Sickle Cell Anaemia and Malaria
Lucio Luzzatto
University of Florence, Scientific Director, Istituto Toscano Tumori. Firenze, Italy
Correspondence
to:
Prof. Lucio Luzzatto, Honorary Professor of Haematology, University of
Florence, Scientific Director, Istituto Toscano Tumori. Firenze, Italy.
E-mail: lucio.luzzatto@ittumori.it
Published: October 3, 2012
Received:August 31, 2012
Accepted: September 1, 2012
Meditter J Hematol Infect Dis 2012, 4(1): e2012065, DOI 10.4084/MJHID.2012.065
This article is available on PDF format at:

This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License
(http://creativecommons.org/licenses/by/2.0),
which permits
unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited
Abstract
Sickle
cell anaemia is a major chapter within haemolytic anaemias; at the same
time, its epidemiology is a remarkable signature of the past and
present world distribution of Plasmodium falciparum malaria. In this
brief review, in keeping with the theme of this journal, we focus on
the close and complex relationship betweeen this blood disease and this
infectious disease. On one hand, heterozygotes for the sickle gene (AS)
are relatively protected against the danger of dying of malaria, as now
firmly established through a number of clinical field studies from
different parts of Africa. In addition, experimental work is consistent
with a plausibile mechanism: namely, that in AS heterozygotes P
falciparum-infected red cells sickle preferentially and are then
removed by macrophages. On the other hand, patients who are homozygous
for the sickle gene and therefore suffer from sickle cell anaemia (SCA)
are highly susceptible to the lethal effects of malaria. The simplest
explanation of this fact is that malaria makes the anaemia of SCA more
severe; in addition, in SCA there is often hyposplenism, which reduces
clearance of parasites. From the point of view of public health it is
important that in malaria-endemic countries patients with SCA, and
particularly children, be protected from malaria by appropriate
prophylaxis.
Introduction
The history of sickle cell anaemia (SCA) lists several gold medals. First, it was for SCA that the term molecular disease was coined over half a century ago,[1] and this led to the notion of haemoglobinopathies. Second, when the structural abnormality of haemoglobin (Hb) S was pinpointed,[2] this was the first time that a single amino acid replacement in a protein was shown to cause a serious disease. Third, once the three-dimensional structure of Hb was solved[3] it became clear why Hb S had the unique characteristic of being normal when oxygenated, but abnormal when deoxygenated.[4,5] Fourth, once the globin genes were cloned, the sickle mutation was found to be in linkage disequilibrium with a polymorphic DNA site,[6] then called a restriction fragment length polymorphism (RFLP), now called a SNP: this was the seminal principle on which all of today’s genome wide association studies (GWAS) are based.
Thus, the entire field of human molecular genetics is greatly indebted to SCA; at the same time, as far as haematology is concerned, SCA is a major chapter within haemolytic anaemias.
Here we intend to discuss briefly one aspect of this condition that is eminently germane to the very name of this journal: we focus on where SCA, a blood disease, meets malaria, an infectious disease. The relationship is complex: here we will try to briefly pinpoint what we know and what we don’t yet know about this two-way relationship: malaria has influenced greatly the epidemiology of SCA, and SCA affects the clinical course of malaria.
The ‘Malaria Hypothesis’
That different persons may differ in how they respond to an infectious disease has been probably perceived for a long time. However, the first to formulate this notion in terms of Darwinian selection was J B S Haldane, who speculated that, depending on their genetic makeup, people would have a different risk of dying when they are confronted by a parasitic organism: so much so, that even if a gene offering protection against that parasite were otherwise harmful, its frequency would increase when a population was exposed to the parasite.[7] Haldane himself later hypothesized[8] that one important example could be thalassemia in the face of malaria, for several reasons. First, one type of malaria that caused by Plasmodium falciparum, is highly lethal. Second, it is estimated to have been around in many parts of the world for several thousands of years, i.e. for several hundreds of generations: thus, malaria as an agent of natural selection seemed a better candidate than an infectious disease causing occasional epidemics even if associated with high mortality (such as plague or influenza). Third, deaths from malaria take place mostly in children, i.e. before reproduction, a critical criterion for effective selection. Last but not least, Plasmodia take on different forms in the course of their life cycle, but what causes disease are the intra-erythrocytic parasites: therefore in principle it is not surprising that if red cells are in any way abnormal (as they, are, for instance, in thalassemia), this may affect the chance of success of the parasite.
Balanced Polymorphism
