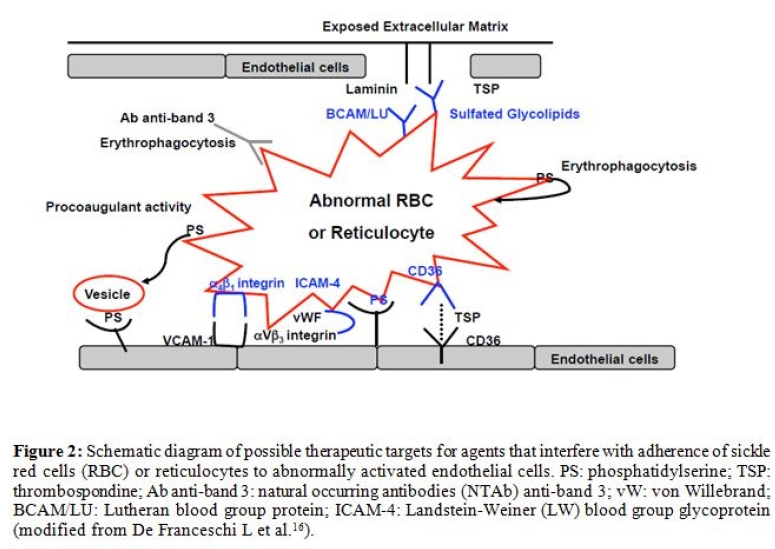
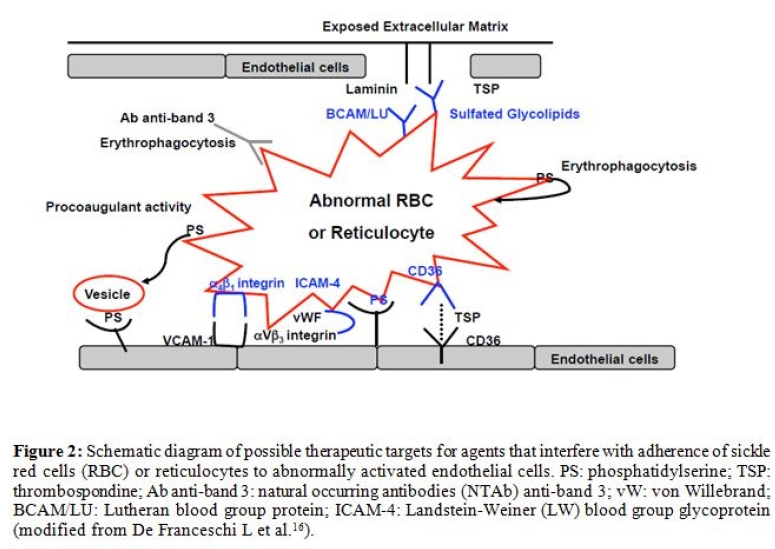
In SCD, the anti-adherence therapeutic strategies (Figure 2) can be divided into:
i. Molecules interfering with chemical-physical processes during erythrocyte-endothelial adhesion events
ii. Molecules interfering with sickle cell-endothelial adhesive mechanisms
iii. Molecules modulating inflammatory pathways involved in sickle cell-endothelial adhesion
iv. The heme-oxygenase-1 (HO-1) connection
Molecules interfering with chemical-physical processes during erythrocyte-endothelial adhesion events: Non-ionic surfactant block copolymer such as RheothRx (Poloxamer 188) lowering viscosity and frictional forces improves microvascular blood flow. RheothRx has been shown to block hydrophobic adhesive interactions (cell-cell, cell-protein or protein-protein interaction) in blood, resulting in reduction of erythrocyte aggregation and red cell adherence to vascular endothelium, with a hypothetical improvement in microvascular flow [41]. Phase II studies have shown a limited favorable effect in treatment of acute pain crises, when associated with hydroxyurea (HU) in sickle cell children. However, no further clinical development studies are planned for this compound.
Molecules interfering with sickle cell-endothelial adhesive mechanisms: Recent studies on the sickle cell-endothelium adhesive mechanism have identified different interactions which may have particular therapeutic relevance: a) the integrin a a4bb1 receptor of fibronectin and the vascular adhesion molecule –1 (VCAM-1), E-selectin and P-selectin; b) the thrombospondin and/or collagen and receptor CD36, present on the surface of endothelial cells, platelets and reticulocyte-rich subpopulations of normal and sickle erythrocytes; c) the sulfate glycolipids, which bind thrombospondin, von Willebrand factor multimer and laminin [2, 42, 43]; d) the Lutheran blood group proteins (BCAM/LU), which expression is increased in red cells from SCD patients that bind to a5 subunit of laminin, a component of extracellular subendothelial matrix [44, 45]; e) the ICAM-4 (Landstein-Weiner blood group glycoprotein- LW), which binds aVb3 integrin receptors on endothelial cells [46-49]; and f) the exposure of phosphatydyl-serine (PS), detectable in a subpopulation of sickle red cells, which participates in sickle cell adhesion to activated endothelium [50-54] (Figure 2). Ex vivo and in vitro experimental studies have shown that thrombospondin- and von Willebrand factor-mediated interaction between sickle red cells and endothelium via a Vb3 integrin might be blocked by monoclonal antibodies against aVb3 integrin receptors [42, 48, 55]. Recent study with short synthetic peptides interfering with ICAM-4 and a Vb3 integrin binding have been evaluated in ex vivo system, showing a reduction in sickle erythrocyte adhesion to activated endothelial cells allowing to consider the blocking of this adhesion pathway as possible therapeutic new strategy in treatment of acute sickle cell events [48, 55]. The binding between thrombospondin, von Willebrand factor and laminin, which mediates sickle cell-endothelial adherence, might be blocked by anionic polysaccharides such as high molecular weight dextran sulfate or chondroitin sulfate [2, 42, 43]. An additional therapeutic approach to block sickle cell adhesion to endothelial cells is heparin that might interfer with sickle cell adhesion to endothelial cells through P-selectin[56-59] or binding to TSP that can mediate the interactions between sickle erythrocytes and the vascular endothelial surface. A double blind randomized trial with tinzaparin in SCD patients during acute VOCs has documented a reduction of severit and duration of the VOCs [51, 60].
Molecules modulating inflammatory pathways involved in sickle cell-endothelial adhesion: Chronic inflammatory state has been described in SCD patients characterized by increase plasma levels of acute phase proteins, of soluble cytokines such as IL1b, IL6, TNF- a and endothelin-1 (ET-1) that are further elevated during acute VOCs. These factors participate to leukocyte chemotasis, modulate vascular tone and contribute in sickle cell related tissue damage. Thus, anti-inflammatory therapy has been propose to interfere with inflammatory storm and abnormal vascular activation [61]. Sulfasalazine is an anti-inflammatory molecule and can inhibit the transcription of nuclear factor NF-kB and interferring with endothelial cell activation [62-65]. Transgenic sickle cell mice treated with sulfasalazine show a reduction in activated circulating endothelial cells, and in VCAM-1, ICAM and E-selectin vascular wall endothelial expression. In a pilot study, the administration of sulfasalazine to sickle cell patients results in reduction in the abnormal endothelial activation [4]. Another possible strategy aimed at reducing the adhesion of sickle red cells to vascular endothelium is the inhibition of interactions between leukocytes already adherent to endothelium and sickle red cells during vaso-occlusive events [66]. Based on the in vitro evidence that immunoglobulin (Ig ) significantly reduces the binding of sickle red cells to neutrophils in transgenic sickle cell mice, the infusion of Ig in vivo was shown to inhibit the interaction between sickle red cells and leukocytes in the cremasteric venules, suggesting that Ig may act either by inhibitiing the interactions between sickle red cells and leukocytes and/or by reducing the number of adherent leukocytes [66]. In humans, three out of four sickle cell patients treated with infusion of Ig showed some beneficial effect, whereas in the fourth case the treatment accelerated a vaso-occlusive crisis [66, 67].Since Ig infusion might be related to severe side effects such as renal toxicity and thrombosis, it should be used with caution in sickle cell patients. Recent studies have shown the important role of ET-1 in acute sickle cell related VOCs in a mouse model for SCD [68, 69]. The block of ET-1 actions was obtained directly by the ET-1 receptors antagonist, Bosentan, evaluating its effects on SCD mouse kidney as target organ and indirectly by the inhibition of phosphodiesterase-4 with Rolipram in a model of early pulmonary hypertension [68, 69]. Bosentan is actually under evaluation in a phase III clinical trial in SCD patients with pulmonary hypertension [70].
The possibility of delivering oxygen directly to sickled red cells entrapped in partially obstructed vessels has also been explored. Perflubron-based fluorocarbon emulsion (PFE) decreases the peripheral vascular resistance ex vivo in the mesocaecal vasculature of rats, due more to its ability to dissolve oxygen than to its ability to modify the vascular tone. [71]
