Lenalidomide in Combination with Dexamethasone in Elderly Patients with Advanced, Relapsed or Refractory Multiple Myeloma and Renal Failure
Patrizia Tosi1, Barbara Gamberi2, Barbara Castagnari3, Anna Lia Molinari1, Paolo Savini4, Michela Ceccolini5, Monica Tani3, Anna Merli1, Manuela Imola1, Anna Maria Mianulli1, Claudia Cellini3, Simona Tomassetti1, Francesco Merli2, Pierpaolo Fattori5 and Alfonso Zaccaria5
1 Hematology Unit, Infermi Hospital, Rimini Italy
2 Hematology Unit, Department of Oncology and Advanced Thechnologies, S Maria Nuova Hospital IRCSS, Reggio Emilia Italy
3 Hematology Unit, S. Maria Delle Croci Hospital, Ravenna Italy
4 Internal Medicine Unit, Faenza Hospital Italy
5 IRCCS IRST Meldola Italy
2 Hematology Unit, Department of Oncology and Advanced Thechnologies, S Maria Nuova Hospital IRCSS, Reggio Emilia Italy
3 Hematology Unit, S. Maria Delle Croci Hospital, Ravenna Italy
4 Internal Medicine Unit, Faenza Hospital Italy
5 IRCCS IRST Meldola Italy
Correspondence
to:
Patrizia Tosi, MD. UO Ematologia, Ospedale degli Infermi, Viale
Settembrini, 2, 47900 – Rimini, Italy. Tel. + 39 0541 705987 Fax. + 39
0541 705567. E-mail: patrizia.tosi@auslrn.net
Published: June 3, 2013
Received: April 4, 2013
Accepted: May 16, 2013
Meditter J Hematol Infect Dis 2013, 5(1): e2013037, DOI 10.4084/MJHID.2013.037
This article is available on PDF format at:

