Rubella Associated with Hemophagocytic Syndrome. First Report in a Male and Review of the Literature
M. Koubāa1, Ch Marrakchi1, I. Māaloul1, S. Makni2, L. Berrajah3, M. Elloumi4, B. Hammami1, D. Lahiani1, T. Boudawara2 and M. Ben Jemāa1
1 Department of
Infectious Diseases, Hedi Chaker Hospital, Sfax 3029, Tunisia
2Department of Pathology, Habib Bourguiba Hospital, Sfax, Tunisia
3Department of Microbiology, Habib Bourguiba Hospital, Sfax, Tunisia
4Department of Clinic Hematology, Hedi Chaker Hospital, Sfax, Tunisia
2Department of Pathology, Habib Bourguiba Hospital, Sfax, Tunisia
3Department of Microbiology, Habib Bourguiba Hospital, Sfax, Tunisia
4Department of Clinic Hematology, Hedi Chaker Hospital, Sfax, Tunisia
Correspondence
to:
Doctor Makram Koubāa, Department of Infectious Diseases, Hedi Chaker
University Hospital, Sfax 3029, Tunisia. Tel: 0021674246906. Fax:
0021674246906. Email: makram.koubaa@gmail.com
and mounir.benjemaa@rns.tn
Published: August 9, 2012
Received: May 14, 2012
Accepted: June 27, 2012
Mediterr J Hematol Infect Dis 2012, 4(1): e2012050, DOI 10.4084/MJHID.2012.050
This article is available on PDF format at:

This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License
(http://creativecommons.org/licenses/by/2.0),
which permits
unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited
Abstract
A
22-year-old man was admitted to our hospital because of fever, skin
rash and epistaxis. Physical examination revealed fever (39.5°C),
generalized purpura, lymphadenopathy and splenomegaly. Blood tests
showed pancytopenia. Bone marrow aspiration and biopsy showed
hemophagocytosis with no evidence of malignant cells. Anti rubella IgM
antibody were positive and the IgG titers increased from 16 to 50 UI/mL
in 3 days. Therefore, he was diagnosed to have rubella-associated
hemophagocytic syndrome. We report herein the first case in a man and
the sixth case of rubella-associated hemophagocytic syndrome in the
literature by search in Pub Med till March 2012.
Introduction
Haemophagocytic syndrome (HS) is caused by a dysregulation in natural killer T-cell function, resulting in activation and proliferation of lymphocytes or histiocytes with uncontrolled haemophagocytosis and cytokine overproduction.[1] The syndrome is characterised by fever, hepatosplenomegaly, cytopenias, liver dysfunction, and hyperferritinaemia. HS can be either primary, with a genetic etiology, or secondary associated with malignancies, autoimmune diseases, or infections.[2]
Rubella or German measles is a viral infection typically characterized by rash, fever, and lymphadenopathy. The rash is usually an erythematous, discrete maculopapular exanthem that begins on the face and spreads caudally. It usually disappears within three days but may persist for eight days.
HS associated with rubella is uncommon. We report the first case of rubella virus-associated HS in a previously healthy 22-year-old man and we review all reported cases of rubella associated with HS in the literature by search in Pub Med till March 2012.
Case Presentation
A 22-year-old man was admitted to infectious diseases department with a 9-day history of fever, eruption, epistaxis and asthenia. Before admission, he had taken to a local hospital for fever and sore throat. He had treated with Cefpodoxime for 7 days. On admission, physical examination revealed fever (39.7 °C), generalized purpura and petechiae on the soft palate. There were several enlarged cervical, axillary and inguinal lymph nodes that were soft and tender. Abdominal examination revealed splenomegaly. Laboratory tests revealed the following: normocytic-normochromic anemia (hemoglobin 9.8 g/dL), white blood cell count 1700 cells/mm3 (neutrophils, 3%), platelet count 6 x109/L. Results of the liver function tests were normal. Serum ferritin level was 6220 ng/mL and fibrinogen 132 mg/dl. Bone marrow aspiration and biopsy (Figure 1) revealed hemophagocytosis with no evidence of malignant cells.
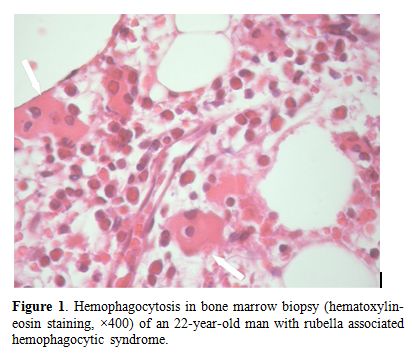
Figure 1. Hemophagocytosis in bone marrow biopsy (hematoxylin-eosin staining, ×400) of an 22-year-old man with rubella associated hemophagocytic syndrome
Anti rubella IgM antibody were positive and the IgG titers increased from 16 to 50 UI/mL in 3 days. The rubella serology was sought following the clinical and epidemiological context. Tests for common bacterial, mycobacterial, viral, fungal, auto-immune and tumoral causes of HS were negative. Therefore, he was diagnosed to have rubella-associated HS. The patient was treated by supportive measures including platelet transfusion. On discharge, physical examination was normal and her white blood cell count was 3500/mm3 (neutrophils, 42%), The hemoglobin level 10.8 g/dL and platelet count 159 x 109/L.
Discussion