Many fundamental experiments in genetics have been carried out in micro-organisms, and biological selection is a good example. Growing bacteria in a culture medium containing streptomycin is a very simple and certain way to select for the few bacteria, within the culture, that already had a gene – we can call it strr – that makes them resistant to this antibiotic. If we now isolate one of the resistant bacteria we can grow up a new culture in which the entire population will be streptomycin resistant. It happens that the streptomycin-resistant bacteria do not grow quite as fast as the streptomycin-sensitive ones:[9] thus, in the presence of streptomycin the strr gene is a great advantage; in the absence of streptomycin it is a disadvantage. Since bacteria are mostly haploid (i.e. they have only one copy of each gene), each one of them either has the strr gene or it doesn’t: there is nothing in between.
Since we humans, like most animals, are diploid, we have in this respect more options. SCA is a disease of homozygotes (SS) – this is why we call the disease recessive – whereas heterozygotes (AS) are normal for most intents and purposes. The first test of Haldane’s hypothesis was carried out by A C Allison,[10] when he showed not only that the S gene was frequent in areas of high malaria transmission, but also that AS heterozygotes seemed to have less malaria. By the laws of population genetics it is to be expected that wherever the S gene is common there will be many patients suffering from SCA, a severe burden in the population; however, in the same population a much larger number of heterozygotes (see Table 1) will have the advantage of being, in first approximation, ‘malaria-resistant’. The disadvantage of homozygotes coexisting with the advantage of heterozygotes – therefore called a balanced polymorphism – had been already well characterized in Drosophila[11] and in other model systems: with the S gene it became clear that balanced polymorphism was a reality also in the human species.
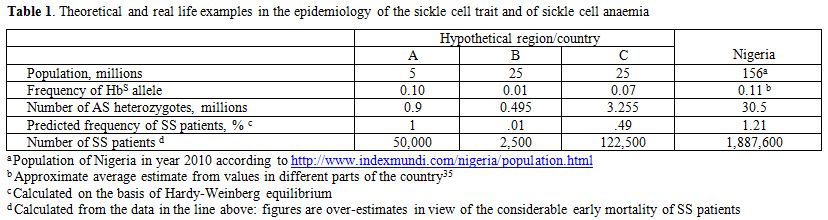
Table 1. Theoretical and real life examples in the epidemiology of the sickle cell trait and of sickle cell anaemia.
How the S Gene Affects Malaria
Allison’s seminal work has been abundantly confirmed by numerous studies on much larger population samples validated by rigorous statistical analysis;[12] and they have indicated that for AS heterozygotes the phrase ‘malaria-resistant’ ought to be regarded as shorthand for ‘relatively protected from dying of malaria’. In essence, the following points have emerged. (a) AS heterozygotes do get malaria. (b) AS heterozygotes with malaria tend to have lower numbers of parasitized red cells in their blood. (c) AS heterozygotes have a decreased incidence of the two forms of severe malaria recognized as immediately life-threatening: namely, cerebral malaria and malaria with severe anaemia. (d) Very rarely do AS heterozygotes die of malaria, even in the rare cases when they do develop cerebral malaria.[13] It stands to reason that (d) is a consequence of (c), and (c) is at least to some extent the result of (b).
These data from clinical epidemiology[14] are consistent with increased fitness of AS heterozygotes in an environment with malaria (there would be no advantage in an environment without malaria); at the same time, they tell us clearly that Hb S is not an absolute impediment to the malaria parasite. Therefore, the mechanism for the increased fitness of AS heterozygotes is not failure of invading red cells (see Table 2): rather, it must be based in something that takes place subsequently. Beet[15] first suggested that the phenomenon of sickling may be responsible; and subsequently it was shown by quantitative in vitro studies that the rate of sickling of AS red cells that had been parasitized in vivo was significantly higher than that of non-parasitized red cells within the very same blood sample.[16] It seemed reasonable to surmise and it was shown subsequently (see Figure 1) that once the parasite has triggered sickling the sickled cells would be removed by macrophages.[17]
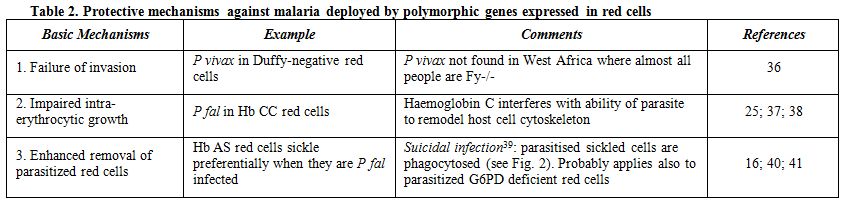
Table 2. Protective mechanisms against malaria deployed by polymorphic genes expressed in red cells.
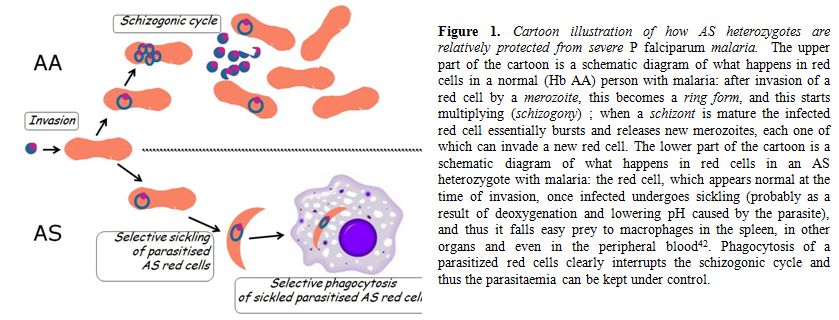
Figure 1. Cartoon illustration of how AS heterozygotes are relatively protected from severe P falciparum malaria. The upper part of the cartoon is a schematic diagram of what happens in red cells in a normal (Hb AA) person with malaria: after invasion of a red cell by a merozoite, this becomes a ring form, and this starts multiplying (schizogony); when a schizont is mature the infected red cell essentially bursts and releases new merozoites, each one of which can invade a new red cell. The lower part of the cartoon is a schematic diagram of what happens in red cells in an AS heterozygote with malaria: the red cell, which appears normal at the time of invasion, once infected undergoes sickling (probably as a result of deoxygenation and lowering pH caused by the parasite), and thus it falls easy prey to macrophages in the spleen, in other organs and even in the peripheral blood.[42] Phagocytosis of a parasitized red cells clearly interrupts the schizogonic cycle and thus the parasitaemia can be kept under control.
This mechanism is consistent with in vitro culture studies that have shown normal growth of P falciparum in AS red cells and even in SS red cells,[17,18] clearly indicating that it is not Hb S per se that hinders parasite development: it must be something downstream of the parasite cycle, such as phagocytosis of sickled cells.
In fact, although it is often stated that the mechanism of protection against malaria of AS heterozygotes is not clear, over the past 40 years there has not been any evidence contrary to the sickling-phagocytosis model; and increased phagocytosis of AS parasitized red cells has been confirmed.[19] The clinically relevant consequence of this process is to keep parasitemia relatively low in AS heterozygotes, and this has been also abundantly confirmed in many studies.[14,20-23] Of course there may be other protective mechanisms at work: for instance, it has been found that AS parasitized red cells have impaired adherence to endothelial cells, which could decrease the risk of cerebral malaria.