This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License
(http://creativecommons.org/licenses/by/2.0),
which permits
unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited
Abstract
Salvage
therapy of elderly patients with advanced, relapsed and refractory
multiple myeloma (MM) is often limited by poor marrow reserve and
multi-organ impairment. In particular, renal failure occurs in up to
50% of such patients, and this can potentially limit the therapeutic
options. Both thalidomide and bortezomib have proven effective in these
patients, with an acceptable toxicity, while, in clinical practice,
lenalidomide is generally not considered a first-choice drug for MM
patients with renal failure as early reports showed an increased
hematological toxicity unless appropriate dose reduction is applied.
Aim of this study was a retrospective evaluation of the efficacy of the
combination Lenalidomide + Dexamethasone in a population of elderly MM
patients treated in 5 Italian Centers. The study included 20
consecutive MM patients (9 M, 11 F, median age 76.5 years) with
relapsed (N= 6) or refractory (N=13) MM and moderate to severe renal
failure, defined as creatinine clearance (Cr Cl) < 50ml/min. Four
patients were undergoing hemodyalisis at study entry. 85 % of the
patients had been previously treated with bortezomib-containing
regimens. Lenalidomide dose was adjusted according to renal function
and patients clinical conditions Median treatment duration was 16
months (1-22), therapy was interrupted after 1 21-day cycle in 2
patients. Grade III-IV neutropenia was observed in 7 patients (35%);
grade III-IV non hematological toxicity was recorded in 3 cases (28%).
A > partial response was observed in 8 patients (40%), 1 of whom
obtained a VGPR; 4 additional patients achieved a minor response.
Median response duration was 16 months (range 2-19+ months). A complete
and partial renal response was obtained in 4 and 3 patients,
respectively, all of them were responsive to Lenalidomide-dexamethasone
According to our data, LEN+DEX has shown efficacy and acceptable
toxicity in this population of elderly patients with advanced MM and
renal failure.
Introduction
Multiple myeloma (MM) is a clonal B cell malignancy characterized by a progressive clinical course, usually within 3 to 5 years from diagnosis.[1] The introduction of novel agents such as thalidomide, bortezomib or lenalidomide in the framework of high-dose or conventional chemotherapy programs has significantly improved patients' outcome and survival.[2] Patients who are refractory or those who relapse after new agents-containing regimens, however, do still represent a therapeutic challenge,[3] especially in case of advanced age and presence of co-morbidities. Renal failure occurs in approximately 20-30% of MM patients at diagnosis and in more than 50% of patients with advanced disease.[4] Salvage therapy in these patients is difficult, due to the necessity to avoid potentially nephrotoxic drugs or compounds that are excreted by the kidney and, until a few years ago, the options were limited to VAD or other high-dose dexamethasone containing regimens. Recently, however, both thalidomide[5] and bortezomib[6] have proven effective in reverting renal failure in MM patients responding to treatment, with an acceptable toxicity profile. Lenalidomide is frequently considered a second-choice drug for MM patients with renal failure as it is catabolized through the kidney[7] and its use has been initially associated with an increased hematological toxicity in patients with impaired renal function.[8-11] Recent observations, however, have pointed out that improvement of renal function can be achieved, in case a response is obtained,[10-13] and that side effects are easily manageable in case a proper dose reduction is performed.[10-15] Aim of the present study was to investigate the efficacy and the toxicity profile of lenalidomide-dexamethasone combination in a series of elderly patients with advanced, relapsed or refractory multiple myeloma and renal failure.
Patients and Methods
Patients. Twenty consecutive patients (9 male, 11 female, median age = 76.5 years, range 68-85 years) with relapsed (n= 7) or refractory (n = 13) multiple myeloma with disease-related moderate to severe chronic renal failure, defined as creatinine clearance (Cr Cl) =<50 ml/minute (Table 1) received lenalidomide as salvage treatment at 5 Italian Centers. None of the patient had a pre-existent nephropathy such as nephroangiosclerosis, diabetes or AL-amyloidosis. Previous therapy (1-3 lines) included thalidomide in 9 patients (47%), bortezomib in 17 patients (84%) and autologous stem cell transplantation in 2 patients. Thirteen patients were refractory to the last administered therapy, either to bortezomib (10 patients) or to thalidomide (2 patients) or to both bortezomib and thalidomide (one patient). Eleven patients had a more severe impairment of renal function (CrCl < 30ml/min) and four of them were undergoing hemodyalisis.
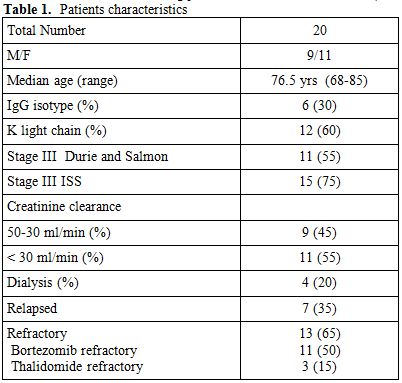
Table 1. Patients characteristics
Treatment. Lenalidomide was administered on days 1-21 of each 28-days course; dosing was chosen according to the extent of renal impairment, as previously reported.[15] Specifically, two patients with Cr Cl = 50ml/min were treated with full dose (25mg/day), 7 patients with Cr Cl < 30ml /min received 15mg every other day, patients undergoing hemodyalisis were treated at 5mg/day, the remaining patients received 10 mg/day. Dexamethasone was used at 20mg/day once a week. All the patients received antithrombotic prophylaxis with either low-molecular weight heparin or aspirin, according to pre-treatment risk of venous thromboembolism, evaluated according to Dimopoulos et al.[16] Treatment was continued until disease progression or occurrence of grade >=3 non-hematological toxicity.