We found in the literature five reports of rubella-associated HS in women.[3-7] (Table 1) But, to our knowledge this is the first report in a man.
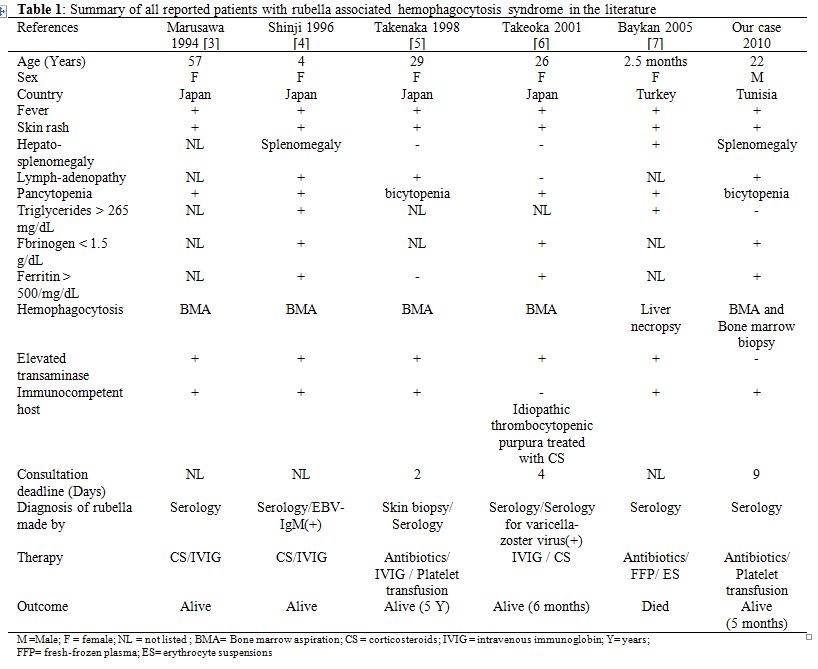
Table 1. Summary of all reported patients with rubella associated hemophagocytosis syndrome in the literature
HS can be divided into primary or genetic HS and secondary or reactive HS. Primary HS usually occurs early in life and is associated with a higher mortality rate, while secondary HS occurs later in life and generally carries a better prognosis.[8] Diagnosis of HS relies on specific clinical, laboratory, and histopathological findings proposed by the Histiocyte Society in 1991 and updated in 2004.[9,10] The prognosis of infection-associated HS is better than other types of secondary HS. Risdall et al. introduced the term ‘‘virus-associated hemophagocytic syndrome’’ and set down criteria for its separation from malignant histiocytosis.[11,12] The bone marrow hypoplasia may be due to the direct effect of viruses on the hemopoietic cells. The most common agents causing this syndrome are viruses, predominantly the herpes group, including Epstein-Barr virus, Herpes simplex, and Cytomegalovirus.[2] Acquired HS is mostly associated with underlying diseases such as immunodeficiency, hematologic neoplasia, or autoimmune disease. Infection-associated HS is most common in immunocompromised patients such as renal transplant or lymphoma.[11] The occurrence of HS in apparently immunocompetent patients may be explained by the basis of transient immunoparesis. There is no specific treatment for rubella. The anti-rubella vaccination represent the only way to prevent serious complications thus it should be indicated either in boys. Supportive therapy to address nutritional status, concomitant anemia, hemorrhagic complications, and secondary infections is therefore essential to optimize treatment outcomes.
Conclusion
Rubella is a benign disease. HS may be observed in rubella, if bone marrow aspiration is performed on patients with cytopenia. Treatment consists on supportive care. No specific therapy for rubella infection is available. The evolution is generally favorable.
Haemophagocytic syndrome (HS) is caused by a dysregulation in natural killer T-cell function, resulting in activation and proliferation of lymphocytes or histiocytes with uncontrolled haemophagocytosis and cytokine overproduction.[1] The syndrome is characterised by fever, hepatosplenomegaly, cytopenias, liver dysfunction, and hyperferritinaemia. HS can be either primary, with a genetic etiology, or secondary associated with malignancies, autoimmune diseases, or infections.[2]
Rubella or German measles is a viral infection typically characterized by rash, fever, and lymphadenopathy. The rash is usually an erythematous, discrete maculopapular exanthem that begins on the face and spreads caudally. It usually disappears within three days but may persist for eight days.
HS associated with rubella is uncommon. We report the first case of rubella virus-associated HS in a previously healthy 22-year-old man and we review all reported cases of rubella associated with HS in the literature by search in Pub Med till March 2012.
Case Presentation