Recently, Hebbel et al have reported the beneficial effects of histone deacetylase inhibitors on vascular pathology in mouse model for sickle cell disease [72]. The Authors observed multiple therapeutic effects of these compounds as: (i) inducers of HbF; (ii) iron chelators; (iii) modulators of vascular damage and abnormal activation sickle cell related (i.e.: reduction of VCAM-1 expression).
The heme-oxygenase-1 (HO-1) connection. In different sickle cell mouse models under steady state, Belcher et al have shown up-regulation of cytoprotective gene as heme oxygenase-1 (HO-1) and a reduction of the sickle cell related organ damage when pathological mice were treated with heme oxygenase-1 products [63, 73]. In SCD patients in steady state, the gene expression profiling of circulating leukocytes has shown increased HO-1 and biliverdin reductase as well as in kidney and in circulating endothelial cells [74, 75], suggesting an induction of cell protective systems in response to chronic inflammatory stress characterizing SCD. However, the still open question is whether these cytoprotective systems are rapidly and further induced driving a continuous cellular protection during acute sickle cell vaso-occlusive crisis.
3) Nitric Oxide (NO) based therapies in sickle cell disease:
Nitric oxide (NO) is a potent vasodilator and inhibitor of vascular remodeling and also affects the multi-step cascade of events involved in leukocyte, platelet and endothelial activation. NO is generated from L-Arginine by endothelial cells via constitutive (eNOS) and inflammatory inducible nitric oxide synthases (iNOS). SCD is characterized by relative reduction in NO bioavaibility that contributes to endothelial abnormal activation and SCD organ damage. In addition chronic hemolysis leading to increase the plasma levels of hemoglobin that is an efficient NO buffer, contributes in reducing NO levels in SCD. Recent studies have focused on inhaled NO for the treatment of tissue damage in various ischaemic syndromes, including cardiovascular disease, pulmonary hypertension, and acute lung distress syndromes. The possible therapeutic role of inhaled NO has been studied in different animal models of lung injury induced by ischaemia/reperfusion. Inhaled NO prevents leukocyte migration and reduces the permeability of the peripheral microvasculature. In association with surfactant, inhaled NO alleviates alveolar edema and reduces bronchoalveolar leukocyte and neutrophil infiltration in animal models of ischaemic lung injury. A placebo-controlled randomized clinical trial of inhaled NO in SCD has recently reported beneficial results in the treatment of acute vaso-occlusive crisis, although the mechanism of action remains unknown. Plasma NO metabolites are decreased in SCD patients during vaso-occlusive crisis associated with severe pain and also in acute chest syndrome [32]. A decrease in exhaled NO has been reported in sickle cell patients, suggesting a role for NO in the pathogenesis of the pulmonary complications [76]. In a transgenic mouse model of sickle cell disease, it has been shown that inhaled NO provides protection during ischaemia/reperfusion lung injury, in which endothelial NO production is reduced [77, 78]. In addition NO-donor as polynitroxy-albumine and nitroxic- albumine have been shown to be effective in reducing inflammatory state in a SCD mouse strain and to reduce the hypoxia induce lung damage in another mouse model of acute VOCs [79, 80]. Another possible therapeutic strategy for increased NO production in sickle cell disease is supplementation of L-Arginine. Morris et al showed that L-Arginine supplementation alone induces an unexpected decrease in NO metabolite production [11, 81]. In a subsequent pilot study, an increase in NO metabolites was observed when L-Arginine was co-administrated with HU, suggesting that the combination treatment may have a synergistic effect on NO production [2, 31]. A phase II trial on L-Arginine supplementation in SCD has shown no effects on NO levels and on erythrocyte features.
4) Antioxidant agents in sickle cell disease
SCD is characterized by a pro-oxidant environment due to high production of reactive oxygen species (ROS) related to increased levels of free pathological iron and heme groups associated with a reduction in antioxidant systems such as GSH [82-85]. Studies in vitro on SCD red cells have shown that iron chelation by deferipone (L1) reduce the sickle red cell membrane susceptibility to iron mediated oxidative damage [82, 86]. In vivo study on SCD patients supplemented with L-glutamate to increase GSH and glutamate levels have shown some improvement of chronic pain [83]
Pathophysiological studies have shown that the dense, dehydrated red cells may play a central role in acute and chronic clinical manifestations of sickle cell disease, in which intravascular sickling in capillaries and small vessels leads to vaso-occlusion and impaired blood flow in a variety of organs and tissues [2, 4]. The persistent membrane damage associated with HbS polymerization also favors the generation of [5]distorted rigid cells and further contributes to vaso-occlusive crisis (VOCs) and cell destruction in the peripheral circulation. These damaged, dense sickle red cells also show a loss of phospholipid asymmetry with externalization of phosphatidylserine (PS), which is believed to play a significant role in promoting macrophage recognition with removal of erythrocytes (erythrophagocytosis), cell apoptosis and activation of coagulation. Although the percentage of dense erythrocytes does not predict the severity of the disease, it has been shown to increase prior to or during the first phase of the painful crisis and to decrease thereafter [4, 6, 7]. Vaso-occlusive events in the microcirculation result from a complex scenario involving the interactions between different cell types, including dense, dehydrated sickle cells, reticulocytes, abnormally activated endothelial cells, leukocytes, platelets and plasma factors such as cytokines[8,9] and oxidized pro-inflammatory lipids [6, 10, 11].
Hydroxycarbamide (hydroxyurea) is currently the only drug approved for chronic administration in adult patients with sickle cell disease to prevent acute painful crises and reduce the incidence of transfusion and acute chest crises.[12] Long-term use of hydroxycarbamide has been demonstrated to produce dramatic reductions in mortality and morbidity in patients with sickle cell disease. [13] Clinical use of hydroxycarbamide in pediatric and adult patients with sickle cell disease is discussed in the next chapter on clinical management (13.2). Decitabine has also been shown to be a promising agent for the modulation on Hb F in sickle cell disease.[14]
We will focus here on therapeutic strategies currently being considered for the treatment of sickle cell disease, which are not based on Hb F modulation. They include:
- Use of agents which reduce or prevent sickle cell dehydration
- Use of agents which reduce sickle cell-endothelial adhesive events
- Use of nitric oxide (NO) or NO-related compounds