The impaired cytoadherence seems to result from altered display on the red cell surface of the P falciparum erythrocyte membrane protein 1 (PfEMP-1).[24] Very recently, through elegant cryoelectron tomography microscopic techniques it has been shown that PfEMP-1 display depends on remodeling by the parasite of the red cells cytoskeleton; and that this process is defective in CC and SC red cells[25] (AS red cells have not yet been tested). Protection against malaria by the S gene has been also demonstrated in a mouse model, and attributed to accelerated breakdown of haeme by haeme oxygenase[26] however, the pathophysiology of P berghei malaria in mouse is very different from that of P falciparum in humans, and therefore it is difficult to know whether this interesting phenomenon observed in the former is relevant to the latter.
Acquired immunity is a major determinant of the clinical outcome of malarial infection. Several studies have suggested that AS heterozygotes have accelerated acquisition of immunity,[27,28] although the matter is still controversial.[29] A recent study carried out in Uganda has shown that AS heterozygous children (age 1-10) are protected from (i) the establishment of blood-stage infection, (ii) the development of high densities of parasites, (iii) the progression of infection to symptomatic malaria.[30] From an analysis of data as a function of age the authors infer that both innate and acquired mechanisms of protection come into play. This confirms the notion[20] that the main advantage of AS heterozygotes in areas with heavy malaria endemicity consists in their increased probability of surviving until acquired immunity is sufficient to protect them as well as others regardless of their haemoglobin type (Figure 2).
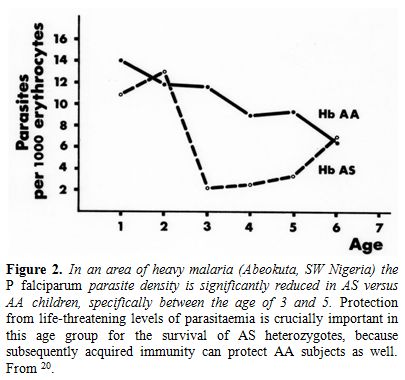
Figure 2. In an area of heavy malaria (Abeokuta, SW Nigeria) the P falciparum parasite density is significantly reduced in AS versus AA children, specifically between the age of 3 and 5. Protection from life-threatening levels of parasitaemia is crucially important in this age group for the survival of AS heterozygotes, because subsequently acquired immunity can protect AA subjects as well. From.[20]
How Malaria Affects Patients with SCA
If AS heterozygotes were protected from malaria through failure of infection, one might expect protection to be at least as effective in SS homozygotes, i.e. in patients with SCA: however, the mechanism is not failure of infection, and therefore it may not necessarily apply to homozyogotes. SCA patients, who have a prototype
congenital haemolytic anaemia, are susceptible to malaria, which is a prototype acquired haemolytic anaemia. Clinical experience has shown that, not surprisingly, this combination is highly dangerous.[31] One obvious reason is that malaria will make theanemia of SCA worse, to the point of it becoming life-threatening; another reason is that malaria, like any other acute infection, can trigger in a patient with SCA a pain crisis or a sequestration crisis. Of special note is the fact that normally the spleen plays an important role in filtering and removing parasitized red cells: but patients with SCA regularly have an impaired splenic function: often to the extent of functional asplenia, and sometimes the functional asplenia evolves to anatomical atrophy of the spleen from multiple infarcts (so-called auto-splenectomy).[32] A recent population study carried out in Kenya has shown that malaria is no more common in SCA children than in controls: however, the mortality of SCA children who had malaria was about 10 times higher than in controls.[33] We can infer that in Africa malaria contributes substantially to the early mortality of patients with SCA, which makes it imperative that they ought to be protected by life-long antimalarial prophylaxis.
Conclusion
In an era of evidence-based medicine it is still not uncommon that hypothetical propositions are stated as facts. By contrast, it is quite remarkable that the protective effect of the Hb S gene against malaria is still portrayed as a hypothesis when it is, in fact, one of the best documented examples in the human species of balanced polymorphism, in which the severe disease of homozygotes (SS or SCA) is balanced by the advantage of AS heterozygotes.
Malaria and sickle cell anaemia are still major challenges to infectious disease medicine and to haematology respectively, and both are also major public health problems. One might have hoped that what we have learnt about the of advantage of AS heterozygotes with respect to malaria would enable us to protect from malaria mortality other people as well. That this has not yet happened is disappointing but perhaps not surprising, because the key is sickling of red cells, and this is a unique phenomenon. It cannot be a straightforward task to mimic sickling by a pharmacological approach in subjects who do not have Hb S, and in a way that would act selectively only on parasitized red cells. We can still hope that human imagination will evolve novel approaches that can match the power of mutation and selection in biological evolution. In the meantime SCA remains a source of great suffering to patients, especially in those developing countries where the numbers are staggering (see Table 1). It is urgent that more is done in order to offer to these patients a better way of life: this ought to include optimal management of pain, often hydroxyurea and, especially in Africa,[34] protection against the potentially fatal threat of P falciparum malaria. If, as doctors, we have a professional obligation towards all of our patients, for those with SCA we have an added human obligation, if we consider that they carry the genetic burden that has helped human populations to survive in malaria-endemic regions of the world.