Clinical and Laboratory Evaluation. Physical examination, quality of life assessment, blood cell counts, serum electrolytes, serum levels of immunoglobulins, serum creatinine, creatinine clearance and Bence-Jones proteinuria were evaluated before treatment and every other week thereafter. Toxicity and adverse events occurring during thalidomide therapy were evaluated according to the WHO grading system.
Assessment of Tumor Response. Response to lenalidomide was assessed after a minimum of 8 weeks; criteria for defining a complete response (CR), a very good partial response (VGPR) a partial response (PR) or a progressive disease (PD) were those reported by the International Myeloma Study Group[17] with the addition of minor response (MR) category, according to Kyle et al.[18]
Renal Response. Improvement in renal function, i.e. complete, partial and minor renal response, were evaluated according to recently reported criteria.[19]
Results
Response. All the patients but two completed at least 8 weeks of treatment; data were analyzed on an intention – to – treat basis. A ≥ partial response was observed in 8 patients (40%), one of whom obtained a complete response and one a very-good partial response. Four additional patients obtained a minor response, for an overall response rate of 60% (Table 2). Maximal response was achieved after a median of 8 weeks. Median response duration was 16 months (range 2-19+ months) (Figure 1A). Seven patients (35%) were refractory to treatment, even though all of them showed a stable disease lasting an average 7.5 months.
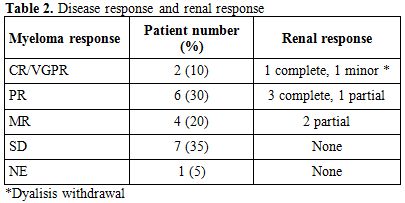
Table 2. Disease response and renal response
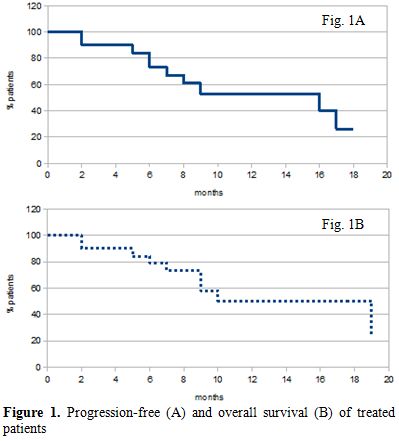
Figure 1. Progression-free (A) and overall survival (B) of treated patients
Renal Response. Recovery of a normal renal function, defined as creatinine clearance =< 60ml/min was observed in 4 out of 8 responding patients (20% of the whole population). Three patients showed an increase in CrCl from < 30 to > 30ml/min (partial response). One further responding patient who was dependent on chronic hemodyalysis showed an improvement of renal function and dyalisis was withdrawn (minor response). No improvement of renal function was observed in patients who were refractory to lenalidomide + dexamethasone therapy.
Toxicity. Toxic effects that were recorded in this series of patients were comparable to those observed in patients with a normal renal function. Neutropenia was the most commonly observed side effect (35% of the patients), although only 3 patients experienced grade ≥3 infections. No patient showed grade ≥3 thrombocytopenia. Dose reduction was necessary in 3 patients while therapy was interrupted after 1 21-day cycle in 2 patients, due to tremors and dizziness (1 patient) and stroke (1 patient), this latter patient received low-molecular heparin prophylaxis. Another patient interrupted the treatment after 5 cycles due to recurrent severe infections
Patient Status and Survival. After 8 months median follow up, 2/8 responding patients showed disease progression; 1 of them died. Five additional non responding patients have died. Overall survival averages 9 months (Figure 1B). No second primary tumor was observed.
Discussion
Recently published reports have demonstrated that lenalidomide-based drug combinations are highly effective in in pre-treated advanced MM.[20] Major concerns were risen regarding the use of the drug in patients with renal failure. Although a direct damage to the kidney has not been demonstrated in MM, worsening of renal function has been described in patients with AL amyloidosis.[21] Lenalidomide is excreted by the kidney, so that its clearance decreases in patients with renal failure, with a consequent 6-12 hours increase in plasma half-life and area-under the curve (AUC).[7] Retrospective evaluation of relapsed/refractory MM patients with some degree of renal impairment treated with full dose Lenalidomide in the context of clinical trials including mainly patients with normal renal function[10,11] confirmed the efficacy of the drug but also the occurrence of hematological toxicity, mainly thrombocytopenia that can potentially lead to more frequent treatment discontinuations. Later reports[12-14] that were mainly focused on patients with renal failure showed that a proper dose reduction can limit hematological toxicity. We further tested this latter hypothesis by analyzing the data obtained in 20 elderly patients with MM and renal insufficiency. Taking into account that the median age of our patients was higher (76.5 years) than that reported by other studies[10-11,14-15] the first, and most significant observation, is that the drug appeared to be safe, as side effects and toxicity, both hematological and non hematological, were not different or more severe than those observed in patients with a normal renal function. Even though karyotype evaluation was not carried out in our patients, their prognosis can be classified as poor (high International staging system score, high percentage of thalidomide and/or bortezomib resistance); in spite of that, 40% of the patients obtained at least a partial response, and this figure is similar to that reported in relapsed-refractory patients with a normal renal function, treated with lenalidomide-dexamethasone combination.[20] Overall, a renal response was achieved in eight patients, all of whom showing some degree of disease response. We can thus assume that renal response is strictly dependent on the attainment of a disease response that is a reduced production of light chains, and not on a direct effect on the inflammatory mechanisms that contribute to the pathogenesis of myeloma kidney as it has been described for bortezomib.[22] A bortezomib-containing regimen is generally considered the first choice therapeutic approach for patients with renal failure and MM, either newly diagnosed or relapsed/refractory. All the same however, our study and others[10-14] showed that lenalidomide-based drug combination can induce a response even in bortezomib refractory patients, thus indicating that a lenalidomide-based approach should not be overlooked, especially in elderly patients. Oral administration and, above all, the absence of toxic effects that are encountered upon thalidomide or bortezomib therapy, such as lethargy, constipation and peripheral neuropathy, render the drug convenient for long-term use, especially in elderly patients.[23] Our results, although obtained in a small series of patients, confirm that lenalidomide + dexamethasone can represent a useful therapeutic tool for elderly patients even in case of renal failure, provided an appropriate dose reduction and close monitoring of side effects.