- Use of antioxidant agents
One of the distinguishing characteristics of sickle cell disease is the presence of dense erythrocytes, formed as a result of cell dehydration and loss of potassium (K+). These dense red cells generally have a lower HbF content and include both reticulocytes and red cells.[15] Usually, the dense fraction of erythrocytes has a high percentage of irreversible sickle cells (ISCs), cells that maintain their sickle shape even when fully oxygenated. An inverse correlation has been demonstrated between percentage of ICSs and erythrocyte survival. In vitro and in vivo studies in animal models for sickle cell disease have suggested a crucial role of dehydrated red cells in the pathogenesis of vaso-occlusive events; in fact, the dense, dehydrated red cells might be easily trapped in post capillary venules, promoting micro-vascular obstruction [16].
Thus, prevention of red cell dehydration represents an exciting possible new therapeutic strategy. Studies on membrane permeability in sickle cell disease have shown abnormalities in different specialized membrane-embedded transporters that carry cations, anions and water across the erythrocyte membrane. In the last two decades, studies on the nature and properties of the pathways mediating K+ loss in sickle cell erythrocytes have led to the development of new therapeutic tools to block K+ loss and dehydration. The major pathways for K+ loss during sickle cell dehydration events are the Ca2+-activated K+ channel, known as Gardos channel, operating in parallel with the conductive Cl- pathway and the electroneutral K-Cl cotransport (Figure 1) [17-22].
Ca2+-activated K+ channel (Gardos channel, KCNN4)
Sickle red cells are characterized by increased amounts of calcium, which is functionally and physically sequestered into intracellular vesicles, but maintained in normal concentration in the steady state. The cyclic deoxygenation and HbS polymerization that occurs in sickle red cells has been shown to produce transient increase in free intracellular calcium, which is responsible for large K+ loss with associated Cl- and water loss. This effect is due to activation of a specific Ca-gated K+ channel that was first described by Gardos.[23]
The imidazole antimycotic clotrimazole (CLT) has shown to be a specific inhibitor of the Gardos channel and to prevent sickle cell dehydration in vitro.[18] In a transgenic mouse model of sickle cell disease, oral administration of CLT was reported to specifically block the Gardos channel, increase the red cell K+ content and reduce red cell dehydration.[24] The compound was further tested in normal humans (AA) and in sickle cell volunteers (SS), and was shown to be a powerful and effective inhibitor of the erythroid Gardos channel and of sickle red cell dehydration.[25, 26] Further studies led to the development of a novel class of compounds based on the back-bone structure of CLT, which have conserved Gardos channel inhibitory power, but are devoid of the imidazole moiety of CLT, and thus of cytochrome P450 inhibitory effects.[27] One of these compounds (ICA-17043) has been shown to have 10-fold greater potency than CLT in blocking the Gardos channel in vitro and in vivo to specifically inhibit Gardos channel and prevent K+ loss and red cell dehydration[28]. Phase I studies in normal human subjects and in sickle cell patients, showed significant blockade of the Gardos channel, in absence of any significant side-effects. [29] A phase II study showed that ICA-17043 reduced haemolysis and the percentage of dense cells, with a significant amelioration of anaemia in patients with sickle cell disease.[30] However, a Phase III clinical trial showed no effect of ICA-17043 on the rate of painful events in SCD patients, most likely related with some effects on blood viscosity of red cells displaying an increase survival. No other studies have been planned with this molecule.
Another therapeutic agent, which has been recently shown to modulate the Gardos channel activity, is L-Arginine. Patients with SCD show a state of relative depletion of arginine, which is part of the nitric oxide pathway. L-Arginine supplementation of transgenic sickle cell mice resulted in inhibition of erythrocyte Gardos channel activity and amelioration of red cell dehydration [16]. A phase II study to test the effect of arginine supplementation have shown no major effects on Gardos channel function and erythrocyte hydration in patients with sickle cell disease [31, 32].
K-Cl cotransport (KCC1/3/4)
Several forms of K-Cl cotransport have been described in various human and mouse tissues. KCC2 expression seems to be limited to brain cells, while human and mouse erythrocytes seem to possess KCC1, KCC3 and KCC4 isoforms in different and still undetermined ratio. The K-Cl cotransport mediates red cell dehydration in SCD. Studies on K-Cl cotransport function have identified different triggers of activation, such as cell swelling, cell acidification, reduced cell magnesium (Mg2+) content, membrane oxidative damage and urea. Franco et al. [22] have also shown that K-Cl cotransport mainly contributes to dehydration of sickle reticulocytes and that deoxygenation of sickle red cells also stimulates K-Cl cotransport in isotonic solutions at pH 7.4 (Figure 1). The relative contribution of the Gardos channel and of the K-Cl cotransport pathway in generating dehydrated, dense sickle red cells is a complex and still unresolved issue. K-Cl cotransport activity is modulated by red cell Mg content and low Mg2+ levels are associated with abnormal activation of K-Cl cotransport. Some small studies have reported a reduction in red cell Mg2+ content in SCD patients. Thus, oral Mg supplementation with the aim of increasing red cell Mg2+ levels and inhibiting K-Cl cotransport activity may represent a possible therapeutic strategy for ameliorating SCD red cell dehydration [16, 17]. Dietary magnesium supplementation in transgenic sickle cell mice has demonstrated that increasing erythrocyte Mg2+ content can ameliorate red cell dehydration. Two uncontrolled trials of oral supplementation with Mg pidolate have been carried out in sickle cell patients, showing a reduction in K-Cl cotransport activity, an increase in red cell K+ and Mg2+ content, an improvement in red cell dehydration and a reduction in the number of painful events.[17, 33] A double-blind, placebo controlled crossover study with Mg pidolate supplementation in children with sickle cell disease did not demonstrate any significant changes in the haematological parameters studied; however, the Mg-pidolate dosage used was markedly lower than that proposed in the previous studies. In a phase I study, the therapeutic association of Mg-pidolate with hydroxyurea have been evaluated in patients with HbSC disease, showing a significant reduction in the activity of the K-Cl cotransport after 3 months of supplementation [34].