Acknowledgement
I am taking this opportunity to thank all patients with sickle cell anemia from whom I have learnt about the disease through their Hospital and Clinic visits in Ibadan, London, New York and Firenze. I also thank all my colleagues in the respective Haematology departments: particularly G J F Esan, O Sodeinde, A Olujohungbe, and the late E S Nwachuku-Jarrett.
The history of sickle cell anaemia (SCA) lists several gold medals. First, it was for SCA that the term molecular disease was coined over half a century ago,[1] and this led to the notion of haemoglobinopathies. Second, when the structural abnormality of haemoglobin (Hb) S was pinpointed,[2] this was the first time that a single amino acid replacement in a protein was shown to cause a serious disease. Third, once the three-dimensional structure of Hb was solved[3] it became clear why Hb S had the unique characteristic of being normal when oxygenated, but abnormal when deoxygenated.[4,5] Fourth, once the globin genes were cloned, the sickle mutation was found to be in linkage disequilibrium with a polymorphic DNA site,[6] then called a restriction fragment length polymorphism (RFLP), now called a SNP: this was the seminal principle on which all of today’s genome wide association studies (GWAS) are based.
Thus, the entire field of human molecular genetics is greatly indebted to SCA; at the same time, as far as haematology is concerned, SCA is a major chapter within haemolytic anaemias.
Here we intend to discuss briefly one aspect of this condition that is eminently germane to the very name of this journal: we focus on where SCA, a blood disease, meets malaria, an infectious disease. The relationship is complex: here we will try to briefly pinpoint what we know and what we don’t yet know about this two-way relationship: malaria has influenced greatly the epidemiology of SCA, and SCA affects the clinical course of malaria.
The ‘Malaria Hypothesis’
That different persons may differ in how they respond to an infectious disease has been probably perceived for a long time. However, the first to formulate this notion in terms of Darwinian selection was J B S Haldane, who speculated that, depending on their genetic makeup, people would have a different risk of dying when they are confronted by a parasitic organism: so much so, that even if a gene offering protection against that parasite were otherwise harmful, its frequency would increase when a population was exposed to the parasite.[7] Haldane himself later hypothesized[8] that one important example could be thalassemia in the face of malaria, for several reasons. First, one type of malaria that caused by Plasmodium falciparum, is highly lethal. Second, it is estimated to have been around in many parts of the world for several thousands of years, i.e. for several hundreds of generations: thus, malaria as an agent of natural selection seemed a better candidate than an infectious disease causing occasional epidemics even if associated with high mortality (such as plague or influenza). Third, deaths from malaria take place mostly in children, i.e. before reproduction, a critical criterion for effective selection. Last but not least, Plasmodia take on different forms in the course of their life cycle, but what causes disease are the intra-erythrocytic parasites: therefore in principle it is not surprising that if red cells are in any way abnormal (as they, are, for instance, in thalassemia), this may affect the chance of success of the parasite.
Balanced Polymorphism
Many fundamental experiments in genetics have been carried out in micro-organisms, and biological selection is a good example. Growing bacteria in a culture medium containing streptomycin is a very simple and certain way to select for the few bacteria, within the culture, that already had a gene – we can call it strr – that makes them resistant to this antibiotic. If we now isolate one of the resistant bacteria we can grow up a new culture in which the entire population will be streptomycin resistant. It happens that the streptomycin-resistant bacteria do not grow quite as fast as the streptomycin-sensitive ones:[9] thus, in the presence of streptomycin the strr gene is a great advantage; in the absence of streptomycin it is a disadvantage. Since bacteria are mostly haploid (i.e. they have only one copy of each gene), each one of them either has the strr gene or it doesn’t: there is nothing in between.
Since we humans, like most animals, are diploid, we have in this respect more options. SCA is a disease of homozygotes (SS) – this is why we call the disease recessive – whereas heterozygotes (AS) are normal for most intents and purposes. The first test of Haldane’s hypothesis was carried out by A C Allison,[10] when he showed not only that the S gene was frequent in areas of high malaria transmission, but also that AS heterozygotes seemed to have less malaria. By the laws of population genetics it is to be expected that wherever the S gene is common there will be many patients suffering from SCA, a severe burden in the population; however, in the same population a much larger number of heterozygotes (see Table 1) will have the advantage of being, in first approximation, ‘malaria-resistant’. The disadvantage of homozygotes coexisting with the advantage of heterozygotes – therefore called a balanced polymorphism – had been already well characterized in Drosophila[11] and in other model systems: with the S gene it became clear that balanced polymorphism was a reality also in the human species.