Acknowledgements
Work supported in part by RiminiAil. The authors gratefully thank Alfredo Grattini for data collection and technical assistance.
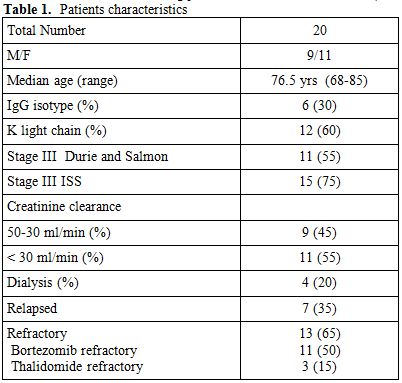
Table 1. Sampling criteria of the examined patients
Multiple myeloma (MM) is a clonal B cell malignancy characterized by a progressive clinical course, usually within 3 to 5 years from diagnosis.[1] The introduction of novel agents such as thalidomide, bortezomib or lenalidomide in the framework of high-dose or conventional chemotherapy programs has significantly improved patients' outcome and survival.[2] Patients who are refractory or those who relapse after new agents-containing regimens, however, do still represent a therapeutic challenge,[3] especially in case of advanced age and presence of co-morbidities. Renal failure occurs in approximately 20-30% of MM patients at diagnosis and in more than 50% of patients with advanced disease.[4] Salvage therapy in these patients is difficult, due to the necessity to avoid potentially nephrotoxic drugs or compounds that are excreted by the kidney and, until a few years ago, the options were limited to VAD or other high-dose dexamethasone containing regimens. Recently, however, both thalidomide[5] and bortezomib[6] have proven effective in reverting renal failure in MM patients responding to treatment, with an acceptable toxicity profile. Lenalidomide is frequently considered a second-choice drug for MM patients with renal failure as it is catabolized through the kidney[7] and its use has been initially associated with an increased hematological toxicity in patients with impaired renal function.[8-11] Recent observations, however, have pointed out that improvement of renal function can be achieved, in case a response is obtained,[10-13] and that side effects are easily manageable in case a proper dose reduction is performed.[10-15] Aim of the present study was to investigate the efficacy and the toxicity profile of lenalidomide-dexamethasone combination in a series of elderly patients with advanced, relapsed or refractory multiple myeloma and renal failure.
Patients and Methods
Patients. Twenty consecutive patients (9 male, 11 female, median age = 76.5 years, range 68-85 years) with relapsed (n= 7) or refractory (n = 13) multiple myeloma with disease-related moderate to severe chronic renal failure, defined as creatinine clearance (Cr Cl) =<50 ml/minute (Table 1) received lenalidomide as salvage treatment at 5 Italian Centers. None of the patient had a pre-existent nephropathy such as nephroangiosclerosis, diabetes or AL-amyloidosis. Previous therapy (1-3 lines) included thalidomide in 9 patients (47%), bortezomib in 17 patients (84%) and autologous stem cell transplantation in 2 patients. Thirteen patients were refractory to the last administered therapy, either to bortezomib (10 patients) or to thalidomide (2 patients) or to both bortezomib and thalidomide (one patient). Eleven patients had a more severe impairment of renal function (CrCl < 30ml/min) and four of them were undergoing hemodyalisis.
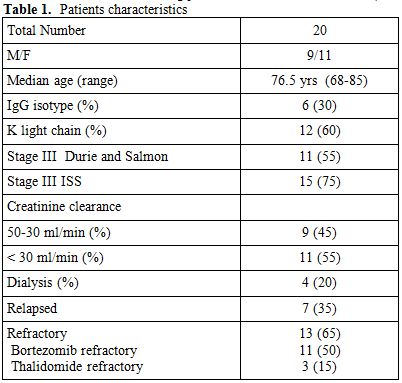
Table 1. Patients characteristics
Treatment. Lenalidomide was administered on days 1-21 of each 28-days course; dosing was chosen according to the extent of renal impairment, as previously reported.[15] Specifically, two patients with Cr Cl = 50ml/min were treated with full dose (25mg/day), 7 patients with Cr Cl < 30ml /min received 15mg every other day, patients undergoing hemodyalisis were treated at 5mg/day, the remaining patients received 10 mg/day. Dexamethasone was used at 20mg/day once a week. All the patients received antithrombotic prophylaxis with either low-molecular weight heparin or aspirin, according to pre-treatment risk of venous thromboembolism, evaluated according to Dimopoulos et al.[16] Treatment was continued until disease progression or occurrence of grade >=3 non-hematological toxicity.
Clinical and Laboratory Evaluation. Physical examination, quality of life assessment, blood cell counts, serum electrolytes, serum levels of immunoglobulins, serum creatinine, creatinine clearance and Bence-Jones proteinuria were evaluated before treatment and every other week thereafter. Toxicity and adverse events occurring during thalidomide therapy were evaluated according to the WHO grading system.
Assessment of Tumor Response. Response to lenalidomide was assessed after a minimum of 8 weeks; criteria for defining a complete response (CR), a very good partial response (VGPR) a partial response (PR) or a progressive disease (PD) were those reported by the International Myeloma Study Group[17] with the addition of minor response (MR) category, according to Kyle et al.[18]
Renal Response. Improvement in renal function, i.e. complete, partial and minor renal response, were evaluated according to recently reported criteria.[19]
Results