Recently, it has been reported that infusion of Mg sulfate reduces the length of stay of sickle cell patients hospitalized during vaso-occlusive crises [16].
Cl- permeability pathway
Studies on the conductive Cl- pathway indicate that for red cell dehydration the movement of K+ must be accompanied by that of chloride (or other monovalent anions) to maintain electroneutrality (Figure 1). Elegant sets of studies demonstrate that movement of K+ and dehydration via the Gardos channel can be blocked if the Cl- conductive pathway is inhibited. A specific inhibitor of Cl-conductance has been recently developed (NS3623). NS3623 has been tested in transgenic sickle cell mice and was found to reduce in vivo sickle cell dehydration, with a mild echinocytosis at the highest doses. Unfortunately, NS3623 was not further developed for clinical use because of undesirable side effects observed in human subjects [16, 19].
2) Anti-adherence therapy in sickle cell disease
Vaso-occlusive episodes are central events in the pathophysiology of sickle cell disease, causing the clinical manifestations and leading to acute and chronic organ damage. The abnormal adhesive interactions between erythrocyte, reticulocytes, endothelial cells, platelets or soluble mediators may represent a possible new therapeutic target. In addition, SCD patients showed abnormally activated circulating endothelial cells that increase during acute vaso-occlusive crisis suggesting the presence of chronic vascular endothelial damage further worsening during acute events [4, 35-37]. The end-point of anti-adherence therapy is to interfere with the initialization and/or amplification of adhesive events. Although anti-adherence therapy has been mainly studied during acute painful events, its mechanisms of action are only partially known [4, 6, 38-40]
In SCD, the anti-adherence therapeutic strategies (Figure 2) can be divided into:
i. Molecules interfering with chemical-physical processes during erythrocyte-endothelial adhesion events
ii. Molecules interfering with sickle cell-endothelial adhesive mechanisms
iii. Molecules modulating inflammatory pathways involved in sickle cell-endothelial adhesion
iv. The heme-oxygenase-1 (HO-1) connection
Molecules interfering with chemical-physical processes during erythrocyte-endothelial adhesion events: Non-ionic surfactant block copolymer such as RheothRx (Poloxamer 188) lowering viscosity and frictional forces improves microvascular blood flow. RheothRx has been shown to block hydrophobic adhesive interactions (cell-cell, cell-protein or protein-protein interaction) in blood, resulting in reduction of erythrocyte aggregation and red cell adherence to vascular endothelium, with a hypothetical improvement in microvascular flow [41]. Phase II studies have shown a limited favorable effect in treatment of acute pain crises, when associated with hydroxyurea (HU) in sickle cell children. However, no further clinical development studies are planned for this compound.
Molecules interfering with sickle cell-endothelial adhesive mechanisms: Recent studies on the sickle cell-endothelium adhesive mechanism have identified different interactions which may have particular therapeutic relevance: a) the integrin a a4bb1 receptor of fibronectin and the vascular adhesion molecule –1 (VCAM-1), E-selectin and P-selectin; b) the thrombospondin and/or collagen and receptor CD36, present on the surface of endothelial cells, platelets and reticulocyte-rich subpopulations of normal and sickle erythrocytes; c) the sulfate glycolipids, which bind thrombospondin, von Willebrand factor multimer and laminin [2, 42, 43]; d) the Lutheran blood group proteins (BCAM/LU), which expression is increased in red cells from SCD patients that bind to a5 subunit of laminin, a component of extracellular subendothelial matrix [44, 45]; e) the ICAM-4 (Landstein-Weiner blood group glycoprotein- LW), which binds aVb3 integrin receptors on endothelial cells [46-49]; and f) the exposure of phosphatydyl-serine (PS), detectable in a subpopulation of sickle red cells, which participates in sickle cell adhesion to activated endothelium [50-54] (Figure 2). Ex vivo and in vitro experimental studies have shown that thrombospondin- and von Willebrand factor-mediated interaction between sickle red cells and endothelium via a Vb3 integrin might be blocked by monoclonal antibodies against aVb3 integrin receptors [42, 48, 55]. Recent study with short synthetic peptides interfering with ICAM-4 and a Vb3 integrin binding have been evaluated in ex vivo system, showing a reduction in sickle erythrocyte adhesion to activated endothelial cells allowing to consider the blocking of this adhesion pathway as possible therapeutic new strategy in treatment of acute sickle cell events [48, 55]. The binding between thrombospondin, von Willebrand factor and laminin, which mediates sickle cell-endothelial adherence, might be blocked by anionic polysaccharides such as high molecular weight dextran sulfate or chondroitin sulfate [2, 42, 43]. An additional therapeutic approach to block sickle cell adhesion to endothelial cells is heparin that might interfer with sickle cell adhesion to endothelial cells through P-selectin[56-59] or binding to TSP that can mediate the interactions between sickle erythrocytes and the vascular endothelial surface. A double blind randomized trial with tinzaparin in SCD patients during acute VOCs has documented a reduction of severit and duration of the VOCs [51, 60].
Molecules modulating inflammatory pathways involved in sickle cell-endothelial adhesion: Chronic inflammatory state has been described in SCD patients characterized by increase plasma levels of acute phase proteins, of soluble cytokines such as IL1b, IL6, TNF- a and endothelin-1 (ET-1) that are further elevated during acute VOCs. These factors participate to leukocyte chemotasis, modulate vascular tone and contribute in sickle cell related tissue damage. Thus, anti-inflammatory therapy has been propose to interfere with inflammatory storm and abnormal vascular activation [61]. Sulfasalazine is an anti-inflammatory molecule and can inhibit the transcription of nuclear factor NF-kB and interferring with endothelial cell activation [62-65]. Transgenic sickle cell mice treated with sulfasalazine show a reduction in activated circulating endothelial cells, and in VCAM-1, ICAM and E-selectin vascular wall endothelial expression. In a pilot study, the administration of sulfasalazine to sickle cell patients results in reduction in the abnormal endothelial activation [4]. Another possible strategy aimed at reducing the adhesion of sickle red cells to vascular endothelium is the inhibition of interactions between leukocytes already adherent to endothelium and sickle red cells during vaso-occlusive events [66]. Based on the in vitro evidence that immunoglobulin (Ig ) significantly reduces the binding of sickle red cells to neutrophils in