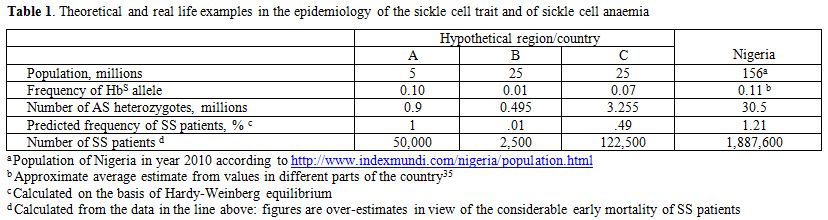
Table 1. Theoretical and real life examples in the epidemiology of the sickle cell trait and of sickle cell anaemia.
How the S Gene Affects Malaria
Allison’s seminal work has been abundantly confirmed by numerous studies on much larger population samples validated by rigorous statistical analysis;[12] and they have indicated that for AS heterozygotes the phrase ‘malaria-resistant’ ought to be regarded as shorthand for ‘relatively protected from dying of malaria’. In essence, the following points have emerged. (a) AS heterozygotes do get malaria. (b) AS heterozygotes with malaria tend to have lower numbers of parasitized red cells in their blood. (c) AS heterozygotes have a decreased incidence of the two forms of severe malaria recognized as immediately life-threatening: namely, cerebral malaria and malaria with severe anaemia. (d) Very rarely do AS heterozygotes die of malaria, even in the rare cases when they do develop cerebral malaria.[13] It stands to reason that (d) is a consequence of (c), and (c) is at least to some extent the result of (b).
These data from clinical epidemiology[14] are consistent with increased fitness of AS heterozygotes in an environment with malaria (there would be no advantage in an environment without malaria); at the same time, they tell us clearly that Hb S is not an absolute impediment to the malaria parasite. Therefore, the mechanism for the increased fitness of AS heterozygotes is not failure of invading red cells (see Table 2): rather, it must be based in something that takes place subsequently. Beet[15] first suggested that the phenomenon of sickling may be responsible; and subsequently it was shown by quantitative in vitro studies that the rate of sickling of AS red cells that had been parasitized in vivo was significantly higher than that of non-parasitized red cells within the very same blood sample.[16] It seemed reasonable to surmise and it was shown subsequently (see Figure 1) that once the parasite has triggered sickling the sickled cells would be removed by macrophages.[17]
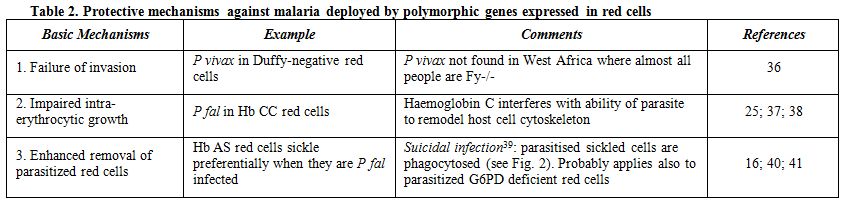
Table 2. Protective mechanisms against malaria deployed by polymorphic genes expressed in red cells.
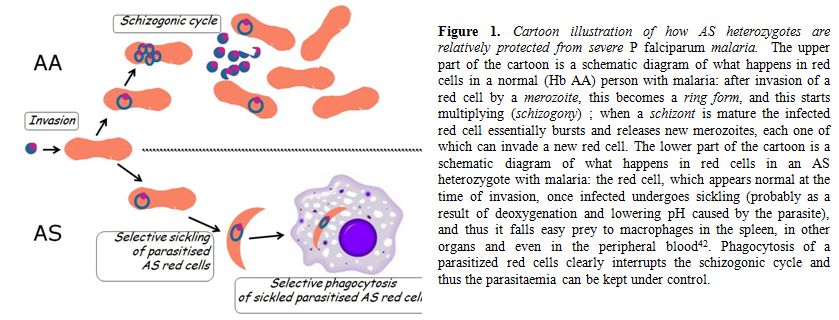
Figure 1. Cartoon illustration of how AS heterozygotes are relatively protected from severe P falciparum malaria. The upper part of the cartoon is a schematic diagram of what happens in red cells in a normal (Hb AA) person with malaria: after invasion of a red cell by a merozoite, this becomes a ring form, and this starts multiplying (schizogony); when a schizont is mature the infected red cell essentially bursts and releases new merozoites, each one of which can invade a new red cell. The lower part of the cartoon is a schematic diagram of what happens in red cells in an AS heterozygote with malaria: the red cell, which appears normal at the time of invasion, once infected undergoes sickling (probably as a result of deoxygenation and lowering pH caused by the parasite), and thus it falls easy prey to macrophages in the spleen, in other organs and even in the peripheral blood.[42] Phagocytosis of a parasitized red cells clearly interrupts the schizogonic cycle and thus the parasitaemia can be kept under control.
This mechanism is consistent with in vitro culture studies that have shown normal growth of P falciparum in AS red cells and even in SS red cells,[17,18] clearly indicating that it is not Hb S per se that hinders parasite development: it must be something downstream of the parasite cycle, such as phagocytosis of sickled cells.
In fact, although it is often stated that the mechanism of protection against malaria of AS heterozygotes is not clear, over the past 40 years there has not been any evidence contrary to the sickling-phagocytosis model; and increased phagocytosis of AS parasitized red cells has been confirmed.[19] The clinically relevant consequence of this process is to keep parasitemia relatively low in AS heterozygotes, and this has been also abundantly confirmed in many studies.[14,20-23] Of course there may be other protective mechanisms at work: for instance, it has been found that AS parasitized red cells have impaired adherence to endothelial cells, which could decrease the risk of cerebral malaria.
The impaired cytoadherence seems to result from altered display on the red cell surface of the P falciparum erythrocyte membrane protein 1 (PfEMP-1).[24] Very recently, through elegant cryoelectron tomography microscopic techniques it has been shown that PfEMP-1 display depends on remodeling by the parasite of the red cells cytoskeleton; and that this process is defective in CC and SC red cells[25] (AS red cells have not yet been tested). Protection against malaria by the S gene has been also demonstrated in a mouse model, and attributed to accelerated breakdown of haeme by haeme oxygenase[26] however, the pathophysiology of P berghei malaria in mouse is very different from that of P falciparum in humans, and therefore it is difficult to know whether this interesting phenomenon observed in the former is relevant to the latter.