Response. All the patients but two completed at least 8 weeks of treatment; data were analyzed on an intention – to – treat basis. A ≥ partial response was observed in 8 patients (40%), one of whom obtained a complete response and one a very-good partial response. Four additional patients obtained a minor response, for an overall response rate of 60% (Table 2). Maximal response was achieved after a median of 8 weeks. Median response duration was 16 months (range 2-19+ months) (Figure 1A). Seven patients (35%) were refractory to treatment, even though all of them showed a stable disease lasting an average 7.5 months.
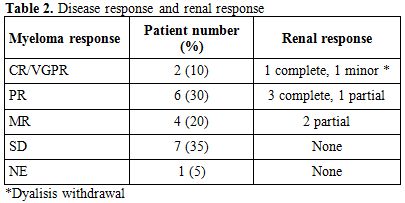
Table 2. Disease response and renal response
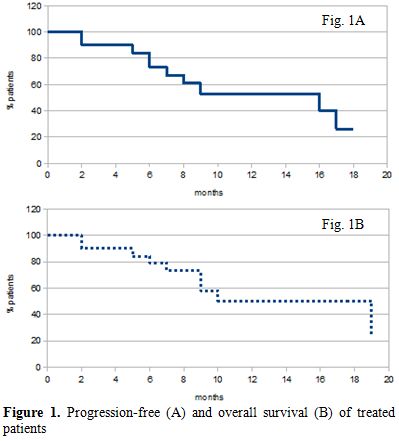
Figure 1. Progression-free (A) and overall survival (B) of treated patients
Renal Response. Recovery of a normal renal function, defined as creatinine clearance =< 60ml/min was observed in 4 out of 8 responding patients (20% of the whole population). Three patients showed an increase in CrCl from < 30 to > 30ml/min (partial response). One further responding patient who was dependent on chronic hemodyalysis showed an improvement of renal function and dyalisis was withdrawn (minor response). No improvement of renal function was observed in patients who were refractory to lenalidomide + dexamethasone therapy.
Toxicity. Toxic effects that were recorded in this series of patients were comparable to those observed in patients with a normal renal function. Neutropenia was the most commonly observed side effect (35% of the patients), although only 3 patients experienced grade ≥3 infections. No patient showed grade ≥3 thrombocytopenia. Dose reduction was necessary in 3 patients while therapy was interrupted after 1 21-day cycle in 2 patients, due to tremors and dizziness (1 patient) and stroke (1 patient), this latter patient received low-molecular heparin prophylaxis. Another patient interrupted the treatment after 5 cycles due to recurrent severe infections
Patient Status and Survival. After 8 months median follow up, 2/8 responding patients showed disease progression; 1 of them died. Five additional non responding patients have died. Overall survival averages 9 months (Figure 1B). No second primary tumor was observed.
Discussion
Recently published reports have demonstrated that lenalidomide-based drug combinations are highly effective in in pre-treated advanced MM.[20] Major concerns were risen regarding the use of the drug in patients with renal failure. Although a direct damage to the kidney has not been demonstrated in MM, worsening of renal function has been described in patients with AL amyloidosis.[21] Lenalidomide is excreted by the kidney, so that its clearance decreases in patients with renal failure, with a consequent 6-12 hours increase in plasma half-life and area-under the curve (AUC).[7] Retrospective evaluation of relapsed/refractory MM patients with some degree of renal impairment treated with full dose Lenalidomide in the context of clinical trials including mainly patients with normal renal function[10,11] confirmed the efficacy of the drug but also the occurrence of hematological toxicity, mainly thrombocytopenia that can potentially lead to more frequent treatment discontinuations. Later reports[12-14] that were mainly focused on patients with renal failure showed that a proper dose reduction can limit hematological toxicity. We further tested this latter hypothesis by analyzing the data obtained in 20 elderly patients with MM and renal insufficiency. Taking into account that the median age of our patients was higher (76.5 years) than that reported by other studies[10-11,14-15] the first, and most significant observation, is that the drug appeared to be safe, as side effects and toxicity, both hematological and non hematological, were not different or more severe than those observed in patients with a normal renal function. Even though karyotype evaluation was not carried out in our patients, their prognosis can be classified as poor (high International staging system score, high percentage of thalidomide and/or bortezomib resistance); in spite of that, 40% of the patients obtained at least a partial response, and this figure is similar to that reported in relapsed-refractory patients with a normal renal function, treated with lenalidomide-dexamethasone combination.[20] Overall, a renal response was achieved in eight patients, all of whom showing some degree of disease response. We can thus assume that renal response is strictly dependent on the attainment of a disease response that is a reduced production of light chains, and not on a direct effect on the inflammatory mechanisms that contribute to the pathogenesis of myeloma kidney as it has been described for bortezomib.[22] A bortezomib-containing regimen is generally considered the first choice therapeutic approach for patients with renal failure and MM, either newly diagnosed or relapsed/refractory. All the same however, our study and others[10-14] showed that lenalidomide-based drug combination can induce a response even in bortezomib refractory patients, thus indicating that a lenalidomide-based approach should not be overlooked, especially in elderly patients. Oral administration and, above all, the absence of toxic effects that are encountered upon thalidomide or bortezomib therapy, such as lethargy, constipation and peripheral neuropathy, render the drug convenient for long-term use, especially in elderly patients.[23] Our results, although obtained in a small series of patients, confirm that lenalidomide + dexamethasone can represent a useful therapeutic tool for elderly patients even in case of renal failure, provided an appropriate dose reduction and close monitoring of side effects.
Acknowledgements
Work supported in part by RiminiAil. The authors gratefully thank Alfredo Grattini for data collection and technical assistance.
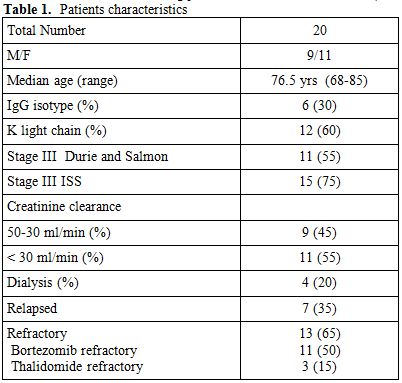
Table 1. Sampling criteria of the examined patients
References
- Kyle RA, Rajkumar SV. Multiple myeloma. N Engl J Med 2004; 351:1806-1873. http://dx.doi.org/10.1056/NEJMra041875 PMid:15509819