transgenic sickle cell mice, the infusion of Ig in vivo was shown to inhibit the interaction between sickle red cells and leukocytes in the cremasteric venules, suggesting that Ig may act either by inhibitiing the interactions between sickle red cells and leukocytes and/or by reducing the number of adherent leukocytes [66]. In humans, three out of four sickle cell patients treated with infusion of Ig showed some beneficial effect, whereas in the fourth case the treatment accelerated a vaso-occlusive crisis [66, 67].Since Ig infusion might be related to severe side effects such as renal toxicity and thrombosis, it should be used with caution in sickle cell patients. Recent studies have shown the important role of ET-1 in acute sickle cell related VOCs in a mouse model for SCD [68, 69]. The block of ET-1 actions was obtained directly by the ET-1 receptors antagonist, Bosentan, evaluating its effects on SCD mouse kidney as target organ and indirectly by the inhibition of phosphodiesterase-4 with Rolipram in a model of early pulmonary hypertension [68, 69]. Bosentan is actually under evaluation in a phase III clinical trial in SCD patients with pulmonary hypertension [70].
The possibility of delivering oxygen directly to sickled red cells entrapped in partially obstructed vessels has also been explored. Perflubron-based fluorocarbon emulsion (PFE) decreases the peripheral vascular resistance ex vivo in the mesocaecal vasculature of rats, due more to its ability to dissolve oxygen than to its ability to modify the vascular tone. [71]
Recently, Hebbel et al have reported the beneficial effects of histone deacetylase inhibitors on vascular pathology in mouse model for sickle cell disease [72]. The Authors observed multiple therapeutic effects of these compounds as: (i) inducers of HbF; (ii) iron chelators; (iii) modulators of vascular damage and abnormal activation sickle cell related (i.e.: reduction of VCAM-1 expression).
The heme-oxygenase-1 (HO-1) connection. In different sickle cell mouse models under steady state, Belcher et al have shown up-regulation of cytoprotective gene as heme oxygenase-1 (HO-1) and a reduction of the sickle cell related organ damage when pathological mice were treated with heme oxygenase-1 products [63, 73]. In SCD patients in steady state, the gene expression profiling of circulating leukocytes has shown increased HO-1 and biliverdin reductase as well as in kidney and in circulating endothelial cells [74, 75], suggesting an induction of cell protective systems in response to chronic inflammatory stress characterizing SCD. However, the still open question is whether these cytoprotective systems are rapidly and further induced driving a continuous cellular protection during acute sickle cell vaso-occlusive crisis.
3) Nitric Oxide (NO) based therapies in sickle cell disease:
Nitric oxide (NO) is a potent vasodilator and inhibitor of vascular remodeling and also affects the multi-step cascade of events involved in leukocyte, platelet and endothelial activation. NO is generated from L-Arginine by endothelial cells via constitutive (eNOS) and inflammatory inducible nitric oxide synthases (iNOS). SCD is characterized by relative reduction in NO bioavaibility that contributes to endothelial abnormal activation and SCD organ damage. In addition chronic hemolysis leading to increase the plasma levels of hemoglobin that is an efficient NO buffer, contributes in reducing NO levels in SCD. Recent studies have focused on inhaled NO for the treatment of tissue damage in various ischaemic syndromes, including cardiovascular disease, pulmonary hypertension, and acute lung distress syndromes. The possible therapeutic role of inhaled NO has been studied in different animal models of lung injury induced by ischaemia/reperfusion. Inhaled NO prevents leukocyte migration and reduces the permeability of the peripheral microvasculature. In association with surfactant, inhaled NO alleviates alveolar edema and reduces bronchoalveolar leukocyte and neutrophil infiltration in animal models of ischaemic lung injury. A placebo-controlled randomized clinical trial of inhaled NO in SCD has recently reported beneficial results in the treatment of acute vaso-occlusive crisis, although the mechanism of action remains unknown. Plasma NO metabolites are decreased in SCD patients during vaso-occlusive crisis associated with severe pain and also in acute chest syndrome [32]. A decrease in exhaled NO has been reported in sickle cell patients, suggesting a role for NO in the pathogenesis of the pulmonary complications [76]. In a transgenic mouse model of sickle cell disease, it has been shown that inhaled NO provides protection during ischaemia/reperfusion lung injury, in which endothelial NO production is reduced [77, 78]. In addition NO-donor as polynitroxy-albumine and nitroxic- albumine have been shown to be effective in reducing inflammatory state in a SCD mouse strain and to reduce the hypoxia induce lung damage in another mouse model of acute VOCs [79, 80]. Another possible therapeutic strategy for increased NO production in sickle cell disease is supplementation of L-Arginine. Morris et al showed that L-Arginine supplementation alone induces an unexpected decrease in NO metabolite production [11, 81]. In a subsequent pilot study, an increase in NO metabolites was observed when L-Arginine was co-administrated with HU, suggesting that the combination treatment may have a synergistic effect on NO production [2, 31]. A phase II trial on L-Arginine supplementation in SCD has shown no effects on NO levels and on erythrocyte features.
4) Antioxidant agents in sickle cell disease
SCD is characterized by a pro-oxidant environment due to high production of reactive oxygen species (ROS) related to increased levels of free pathological iron and heme groups associated with a reduction in antioxidant systems such as GSH [82-85]. Studies in vitro on SCD red cells have shown that iron chelation by deferipone (L1) reduce the sickle red cell membrane susceptibility to iron mediated oxidative damage [82, 86]. In vivo study on SCD patients supplemented with L-glutamate to increase GSH and glutamate levels have shown some improvement of chronic pain [83]
Conclusion
In
conclusion, the emerging picture for treatment of sickle cell disease
is that abnormalities ranging from membrane cation transport pathways
to red cell membrane proteins structure and function, or red
cell-endothelial adhesive events, might constitute new pharmacological
targets for treating sickle cell disease. Prospective therapy for SCD
need to combine molecules with different pharmacological targets in
order to increase their therapeutic efficacy and to reduce their side
effects (e.g., volume-controlling drugs and either hydroxyurea or
anti-adhesive molecules).
References
- Eaton, W. A., Hofrichter, J., Sickle cell
hemoglobin polymerization. Adv Protein Chem 1990, 40, 63-279.