Acquired immunity is a major determinant of the clinical outcome of malarial infection. Several studies have suggested that AS heterozygotes have accelerated acquisition of immunity,[27,28] although the matter is still controversial.[29] A recent study carried out in Uganda has shown that AS heterozygous children (age 1-10) are protected from (i) the establishment of blood-stage infection, (ii) the development of high densities of parasites, (iii) the progression of infection to symptomatic malaria.[30] From an analysis of data as a function of age the authors infer that both innate and acquired mechanisms of protection come into play. This confirms the notion[20] that the main advantage of AS heterozygotes in areas with heavy malaria endemicity consists in their increased probability of surviving until acquired immunity is sufficient to protect them as well as others regardless of their haemoglobin type (Figure 2).
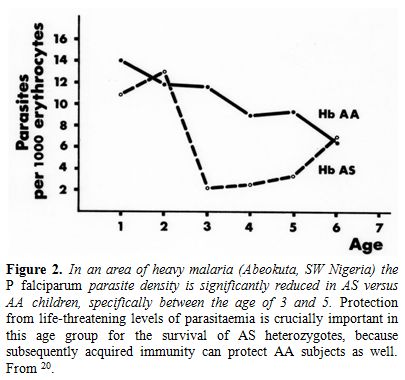
Figure 2. In an area of heavy malaria (Abeokuta, SW Nigeria) the P falciparum parasite density is significantly reduced in AS versus AA children, specifically between the age of 3 and 5. Protection from life-threatening levels of parasitaemia is crucially important in this age group for the survival of AS heterozygotes, because subsequently acquired immunity can protect AA subjects as well. From.[20]
How Malaria Affects Patients with SCA
If AS heterozygotes were protected from malaria through failure of infection, one might expect protection to be at least as effective in SS homozygotes, i.e. in patients with SCA: however, the mechanism is not failure of infection, and therefore it may not necessarily apply to homozyogotes. SCA patients, who have a prototype
congenital haemolytic anaemia, are susceptible to malaria, which is a prototype acquired haemolytic anaemia. Clinical experience has shown that, not surprisingly, this combination is highly dangerous.[31] One obvious reason is that malaria will make theanemia of SCA worse, to the point of it becoming life-threatening; another reason is that malaria, like any other acute infection, can trigger in a patient with SCA a pain crisis or a sequestration crisis. Of special note is the fact that normally the spleen plays an important role in filtering and removing parasitized red cells: but patients with SCA regularly have an impaired splenic function: often to the extent of functional asplenia, and sometimes the functional asplenia evolves to anatomical atrophy of the spleen from multiple infarcts (so-called auto-splenectomy).[32] A recent population study carried out in Kenya has shown that malaria is no more common in SCA children than in controls: however, the mortality of SCA children who had malaria was about 10 times higher than in controls.[33] We can infer that in Africa malaria contributes substantially to the early mortality of patients with SCA, which makes it imperative that they ought to be protected by life-long antimalarial prophylaxis.
Conclusion
In an era of evidence-based medicine it is still not uncommon that hypothetical propositions are stated as facts. By contrast, it is quite remarkable that the protective effect of the Hb S gene against malaria is still portrayed as a hypothesis when it is, in fact, one of the best documented examples in the human species of balanced polymorphism, in which the severe disease of homozygotes (SS or SCA) is balanced by the advantage of AS heterozygotes.
Malaria and sickle cell anaemia are still major challenges to infectious disease medicine and to haematology respectively, and both are also major public health problems. One might have hoped that what we have learnt about the of advantage of AS heterozygotes with respect to malaria would enable us to protect from malaria mortality other people as well. That this has not yet happened is disappointing but perhaps not surprising, because the key is sickling of red cells, and this is a unique phenomenon. It cannot be a straightforward task to mimic sickling by a pharmacological approach in subjects who do not have Hb S, and in a way that would act selectively only on parasitized red cells. We can still hope that human imagination will evolve novel approaches that can match the power of mutation and selection in biological evolution. In the meantime SCA remains a source of great suffering to patients, especially in those developing countries where the numbers are staggering (see Table 1). It is urgent that more is done in order to offer to these patients a better way of life: this ought to include optimal management of pain, often hydroxyurea and, especially in Africa,[34] protection against the potentially fatal threat of P falciparum malaria. If, as doctors, we have a professional obligation towards all of our patients, for those with SCA we have an added human obligation, if we consider that they carry the genetic burden that has helped human populations to survive in malaria-endemic regions of the world.
Acknowledgement
I am taking this opportunity to thank all patients with sickle cell anemia from whom I have learnt about the disease through their Hospital and Clinic visits in Ibadan, London, New York and Firenze. I also thank all my colleagues in the respective Haematology departments: particularly G J F Esan, O Sodeinde, A Olujohungbe, and the late E S Nwachuku-Jarrett.
References
- Pauling, L., Itano, H.A., Singer, S.J., and Wells, I.C. (1949). Sickle cell anemia, a molecular disease. Science 110, 543-546. http://dx.doi.org/10.1126/science.110.2865.543 PMid:15395398