- Kumar SK, Rajkumar SV, Dispenzieri A Lacy
MQ, Hayman SR, Buadi FK, Zeldenrust SR, Dingli D, Russell SJ, Lust JA,
Greipp PR, Kyle RA, Gertz MA. Improved survival in multiple myeloma and
the impact of novel therapies. Blood 2008; 111:2516-2520. http://dx.doi.org/10.1182/blood-2007-10-116129 PMid:17975015 PMCid:2254544

- Kumar SK, Lee JH, Lahuerta JJ Morgan G,
Richardson PG, Crowley J, Haessler J, Feather J, Hoering A, Moreau P,
LeLeu X, Hulin C, Klein SK, Sonneveld P, Siegel D, Blade J, Goldschmidt
H, Jagannath S, San Miguel J, Orlowski R, Palumbo A, Sezer O, Rajkumar
SV, Durie BG. Risk of progression and survival in multiple myeloma
relapsing after therapy with ImiDs and bortezomib: a multicenter
international myeloma working group study. Leukemia 2012;26:149-157. http://dx.doi.org/10.1038/leu.2011.196 PMid:21799510

- Dimopoulos MA, Terpos E, Chanan-Khan A,
Leung N, Ludwig H, Jagannath S, Niesvizky R, Giralt S, Fermand JP,
Blade J, Comenzo RL, Sezer O, Palumbo A, Harousseau JL, Richardson PG,
Barlogie B, Anderson KC, Tosi P, Cavo M, Rajkumar SV, Durie BG, San
Miguel J. Renal impairment in patients with multiple myeloma: a
consensus statement on behalf of the International myeloma working
group. J Clin Oncol 2010; 28:4976-4984. http://dx.doi.org/10.1200/JCO.2010.30.8791 PMid:20956629