- Steinberg, M. H., Management of sickle cell
disease. N Engl J Med 1999, 340, 1021-1030.

- Ballas, S. K., Smith, E. D., Red blood cell
changes
during the evolution of the sickle cell painful crisis. Blood 1992, 79,
2154-2163.

- Solovey, A. A., Solovey, A. N., Harkness,
J., Hebbel,
R. P., Modulation of endothelial cell activation in sickle cell
disease: a pilot study. Blood 2001, 97, 1937-1941.

- Hoppe, C., Klitz, W., D'Harlingue, K.,
Cheng, S., et
al., Confirmation of an association between the TNF(-308) promoter
polymorphism and stroke risk in children with sickle cell anemia.
Stroke 2007, 38, 2241-2246.

- Hebbel, R. P., Adhesive interactions of
sickle erythrocytes with endothelium. J Clin Invest 1997, 100, S83-86.

- Kuypers, F. A., Yuan, J., Lewis, R. A.,
Snyder, L. M.,
et al., Membrane phospholipid asymmetry in human thalassemia. Blood
1998, 91, 3044-3051.

- Archer, D. R., Stiles, J. K., Newman, G.
W., Quarshie,
A., et al., C-reactive protein and interleukin-6 are decreased in
transgenic sickle cell mice fed a high protein diet. J Nutr 2008, 138,
1148-1152.

- Rosenbaum, C., Peace, D., Rich, E., Van
Besien, K.,
Granulocyte colony-stimulating factor-based stem cell mobilization in
patients with sickle cell disease. Biol Blood Marrow Transplant 2008,
14, 719-723.

- Ou, J., Ou, Z., Jones, D. W., Holzhauer,
S., et al.,
L-4F, an apolipoprotein A-1 mimetic, dramatically improves vasodilation
in hypercholesterolemia and sickle cell disease. Circulation 2003, 107,
2337-2341.

- Belcher, J. D., Marker, P. H., Geiger, P.,
Girotti, A.
W., et al., Low-density lipoprotein susceptibility to oxidation and
cytotoxicity to endothelium in sickle cell anemia. J Lab Clin Med 1999,
133, 605-612.

- Charache, S., Terrin, M. L., Moore, R. D.,
Dover, G.
J., et al., Effect of hydroxyurea on the frequency of painful crises in
sickle cell anemia. Investigators of the Multicenter Study of
Hydroxyurea in Sickle Cell Anemia. N Engl J Med 1995, 332, 1317-1322.

- Steinberg, M. H., Barton, F., Castro, O.,
Pegelow, C.
H., et al., Effect of Hydroxyurea on Mortality and Morbidity in Adult
Sickle Cell Anemia: Risks and Benefits Up to 9 Years of Treatment. JAMA
2003, 289, 1645-1651.

- Saunthararajah, Y., Molokie, R., Saraf,
S., Sidhwani,
S., et al., Clinical effectiveness of decitabine in severe sickle cell
disease. Br J Haematol 2008, 141, 126-129.

- Fabry, M. E., Nagel, R. L., Heterogeneity
of red cells
in the sickler: a characteristic with practical clinical and
pathophysiological implications. Blood Cells 1982, 8, 9-15.

- De Franceschi, L., Corroche, R.,
Established and
experimental treatments for sickle cell disease. Haematologica 2004,
89, 348-356.

- De Franceschi, L., Bachir, D., Galacteros,
F.,
Tchernia, G., et al., Oral magnesium supplements reduce erythrocyte
dehydration in patients with sickle cell disease. J Clin Invest 1997,
100, 1847-1852.

- Brugnara, C., de Franceschi, L., Alper, S.
L.,
Inhibition of Ca(2+)-dependent K+ transport and cell dehydration in
sickle erythrocytes by clotrimazole and other imidazole derivatives. J
Clin Invest 1993, 92, 520-526.

- Brugnara, C., De Franceschi, L., Bennekou,
P., Alper,
S. L., Christophersen, P., Novel therapies for prevention of
erythrocyte dehydration in sickle cell anemia. Drug News Perspect 2001,
14, 208-220.

- Lew, V. L., Ortiz, O. E., Bookchin, R. M.,
Stochastic
nature and red cell population distribution of the sickling-induced
Ca2+ permeability. J Clin Invest 1997, 99, 2727-2735.

- McGoron, A. J., Joiner, C. H., Palascak,
M. B.,
Claussen, W. J., Franco, R. S., Dehydration of mature and immature
sickle red blood cells during fast oxygenation/deoxygenation cycles:
role of KCl cotransport and extracellular calcium. Blood 2000, 95,
2164-2168.

- Franco, R. S., Thompson, H., Palascak, M.,
Joiner, C.
H., The formation of transferrin receptor-positive sickle reticulocytes
with intermediate density is not determined by fetal hemoglobin
content. Blood 1997, 90, 3195-3203.

- Gardos, G., The function of calcium in the
potassium
permeability of human erythrocytes. Biochim Biophys Acta 1958, 30,
653-654.

- De Franceschi, L., Saadane, N., Trudel,
M., Alper, S.
L., et al., Treatment with oral clotrimazole blocks Ca(2+)-activated K+
transport and reverses erythrocyte dehydration in transgenic SAD mice.
A model for therapy of sickle cell disease. J Clin Invest 1994, 93,
1670-1676.

- Brugnara, C., Armsby, C. C., Sakamoto, M.,
Rifai, N.,
et al., Oral administration of clotrimazole and blockade of human
erythrocyte Ca(++)-activated K+ channel: the imidazole ring is not
required for inhibitory activity. J Pharmacol Exp Ther. 1995
Apr;273(1):266-72.

- Brugnara, C., Gee, B., Armsby, C. C.,
Kurth, S., et
al., Therapy with oral clotrimazole induces inhibition of the Gardos
channel and reduction of erythrocyte dehydration in patients with
sickle cell disease. Journal of Clinical Investigation 1996, 97,
1227-1234.

- McNaughton-Smith, G. A., Burns, J. F.,
Stocker, J. W.,
Rigdon, G. C., et al., Novel inhibitors of the Gardos channel for the
treatment of sickle cell disease. J Med Chem 2008, 51, 976-982.

- Stocker, J. W., De Franceschi, L.,
McNaughton-Smith,
G. A., Corrocher, R., et al., ICA-17043, a novel Gardos channel
blocker, prevents sickled red blood cell dehydration in vitro and in
vivo in SAD mice. Blood 2003, 101, 2412-2418.

- Ataga, K. I., DeCastro, L. M., Swerdlow, P., Saunthararajay, Y., Smith, W., Efficacy and safety of the Gardos channel inhibitor, ICA-17043, in patients with sickle cell anemia. Blood 2004, 104, 33a.
- Ataga, K. I., Smith, W. R., De Castro, L.
M.,
Swerdlow, P., et al., Efficacy and safety of the Gardos channel
blocker, senicapoc (ICA-17043), in patients with sickle cell anemia.
Blood 2008, 111, 3991-3997.

- Morris, C. R., Kato, G. J., Poljakovic,
M., Wang, X.,
et al., Dysregulated arginine metabolism, hemolysis-associated
pulmonary hypertension, and mortality in sickle cell disease. Jama
2005, 294, 81-90.

- Lopez, B. L., Kreshak, A. A., Morris, C.
R.,
Davis-Moon, L., et al., L-arginine levels are diminished in adult acute
vaso-occlusive sickle cell crisis in the emergency department. Br J
Haematol 2003, 120, 532-534.

- De Franceschi, L., Bachir, D., Galacteros,
F.,
Tchernia, G., et al., Oral magnesium pidolate: effects of long-term
administration in patients with sickle cell disease. Br J Haematol.
2000 Feb;108(2):284-9.