A 22-year-old man was admitted to infectious diseases department with a 9-day history of fever, eruption, epistaxis and asthenia. Before admission, he had taken to a local hospital for fever and sore throat. He had treated with Cefpodoxime for 7 days. On admission, physical examination revealed fever (39.7 °C), generalized purpura and petechiae on the soft palate. There were several enlarged cervical, axillary and inguinal lymph nodes that were soft and tender. Abdominal examination revealed splenomegaly. Laboratory tests revealed the following: normocytic-normochromic anemia (hemoglobin 9.8 g/dL), white blood cell count 1700 cells/mm3 (neutrophils, 3%), platelet count 6 x109/L. Results of the liver function tests were normal. Serum ferritin level was 6220 ng/mL and fibrinogen 132 mg/dl. Bone marrow aspiration and biopsy (Figure 1) revealed hemophagocytosis with no evidence of malignant cells.
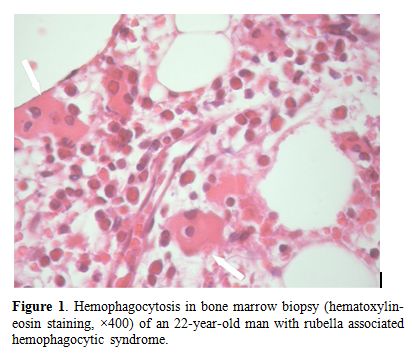
Figure 1. Hemophagocytosis in bone marrow biopsy (hematoxylin-eosin staining, ×400) of an 22-year-old man with rubella associated hemophagocytic syndrome
Anti rubella IgM antibody were positive and the IgG titers increased from 16 to 50 UI/mL in 3 days. The rubella serology was sought following the clinical and epidemiological context. Tests for common bacterial, mycobacterial, viral, fungal, auto-immune and tumoral causes of HS were negative. Therefore, he was diagnosed to have rubella-associated HS. The patient was treated by supportive measures including platelet transfusion. On discharge, physical examination was normal and her white blood cell count was 3500/mm3 (neutrophils, 42%), The hemoglobin level 10.8 g/dL and platelet count 159 x 109/L.
Discussion
We found in the literature five reports of rubella-associated HS in women.[3-7] (Table 1) But, to our knowledge this is the first report in a man.
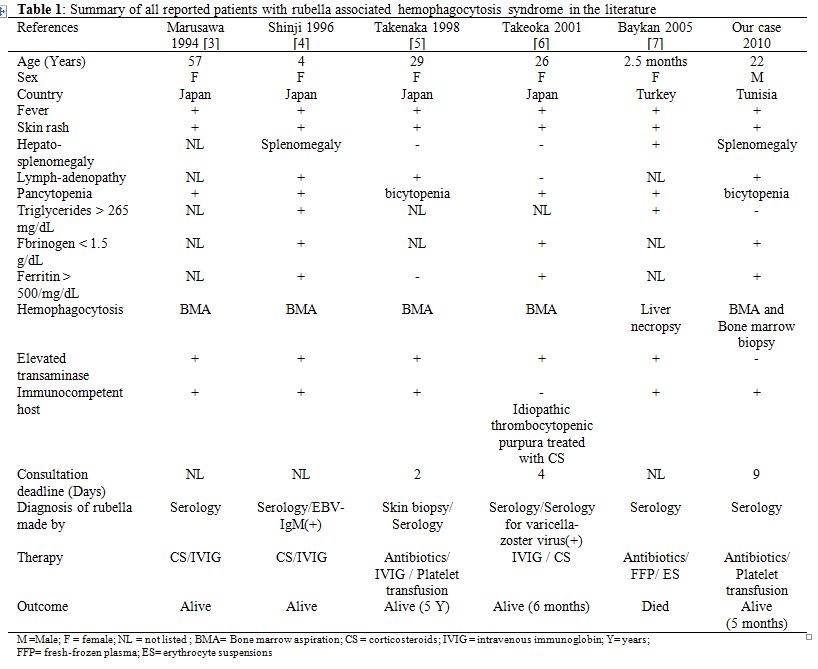
Table 1. Summary of all reported patients with rubella associated hemophagocytosis syndrome in the literature
HS can be divided into primary or genetic HS and secondary or reactive HS. Primary HS usually occurs early in life and is associated with a higher mortality rate, while secondary HS occurs later in life and generally carries a better prognosis.[8] Diagnosis of HS relies on specific clinical, laboratory, and histopathological findings proposed by the Histiocyte Society in 1991 and updated in 2004.[9,10] The prognosis of infection-associated HS is better than other types of secondary HS. Risdall et al. introduced the term ‘‘virus-associated hemophagocytic syndrome’’ and set down criteria for its separation from malignant histiocytosis.[11,12] The bone marrow hypoplasia may be due to the direct effect of viruses on the hemopoietic cells. The most common agents causing this syndrome are viruses, predominantly the herpes group, including Epstein-Barr virus, Herpes simplex, and Cytomegalovirus.[2] Acquired HS is mostly associated with underlying diseases such as immunodeficiency, hematologic neoplasia, or autoimmune disease. Infection-associated HS is most common in immunocompromised patients such as renal transplant or lymphoma.[11] The occurrence of HS in apparently immunocompetent patients may be explained by the basis of transient immunoparesis. There is no specific treatment for rubella. The anti-rubella vaccination represent the only way to prevent serious complications thus it should be indicated either in boys. Supportive therapy to address nutritional status, concomitant anemia, hemorrhagic complications, and secondary infections is therefore essential to optimize treatment outcomes.
Conclusion
Rubella is a benign disease. HS may be observed in rubella, if bone marrow aspiration is performed on patients with cytopenia. Treatment consists on supportive care. No specific therapy for rubella infection is available. The evolution is generally favorable.
References
- Janka GE. Hemophagocytic syndromes. Blood
Rev 2007;21:245-53. http://dx.doi.org/10.1016/j.blre.2007.05.001
PMid:17590250