- Tosi P, Zamagni E, Tacchetti P Ceccolini M,
Perrone G, Brioli A, Pallotti MC, Pantani L, Petrucci A, Baccarani M,
Cavo M. Thalidomide-Dexamethasone as Induction Therapy before
Autologous Stem Cell Transplantation in Patients with Newly Diagnosed
Multiple Myeloma and Renal Insufficiency. Biol Blood Marrow Transplant
2010;16:1115-1121.

- Chanan-Khan AA, Kaufman JL, Metha
JRichardson PG, Miller KC, Lonial S, Munshi NC, Schlossman R, Tariman
J, Singhal S. Activity and safety of bortezomib in multiple myeloma
patients with advanced renal failure: a multicenter retrospective
study. Blood 2007;109:2604-2606. http://dx.doi.org/10.1182/blood-2006-09-046409 PMid:17138816

- Chen N, Lau H, Kong L Kumar G, Zeldis JB,
Knight R, Laskin OL. Pharmacokinetics of lenalidomide in subjects wiyh
various degrees of renal impairment and in subjects on hemodialysis. J
Clin Pharmacol 2007; 47:1466-1475. http://dx.doi.org/10.1177/0091270007309563 PMid:17954615

- Niesvizky R, Naib T, Christos PJ, Jayabalan
D, Furst JR, Jalbrzikowski J, Zafar F, Mark T, Lent R, Pearse RN, Ely
S, Leonard JP, Mazumdar M, Chen-Kiang S, Coleman M.
Lenalidomide-induced myelosuppression is associated with renal
dysfunction: adverse events evaluation of treatment-naďve patients
undergoing front-line lenalidomide and dexamethasone therapy. Br J
Haematol 2007;138:640-643. http://dx.doi.org/10.1111/j.1365-2141.2007.06698.x PMid:17686058

- Chen C, Reece DE, Siegel D Niesvizky R,
Boccia RV, Stadtmauer EA, Abonour R, Richardson PG, Matous J, Kumar S,
Bahlis NJ, Alsima M, Vescio R, Coutre SE, Pietronigro D, Knight RD,
Zeldis JB, Rajkumar V. Expanded safety experience with with
lenalidomide plus dexamethasone in relapsed or refractory multiple
myeloma. Br J Haematol 2009; 146:164-170. http://dx.doi.org/10.1111/j.1365-2141.2009.07728.x PMid:19545290 PMCid:2728892

- Dimopoulos M, Alegre A, Stadtmauer EA,
Goldschmidt H, Zonder JA, de Castro CM, Masliak Z, Reece D, Olesnyckyj
M, Yu Z, Weber DM. The efficacy and safety of lenalidomide plus
dexamethasone in relapsed and/or refractory multiple myeloma patients
with impaired renal function Cancer. 2010;116:3807-3814. http://dx.doi.org/10.1002/cncr.25139 PMid:20564094 PMCid:2970911

- Klein U, Neben K, Hielscher T, Heiss C, Ho
AD, Goldschmidt H. Lenalidomide in combination with dexameyhasone:
effective regimen in patients with relapsed or refractory multiple
myeloma complicated by renal impairment. Ann Hematol 2011; 90:429-43. http://dx.doi.org/10.1007/s00277-010-1080-4 PMid:20857112

- Ludwig H, Zojer N. Renal recovery with
lenalidomide in a patient with bortezomib-resistant myeloma. Nat Rev
Oncol 2010;7:289-294. http://dx.doi.org/10.1038/nrclinonc.2010.31 PMid:20351701

- de la Rubia J, Roig M, Ibanez A, Garcia I,
Vera JA, Aguilar C, Del Campo R, Gonzales N, Martinez R, Palomera L,
Picon I, Rodriguez JN, Sanz M Activity and safety of lenalidomide and
dexamethasone in patients with multiple myeloma requiring dialysis: a
Spanish multicenter retrospective study. Eur J Haematol 2010;
85:363-365. http://dx.doi.org/10.1111/j.1600-0609.2010.01500.x PMid:20662900

- Oehrlein K, Langer C, Sturm I, Ponisch W,
Hahn-Ast C, Kuhn S, Weisel KC. Successful treatment of patients with
multiple myeloma and impaired renal function with lenalidomide: results
of 4 german centers. Clin Lymphoma, myeloma and leukemia 2012;
12:191-196.