- Hankins, J. S., Wynn, L. W., Brugnara, C.,
Hillery, C.
A., et al., Phase I study of magnesium pidolate in combination with
hydroxycarbamide for children with sickle cell anaemia. Br J Haematol
2008, 140, 80-85.

- Solovey, A., Gui, L., Ramakrishnan, S.,
Steinberg, M.
H., Hebbel, R. P., Sickle cell anemia as a possible state of enhanced
anti-apoptotic tone: survival effect of vascular endothelial growth
factor on circulating and unanchored endothelial cells. Blood 1999, 93,
3824-3830.

- Ortiz, A., Circulating endothelial cells
in sickle cell anemia. N Engl J Med 1998, 338, 1162; author reply
1162-1163.

- Parise, L. V., Telen, M. J., Erythrocyte
adhesion in sickle cell disease. Curr Hematol Rep 2003, 2, 102-108.

- Hebbel, R. P., Vercellotti, G., Nath, K.
A., A Systems
Biology Consideration of the Vasculopathy of Sickle Cell Anemia: The
Need for Multi-Modality Chemo-Prophylaxsis. Cardiovasc Hematol Disord
Drug Targets 2009.

- Hebbel, R. P., The systems biology-based
argument for
taking a bold step in chemoprophylaxis of sickle vasculopathy. Am J
Hematol 2009, 84, 543-545.

- Kato, G. J., Hebbel, R. P., Steinberg, M.
H., Gladwin,
M. T., Vasculopathy in sickle cell disease: Biology, pathophysiology,
genetics, translational medicine, and new research directions. Am J
Hematol 2009, 84, 618-625.

- Orringer, E. P., Casella, J. F., Ataga, K.
I., Koshy,
M., et al., Purified poloxamer 188 for treatment of acute
vaso-occlusive crisis of sickle cell disease: A randomized controlled
trial. Jama 2001, 286, 2099-2106.

- Kaul, D. K., Tsai, H. M., Liu, X. D.,
Nakada, M. T.,
et al., Monoclonal antibodies to alphaVbeta3 (7E3 and LM609) inhibit
sickle red blood cell-endothelium interactions induced by
platelet-activating factor. Blood 2000, 95, 368-374.

- Barabino, G. A., Liu, X. D., Ewenstein, B.
M., Kaul,
D. K., Anionic polysaccharides inhibit adhesion of sickle erythrocytes
to the vascular endothelium and result in improved hemodynamic
behavior. Blood 1999, 93, 1422-1429.

- Hines, P. C., Zen, Q., Burney, S. N.,
Shea, D. A., et
al., Novel epinephrine and cyclic AMP-mediated activation of
BCAM/Lu-dependent sickle (SS) RBC adhesion. Blood 2003, 101, 3281-3287.

- Murphy, M. M., Zayed, M. A., Evans, A.,
Parker, C. E.,
et al., Role of Rap1 in promoting sickle red blood cell adhesion to
laminin via BCAM/LU. Blood 2005, 105, 3322-3329.

- Zennadi, R., Hines, P. C., De Castro, L.
M., Cartron,
J. P., et al., Epinephrine acts through erythroid signaling pathways to
activate sickle cell adhesion to endothelium via LW-alphavbeta3
interactions. Blood 2004, 104, 3774-3781.

- Zennadi, R., De Castro, L., Eyler, C., Xu,
K., et al.,
Role and regulation of sickle red cell interactions with other cells:
ICAM-4 and other adhesion receptors. Transfus Clin Biol 2008, 15, 23-28.

- Kaul, D. K., Liu, X. D., Zhang, X.,
Mankelow, T., et
al., Peptides based on alphaV-binding domains of erythrocyte ICAM-4
inhibit sickle red cell-endothelial interactions and vaso-occlusion in
the microcirculation. Am J Physiol Cell Physiol 2006, 291, C922-930.

- Mankelow, T. J., Spring, F. A., Parsons,
S. F., Brady,
R. L., et al., Identification of critical amino-acid residues on the
erythroid intercellular adhesion molecule-4 (ICAM-4) mediating adhesion
to alpha V integrins. Blood 2004, 103, 1503-1508.

- Sabina, R. L., Wandersee, N. J., Hillery,
C. A.,
Ca(2+)-CaM activation of AMP deaminase contributes to adenine
nucleotide dysregulation and phosphatidylserine externalization in
human sickle erythrocytes. Br J Haematol. 2009 Feb;144(3):434-45.

- Gayen Betal, S., Setty, B. N.,
Phosphatidylserine-positive erythrocytes bind to immobilized and
soluble thrombospondin-1 via its heparin-binding domain. Transl Res
2008, 152, 165-177.

- Hebbel, R. P., Adhesion of sickle red
cells to
endothelium: myths and future directions. Transfus Clin Biol 2008, 15,
14-18.

- Kuypers, F. A., Styles, L. A., The role of
secretory
phospholipase A2 in acute chest syndrome. Cell Mol Biol
(Noisy-le-grand) 2004, 50, 87-94.

- Kuypers, F. A., de Jong, K., The role of
phosphatidylserine in recognition and removal of erythrocytes. Cell Mol
Biol (Noisy-le-grand) 2004, 50, 147-158.

- Finnegan, E. M., Barabino, G. A., Liu, X.
D., Chang,
H. Y., et al., Small-molecule cyclic alpha V beta 3 antagonists inhibit
sickle red cell adhesion to vascular endothelium and vasoocclusion. Am
J Physiol Heart Circ Physiol 2007, 293, H1038-1045.

- Kato, G. J., Martyr, S., Blackwelder, W.
C., Nichols,
J. S., et al., Levels of soluble endothelium-derived adhesion molecules
in patients with sickle cell disease are associated with pulmonary
hypertension, organ dysfunction, and mortality. Br J Haematol 2005,
130, 943-953.

- Mohan, J. S., Lip, G. Y., Wright, J.,
Bareford, D.,
Blann, A. D., Plasma levels of tissue factor and soluble E-selectin in
sickle cell disease: relationship to genotype and to inflammation.
Blood Coagul Fibrinolysis 2005, 16, 209-214.

- Wood, K., Russell, J., Hebbel, R. P.,
Granger, D. N.,
Differential expression of E- and P-selectin in the microvasculature of
sickle cell transgenic mice. Microcirculation 2004, 11, 377-385.

- Blum, A., Yeganeh, S., Peleg, A., Vigder,
F., et al.,
Endothelial function in patients with sickle cell anemia during and
after sickle cell crises. J Thromb Thrombolysis 2005, 19, 83-86.

- Qari, M. H., Aljaouni, S. K., Alardawi, M.
S., Fatani,
H., et al., Reduction of painful vaso-occlusive crisis of sickle cell
anaemia by tinzaparin in a double-blind randomized trial. Thromb
Haemost 2007, 98, 392-396.