- Ingram, V.M. (1956). A specific chemical
difference between the globins of normal human and sickle cell anaemia
haemoglobin. Nature 178, 792-794. http://dx.doi.org/10.1038/178792a0 PMid:13369537

- Muirhead, H., and Perutz, M.F. (1963).
Structure of Haemoglobin. A Three-Dimensional Fourier Synthesis of
Reduced Human Haemoglobin at 5-5 a Resolution. Nature 199, 633-638. http://dx.doi.org/10.1038/199633a0 PMid:14074546

- Perutz, M.F., and Lehmann, H. (1968). Molecular pathology of human hemoglobin. Nature 219, 902-909. http://dx.doi.org/10.1038/219902a0 PMid:5691676

- Wishner, B.C., Ward, K.B., Lattman, E.E.,
and Love, W.E. (1996). Crystal structure of sickle-cel deoxyhemoglobin
at 5 resolution. Journal of Molecular Biology 98, 179-191. http://dx.doi.org/10.1016/S0022-2836(75)80108-2

- Kan, Y.W., and Dozy, A.M. (1978).
Polymorphism of DNA sequence adjacent to human beta-globin structural
gene: relationship to sickle mutation. 75, 5631-5635.

- Haldane, J.B.S. (1932). The causes of evolution.(London: Longmans, Green & Co).
- Haldane, J.B.S. (1949). Disease and evolution. Ricerca Sci 19, Suppl. I, 68-76.

- Lopez-Revilla, R., and Bastarrachea, F.
(1971). A slow-growing, streptomycin resistant mutant of Escherichia
coli affected in protein synthesis and ribosomal assembly. Mol Gen
Genet 113, 99-113. PMid:4944014

- Allison, A.C. (1954). Protection afforded
by the sickle cell trait against subtertian malarial infection. British
Medical Journal i, 290-294. http://dx.doi.org/10.1136/bmj.1.4857.290 PMid:13115700 PMCid:2093356

- Freire-Maia, N. (1949). Balanced polymorphism in Drosophila montium. Evolution 3, 98. http://dx.doi.org/10.2307/2405455 PMid:18115120

- Williams, T.N. (2006). Human red blood cell polymorphisms and malaria. Curr Opin Microbiol 9, 388-394. http://dx.doi.org/10.1016/j.mib.2006.06.009 PMid:16815736

- Olumese, P.E., Adeyemo, A.A., Ademowo,
O.G., Gbadegesin, R.A., Sodeinde, O., and Walker, O. (1997). The
clinical manifestations of cerebral malaria among Nigerian children
with the sickle cell trait. Annals of Tropical Paediatrics 17, 141-145.
PMid:9230977

- Taylor, S.M., Parobek, C.M., and
Fairhurst, R.M. (2012). Haemoglobinopathies and the clinical
epidemiology of malaria: a systematic review and meta-analysis. Lancet
Infect Dis 12, 457-468. http://dx.doi.org/10.1016/S1473-3099(12)70055-5

- Beet,
E.A. (1946). Sickle cell disease in the Balovale District of Northern
Rhodesia. East Afr Med J 23, 75-86. PMid:21027890

- Luzzatto, L., Nwachuku-Jarrett, E.S., and
Reddy, S. (1970). Increased sickling of parasitised erythrocytes as
mechanism of resistance against malaria in the sickle-cell trait.
Lancet i, 319-321. http://dx.doi.org/10.1016/S0140-6736(70)90700-2

- Luzzatto, L., and Pinching, A.J. (1990).
Commentary to R Nagel - Innate Resistance to Malaria: The
Intraerythrocytic Cycle. Blood Cells 16, 340-347.

- Friedman, M.J. (1978). Erythrocytic mechanism of sickle cell resistance to malaria. Proc Natl Acad Sci USA 75, 1994-1997. http://dx.doi.org/10.1073/pnas.75.4.1994

- Ayi, K., Turrini, F., Piga, A., and Arese,
P. (2004). Enhanced phagocytosis of ring-parasitized mutant
erythrocytes: a common mechanism that may explain protection against
falciparum malaria in sickle trait and beta-thalassemia trait. Blood
104, 3364-3371. http://dx.doi.org/10.1182/blood-2003-11-3820 PMid:15280204

- Guggenmoos-Holzmann, I., Bienzle, U., and
Luzzatto, L. (1981). Plasmodium falciparum malaria and human red cells.
II. Red cell genetic traits and resistance against malaria. 10, 16-22.

- Aidoo, M., Terlouw, D.J., Kolczak, M.S.,
McElroy, P.D., ter Kuile, F.O., Kariuki, S., Nahlen, B.L., Lal, A.A.,
and Udhayakumar, V. (2002). Protective effects of the sickle cell gene
against malaria morbidity and mortality. Lancet 359, 1311-1312. http://dx.doi.org/10.1016/S0140-6736(02)08273-9

- Danquah, I., Ziniel, P., Eggelte, T.A.,
Ehrhardt, S., and Mockenhaupt, F.P. (2010). Influence of haemoglobins S
and C on predominantly asymptomatic Plasmodium infections in northern
Ghana. Trans R Soc Trop Med Hyg 104, 713-719. http://dx.doi.org/10.1016/j.trstmh.2010.08.001 PMid:20800861

- Kreuels, B., Kreuzberg, C., Kobbe, R.,
Ayim-Akonor, M., Apiah-Thompson, P., Thompson, B., Ehmen, C., Adjei,
S., Langefeld, I., Adjei, O., et al. (2010). Differing effects of HbS
and HbC traits on uncomplicated falciparum malaria, anemia, and child
growth. Blood 115, 4551-4558. http://dx.doi.org/10.1182/blood-2009-09-241844 PMid:20231425

- Cholera, R., Brittain, N.J., Gillrie,
M.R., Lopera-Mesa, T.M., Diakite, S.A., Arie, T., Krause, M.A., Guindo,
A., Tubman, A., Fujioka, H., et al. (2008). Impaired cytoadherence of
Plasmodium falciparum-infected erythrocytes containing sickle
hemoglobin. Proc Natl Acad Sci U S A 105, 991-996. http://dx.doi.org/10.1073/pnas.0711401105 PMid:18192399 PMCid:2242681

- Cyrklaff, M., Sanchez, C.P., Kilian, N.,
Bisseye, C., Simpore, J., Frischknecht, F., and Lanzer, M. (2011).
Hemoglobins S and C interfere with actin remodeling in Plasmodium
falciparum-infected erythrocytes. Science 334, 1283-1286. http://dx.doi.org/10.1126/science.1213775 PMid:22075726

- Ferreira, A., Marguti, I., Bechmann, I.,
Jeney, V., Chora, A., Palha, N.R., Rebelo, S., Henri, A., Beuzard, Y.,
and Soares, M.P. (2011). Sickle hemoglobin confers tolerance to
Plasmodium infection. Cell 145, 398-409. http://dx.doi.org/10.1016/j.cell.2011.03.049 PMid:21529713