- Rouphael NG, Talati NJ, Vaughan C,
Cunningham K, Moreira R, Gould C. Infections associated with
haemophagocytic syndrome. Lancet Infect Dis 2007;7:814-22. http://dx.doi.org/10.1016/S1473-3099(07)70290-6

- Marusawa H, Hamamoto K. [Virus-associated
hemophagocytic syndrome due to rubella virus in an adult]. Rinsho
Ketsueki 1994;35:576-80. PMid:7521404

- Shinji K, Hiroshi T, Noriyuki A, Michio K.
A Case of Hemophagocytic Syndrome Associated with Rubella and EBV
Dual-Infection Successfully Treated with High-Dose Gamma-Globulin.
日本小児血液学会雑誌 1996;10:205-209.

- Takenaka H, Kishimoto S, Ichikawa R,
Shibagaki R, Kubota Y, Yamagata N, Gotoh H, Fujita N, Yasuno H.
Virus-associated haemophagocytic syndrome caused by rubella in an
adult. Br J Dermatol 1998;139: 877-80. http://dx.doi.org/10.1046/j.1365-2133.1998.02517.x
PMid:9892958

- Takeoka Y, Hino M, Oiso N, Nishi S, Koh KR,
Yamane T, Ohta K, Nakamae H, Aoyama Y, Hirose A, Fujino H, Takubo T,
Inoue T, Tatsumi N. Virus-associated hemophagocytic syndrome due to
rubella virus and varicella-zoster virus dual infection in patient with
adult idiopathic thrombocytopenic purpura. Ann Hematol 2001;80:361-4. http://dx.doi.org/10.1007/s002770000282

- Baykan A, Akcakus M, Deniz K.
Rubella-associated hemophagocytic syndrome in an infant. J Pediatr
Hematol Oncol 2005;27:430-1. http://dx.doi.org/10.1097/01.mph.0000177427.94164.df
PMid:16096525

- Maakaroun NR, Moanna A, Jacob JT, Albrecht
H. Viral infections associated with haemophagocytic syndrome. Rev Med
Virol 2010;20:93-105. http://dx.doi.org/10.1002/rmv.638
PMid:20127750

- Henter JI, Elinder G, Ost A. Diagnostic
guidelines for hemophagocytic lymphohistiocytosis. The FHL Study Group
of the Histiocyte Society. Semin Oncol 1991;18:29-33. PMid:1992521

- Henter JI, Horne A, Arico M, Egeler RM,
Filipovich AH, Imashuku S, Ladisch S, McClain K, Webb D, Winiarski J,
Janka G. HLH-2004: Diagnostic and therapeutic guidelines for
hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer
2007;48:124-31. http://dx.doi.org/10.1002/pbc.21039

- Risdall RJ, McKenna RW, Nesbit ME, Krivit
W, Balfour HH, Jr., Simmons RL, Brunning RD. Virus-associated
hemophagocytic syndrome: a benign histiocytic proliferation distinct
from malignant histiocytosis. Cancer 1979;44:993-1002. http://dx.doi.org/10.1002/1097-0142(197909)44:3<993::AID-CNCR2820440329>3.0.CO;2-5

- Risdall RJ, Brunning RD, Hernandez JI,
Gordon DH. Bacteria-associated hemophagocytic syndrome. Cancer
1984;54:2968-72. http://dx.doi.org/10.1002/1097-0142(19841215)54:12<2968::AID-CNCR2820541226>3.0.CO;2-4