- Kaul, D. K., Liu, X. D., Choong, S.,
Belcher, J. D.,
et al., Anti-inflammatory therapy ameliorates leukocyte adhesion and
microvascular flow abnormalities in transgenic sickle mice. Am J
Physiol Heart Circ Physiol 2004, 287, H293-301.

- Bao, B., Prasad, A. S., Beck, F. W.,
Snell, D., et
al., Zinc supplementation decreases oxidative stress, incidence of
infection, and generation of inflammatory cytokines in sickle cell
disease patients. Transl Res 2008, 152, 67-80.

- Belcher, J. D., Mahaseth, H., Welch, T.
E., Vilback,
A. E., et al., Critical role of endothelial cell activation in
hypoxia-induced vasoocclusion in transgenic sickle mice. Am J Physiol
Heart Circ Physiol 2005, 288, H2715-2725.

- Arruda, M. A., Rossi, A. G., de Freitas,
M. S.,
Barja-Fidalgo, C., Graca-Souza, A. V., Heme inhibits human neutrophil
apoptosis: involvement of phosphoinositide 3-kinase, MAPK, and
NF-kappaB. J Immunol 2004, 173, 2023-2030.

- Osarogiagbon, U. R., Choong, S., Belcher,
J. D.,
Vercellotti, G. M., et al., Reperfusion injury pathophysiology in
sickle transgenic mice. Blood 2000, 96, 314-320.

- Turhan, A., Jenab, P., Bruhns, P.,
Ravetch, J. V., et
al., Intravenous immune globulin prevents venular vaso-occlusion in
sickle cell mice by inhibiting leukocyte adhesion and the interactions
between sickle erythrocytes and adherent leukocytes. Blood 2004, 103,
2397-2400.

- Chang, J., Shi, P. A., Chiang, E. Y.,
Frenette, P. S.,
Intravenous immunoglobulins reverse acute vaso-occlusive crises in
sickle cell mice through rapid inhibition of neutrophil adhesion. Blood
2008, 111, 915-923.

- Sabaa, N., de Franceschi, L., Bonnin, P.,
Castier, Y.,
et al., Endothelin receptor antagonism prevents hypoxia-induced
mortality and morbidity in a mouse model of sickle-cell disease. J Clin
Invest 2008, 118, 1924-1933.

- De Franceschi, L., Platt, O. S., Malpeli,
G., Janin,
A., et al., Protective effects of phosphodiesterase-4 (PDE-4)
inhibition in the early phase of pulmonary arterial hypertension in
transgenic sickle cell mice. FASEB J 2008, 22, 1849-1860.

- Benza, R. L., Pulmonary hypertension
associated with
sickle cell disease: pathophysiology and rationale for treatment. Lung
2008, 186, 247-254.

- Kaul, D. K., Liu, X., Nagel, R. L.,
Ameliorating
effects of fluorocarbon emulsion on sickle red blood cell-induced
obstruction in an ex vivo vasculature. Blood 2001, 98, 3128-3131.

- Hebbel,
R. P., Vercellotti, G.M, Pace, B., Solovey,
A., Kollander R., Abanou, C., Nguyen, J., Belcher, J.D., Abdulla, F.,
Osifuye, S., Eaton, J.W., Kelm, R., Slungaard, A., The HDAC inhibitors
trichostatin A and suberoylanilide hydroxamic acid exhibit multiple
modalities of benefit for the vascular pathobiology of sickle
transgenic mice.Blood. 2010 Mar 25;115(12):2483-90.

- Belcher, J. D., Mahaseth, H., Welch, T.
E., Otterbein,
L. E., et al., Heme oxygenase-1 is a modulator of inflammation and
vaso-occlusion in transgenic sickle mice. J Clin Invest 2006, 116,
808-816.

- Nath, K. A., Grande, J. P., Haggard, J.
J., Croatt, A.
J., et al., Oxidative stress and induction of heme oxygenase-1 in the
kidney in sickle cell disease. Am J Pathol 2001, 158, 893-903.

- Jison, M. L., Munson, P. J., Barb, J. J.,
Suffredini,
A. F., et al., Blood mononuclear cell gene expression profiles
characterize the oxidant, hemolytic, and inflammatory stress of sickle
cell disease. Blood 2004, 104, 270-280.

- Girgis, R. E., Qureshi, M. A., Abrams, J.,
Swerdlow,
P., Decreased exhaled nitric oxide in sickle cell disease: relationship
with chronic lung involvement. Am J Hematol 2003, 72, 177-184.

- Weiner, D. L., Hibberd, P. L., Betit, P.,
Cooper, A.
B., et al., Preliminary assessment of inhaled nitric oxide for acute
vaso-occlusive crisis in pediatric patients with sickle cell disease.
Jama 2003, 289, 1136-1142.

- de Franceschi, L., Baron, A., Scarpa, A.,
Adrie, C.,
et al., Inhaled nitric oxide protects transgenic SAD mice from sickle
cell disease-specific lung injury induced by hypoxia/reoxygenation.
Blood 2003, 102, 1087-1096.

- de Franceschi, L., Malpeli, G., Scarpa,
A., Janin, A.,
et al., Protective effects of S-nitrosoalbumin on lung injury induced
by hypoxia-reoxygenation in mouse model of sickle cell disease. Am J
Physiol Lung Cell Mol Physiol. 2006 Sep;291(3):L457-65.

- Mahaseth, H., Vercellotti, G. M., Welch,
T. E.,
Bowlin, P. R., et al., Polynitroxyl albumin inhibits inflammation and
vasoocclusion in transgenic sickle mice. J Lab Clin Med 2005, 145,
204-211.

- Morris, C. R., Morris, S. M., Jr., Hagar,
W., Van
Warmerdam, J., et al., Arginine therapy: a new treatment for pulmonary
hypertension in sickle cell disease? Am J Respir Crit Care Med 2003,
168, 63-69.

- Shalev, O., Hebbel, R. P., Extremely high
avidity
association of Fe(III) with the sickle red cell membrane. Blood 1996,
88, 349-352.

- Morris, C. R., Suh, J. H., Hagar, W.,
Larkin, S., et
al., Erythrocyte glutamine depletion, altered redox environment, and
pulmonary hypertension in sickle cell disease. Blood 2008, 111, 402-410.

- Aslan, M., Canatan, D., Modulation of
redox pathways
in neutrophils from sickle cell disease patients. Exp Hematol 2008, 36,
1535-1544.

- Reid, M., Badaloo, A., Forrester, T.,
Jahoor, F., In
vivo rates of erythrocyte glutathione synthesis in adults with sickle
cell disease.Am J Physiol Endocrinol Metab. 2006 Jul;291(1):E73-9.

- Shalev, O., Repka, T., Goldfarb, A.,
Grinberg, L., et
al., Deferiprone (L1) chelates pathologic iron deposits from membranes
of intact thalassemic and sickle red blood cells both in vitro and in
vivo. Blood 1995, 86, 2008-2013