- Williams, T.N., Mwangi, T.W., Roberts,
D.J., Alexander, N.D., Weatherall, D.J., Wambua, S., Kortok, M., Snow,
R.W., and Marsh, K. (2005). An immune basis for malaria protection by
the sickle cell trait. PLoS Med 2, e128. http://dx.doi.org/10.1371/journal.pmed.0020128 PMid:15916466 PMCid:1140945

- Verra, F., Simpore, J., Warimwe, G.M.,
Tetteh, K.K., Howard, T., Osier, F.H., Bancone, G., Avellino, P., Blot,
I., Fegan, G., et al. (2007). Haemoglobin C and S role in acquired
immunity against Plasmodium falciparum malaria. PLoS One 2, e978. http://dx.doi.org/10.1371/journal.pone.0000978 PMid:17912355 PMCid:1991593

- Tan, X., Traore, B., Kayentao, K.,
Ongoiba, A., Doumbo, S., Waisberg, M., Doumbo, O.K., Felgner, P.L.,
Fairhurst, R.M., and Crompton, P.D. (2011). Hemoglobin S and C
heterozygosity enhances neither the magnitude nor breadth of antibody
responses to a diverse array of Plasmodium falciparum antigens. J
Infect Dis 204, 1750-1761. http://dx.doi.org/10.1093/infdis/jir638 PMid:21998476

- Gong, L., Maiteki-Sebuguzi, C., Rosenthal,
P.J., Hubbard, A.E., Drakeley, C.J., Dorsey, G., and Greenhouse, B.
(2012). Evidence for both innate and acquired mechanisms of protection
from Plasmodium falciparum in children with sickle cell trait. Blood
119, 3808-3814. http://dx.doi.org/10.1182/blood-2011-08-371062 PMid:22327223

- Luzzatto, L. (1981). Sickle cell anaemia in Tropical Africa. 10, 757-784.

- Adeloye, A., Luzzatto, L., and Edington,
G.M. (1971). Severe malarial infection in a patient with sickle-cell
anaemia. British medical journal 2, 445-446. http://dx.doi.org/10.1136/bmj.2.5759.445 PMid:5576007 PMCid:1796190

- McAuley, C.F., Webb, C., Makani, J.,
Macharia, A., Uyoga, S., Opi, D.H., Ndila, C., Ngatia, A., Scott, J.A.,
Marsh, K., et al. (2010). High mortality from Plasmodium falciparum
malaria in children living with sickle cell anemia on the coast of
Kenya. Blood 116, 1663-1668. http://dx.doi.org/10.1182/blood-2010-01-265249 PMid:20530796 PMCid:3073423

- Luzzatto, L., Fasola, F., and Tshilolo, L. (2011). Haematology in Africa. Br J Haematol. http://dx.doi.org/10.1111/j.1365-2141.2011.08763.x PMid:21726208

- Piel, F.B., Patil, A.P., Howes, R.E.,
Nyangiri, O.A., Gething, P.W., Williams, T.N., Weatherall, D.J., and
Hay, S.I. (2010). Global distribution of the sickle cell gene and
geographical confirmation of the malaria hypothesis. Nat Commun 1,
104. http://dx.doi.org/10.1038/ncomms1104 PMid:21045822 PMCid:3060623

- Miller, L.H., Mason, S.J., Dvorak, J.A.,
McGinniss, M.H., and Rothman, I.K. (1975). Erythrocyte receptors for
(Plasmodium knowlesi) malaria: Duffy blood group determinants. Science
189, 561-563. http://dx.doi.org/10.1126/science.1145213 PMid:1145213

- Modiano, D., Luoni, G., Sirima, B.S.,
Simpore, J., Verra, F., Konate, A., Rastrelli, E., Olivieri, A.,
Calissano, C., Paganotti, G.M., et al. (2001). Haemoglobin C protects
against clinical Plasmodium falciparum malaria. Nature 414, 305-308. http://dx.doi.org/10.1038/35104556 PMid:11713529

- Fairhurst, R.M., Baruch, D.I., Brittain,
N.J., Ostera, G.R., Wallach, J.S., Hoang, H.L., Hayton, K., Guindo, A.,
Makobongo, M.O., Schwartz, O.M., et al. (2005). Abnormal display of
PfEMP-1 on erythrocytes carrying haemoglobin C may protect against
malaria. Nature 435, 1117-1121. http://dx.doi.org/10.1038/nature03631 PMid:15973412

- Luzzatto, L., Usanga, E.A., and Reddy, S.
(1969). Glucose 6-phosphate dehydrogenase deficient red cells:
resistance to infection by malarial parasites. Science 164, 839-842. http://dx.doi.org/10.1126/science.164.3881.839 PMid:4889647

- Luzzatto, L. (1979). Genetics of red cells and susceptibility to malaria. Blood 54, 961-976. PMid:387115

- Cappadoro, M., Giribaldi, G., O'Brien, E.,
Turrini, F., Mannu, F., Ulliers, D., Simula, G., Luzzatto, L., and
Arese, P. (1998). Early phagocytosis of glucose-6-phosphate
dehydrogenase (G6PD)-deficient erythrocytes parasitized by Plasmodium
falciparum may explain malaria protection in G6PD deficiency. Blood 92,
2527-2534. PMid:9746794

- Vernes, A. (1980). Phagocytosis of P falciparum parasitised erythrocytes by peripheral monocytes. Lancet 2, 1297-1298. http://dx.doi.org/10.1016/S0140-6736(80)92357-0