- Dimopoulos MA, Terpos E, Goldschmidt H,
Alegre A, Mark T, Niesvizky. Treatment with lenalidomide and
dexamethasone in patients with multiple myeloma and renal impairment.
Cancer Treat Rev 2012;38:1012-1019. http://dx.doi.org/10.1016/j.ctrv.2012.02.009 PMid:22609463

- Dimopoulos MA, Palumbo A, Attal M, Beksac
M, Davies FE, Delforge M, Einsele H, Hajek R, Harousseau JL, Leal Da
Costa F, Ludwig H, Mellqvist UH, Morgan GJ, San Miguel JF, Zweegman S,
Sonneveld P. Optimizing the use of lenalidomide in relapsed or
refractory multiple myeloma: consensus statement. Leukemia
2011;25749-760.

- Durie BG, Harousseau JL, Miguel JS, Bladé
J, Barlogie B, Anderson K,Gertz M, Dimopoulos M, Westin J, Sonneveld P,
Ludwig H, Gahrton G, Beksac M, Crowley J, Belch A, Boccadoro M, Cavo M,
Turesson I, Joshua D, Vesole D, Kyle R, Alexanian R, Tricot G, Attal M,
Merlini G, Powles R, Richardson P, Shimizu K, Tosi P, Morgan G,
Rajkumar SV. International uniform response criteria for multiple
myeloma Leukemia. 2006;20:1467-1473. http://dx.doi.org/10.1038/sj.leu.2404284 PMid:16855634

- Kyle RA, Rajkumar SV. Criteria for
diagnosis, staging, risk stratification and response assessment of
multiple myeloma. Leukemia 2009; 23:3-9. http://dx.doi.org/10.1038/leu.2008.291 PMid:18971951 PMCid:2627786

- Dimopoulos MA, Roussou M, Gkotzamanidou
Nikitas N, Psimenou E, Mparmaparoussi D, Matsouka C,
Spyropoulou-Vlachou M, Terpos E, Kastritis E. The role of novel agents
on the reversibility of renal impairment in newly diagnosed symptomatic
patients with multiple myeloma Leukemia 2013;27:423-429. http://dx.doi.org/10.1038/leu.2012.182 PMid:22763386

- Dimopoulos M, Spencer A, Attal M, Prince
HM, Harousseau JL, Dmoszynska A, San Miguel J, Hellman A, Facon T, Foa
R, Corso A, Masliak Z, Olesnyckyi M, Patin J, Zeldis JB, Knight RD, et
al. Lenalidomide plus dexamethasone for relapsed or refractory multiple
myeloma. N Engl J Med 2007; 357:2123-2132. http://dx.doi.org/10.1056/NEJMoa070594 PMid:18032762

- Specter R, Sanchorawala V, Seldin DC
Shelton A, Fennessey S, Finn KT, Zeldis JB, Dember LM. Kidney
disfunction during lenalidomide treatment for AL amyloidosis. Nephrol
Dial Transplant 2011; 26:881-886. http://dx.doi.org/10.1093/ndt/gfq482 PMid:20693160 PMCid:3108346

- Sarkozi R, Perco P, Hochegger K Enrich J,
Wiesinger M, Pirklbauer M, Eder S, Rudnicki M, Rosenkranz AR, Mayer B,
Schramek H. Bortezomib-induced survival signals and genes in human
proximal tubular cells. J Pharmacol Exp Ther 2008; 327:645-656. http://dx.doi.org/10.1124/jpet.108.142604 PMid:18776064

- Palumbo A, Bringhen S, Ludwig HDimopoulos
MA, Bladé J, Mateos MV, Rosi-ol L, Boccadoro M, Cavo M, Lokhorst H,
Zweegman S, Terpos E, Davies F, Driessen C, Gimsing P, Gramatzki M,
Hŕjek R, Johnsen HE, Leal Da Costa F, Sezer O, Spencer A, Beksac M,
Morgan G, Einsele H, San Miguel JF, Sonneveld P. Personalized therapy
in multiple myeloma according to patient age and vulnerability: a
report of the European Myeloma Network (EMN). Blood 2011;
118:4519-4529. http://dx.doi.org/10.1182/blood-2011-06-358812 PMid:21841166
