The Biology of Mycobacterium Tuberculosis Infection
Giovanni Delogu1, Michela Sali1 and Giovanni Fadda1
1 Istituto di Microbiologia, UniversitÓ Cattolica del Sacro Cuore, Rome.
Correspondence
to:
Prof. Giovanni Delogu, Istituto di Microbiologia, UniversitÓ Cattolica
del Sacro Cuore, Roma. Largo A. Gemelli, 8 – 00168 – Roma. Tel.
++390630154964; fax ++39063051152; gdelogu@rm.unicatt.it
Published: November 16, 2013
Received: October 28, 2013
Accepted: November 15, 2013
Meditter J Hematol Infect Dis 2013, 5(1): e2013070, DOI 10.4084/MJHID.2013.070
This article is available on PDF format at:

This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License
(http://creativecommons.org/licenses/by/2.0),
which permits
unrestricted use, distribution, and reproduction in any medium,
provided the original work is properly cited
Abstract
Tuberculosis
(TB) still poses a major threat to mankind and during the last thirty
years we have seen a recrudescence of the disease even in countries
where TB was thought to be conquered. It is common opinion that more
effective control tools such as new diagnostics, a new vaccine and new
drugs are urgently needed to control the global pandemic, though the so
far insufficient understanding of the Mycobacterium tuberculosis (Mtb)
mechanism of pathogenesis is a major obstacle for the development of
these control tools. In this review, we will summarize the recent
advancement in the understanding of Mtb biology and on the pathogenesis
of Mtb infection with emphasis on latent infection, with the change in
paradigm of the last few years where the dichotomy between latent and
active disease has been reconsidered in favor of a dynamic equilibrium
between the host and the bacilli, encompassing a continuous spectrum of
conditions that has been named TB spectrum. Implications for the
diagnosis and control of disease in certain population will also be
discussed..
Introduction
Tuberculosis (TB) is one of the ancient and deadliest disease of mankind, still posing a major health, social and economic burden at a global level and primarily in low and middle income countries.[1] The lack of an effective vaccine, the long and expensive drug regimens, the few diagnostic tools available in countries where TB is endemic and the dismantlement in several nations of the health systems and control measures that so effectively contributed to control TB throughout most of the XX century, led to the reemergence of TB as a global pandemic. The last twenty years have seen a renewed interest on TB by health authorities and governments which resulted in halving TB deaths. However, it is widely accepted that only a better understanding of the pathogenic processes associated with infection and disease will lead to the development of effective tools capable of conquering this ancient scourge. TB is one of the first and most studied infectious disease, as classically highlighted by the seminal work of R. Koch more than 100 years ago, but we have yet to answer many key questions on the mechanisms of pathogenesis and on the immunological correlates, if any, associated with protection from developing disease such as those posed by E.L. Trudeau more than a century ago.[2]
Mycobacterium tuberculosis
Evolution. TB is caused by members of the specie Mycobacterium tuberculosis complex (MTBC), which includes: Mycobacterium tuberculosis (Mtb), the etiologic agent of TB in humans; M. africanum, that causes TB in humans only in certain regions of Africa; M. bovis, M. caprae and M. pinnipedii, causing TB in wild and domesticated mammals; M. microti, that causes TB only in voles. Deciphering the ≅ 4 Mbp genome provided a new understanding of the biology of the tubercle bacillus, with the identification of new and somehow unexpected properties[3] and allowed the reconstruction of the history of Mtb as a global human infectious agent.[4] Mtb emerged as a human pathogen in Africa around 70.000 years ago and then spread out of the continent following human migrations.[5,6] It is now widely accepted that the ancients Mtb strains originated from environmental mycobacteria (smooth tubercle bacilli),[7] that can still be isolated from immunocompromised patients in certain parts of east Africa, are unable to cause chronic persistent infection in the immune-competent host and are not transmitted among humans. These ancient Mtb strains evolved, through a genetic bottleneck, so to persist in low density populations, causing disease reactivation following long period of latent infection.[8] Following domestication, humans were able to transmit the disease to animals and M. bovis emerged as a pathogen of domesticated and wild animals.[4] The introduction of agriculture, civilization and the increase in human population density in urban areas led to the selection of Mtb strains with enhanced virulence and transmissibility that are named modern Mtb strains.[9,10] The modern Mtb strains spread throughout the world causing the TB epidemics that ravaged mankind for centuries and these strains are responsible for most of the TB cases nowadays.[11]
The Bacillus. Mtb is a slow growing mycobacteria with a doubling time of 12-24 h under optimal conditions. A major feature of Mtb is the peculiar cell wall structure, that provides an exceptionally strong impermeable barrier to noxious compounds and drugs and that plays a fundamental role in virulence. The classical view of the mycobacterial cell wall structure has been revised thanks to the introduction of a new electron microscopy technique, cryo-electron tomography on vitreous section, that preserves cell wall organization by avoiding sample dehydration.[12,13] Thanks to these advancements it was shown that mycobacteria possess an outer membrane, functionally similar to what seen in gram-negative bacteria, consisting in an asymmetric lipid bilayer made of long fatty acids in the inner leaflet (mycolic acids) and of glycolipids and waxy components on the outer layer. The outer and inner membrane form a periplasmic space, with the presence of a thin layer of peptidoglycan in the innermost side covalently linked to arabinogalactan and lipoarabinomannan which in turn are bound to mycolic acids. Isoniazid and ethambutol, two of the most effective anti-TB drugs, target the synthesis of the mycolic acids and arabinogalactan, respectively, highlighting the importance of the mycobacterial cell wall in Mtb biology.
Protein secretion systems are the main virulence factors of pathogenic bacteria and in Mtb five type 7 secretion systems were identified (ESX1-5)(Figure1).[14] The best characterized of these is ESX1, which is missing in the attenuated M. bovis vaccine strain Bacille Calmette and Guerin.[15,16] ESX1 is required for the full virulence of Mtb, which uses this secretion system to translocate from the phagosome into the cytosol of infected macrophages where it may persist in a protected environment.[17-19] ESX1 secretes among many antigens, ESAT-6 and CFP-10, two small highly immunogenic proteins that form the basis of the immunological diagnosis of Mtb infection in the interferon-gamma release assays (IGRAs).[20] Since BCG lacks ESX1 and does not express ESAT-6 and CFP-10, IGRAs can be used to detect Mtb infection even in subjects previously immunized with BCG, which may not be otherwise distinguished with the classical Mantoux intradermal reaction. ESX3 is involved in the acquisition of iron and zinc by Mtb and is essential for growth also in culture.[21] ESX5 is found only in MTBC, M. marinum and M. ulcerans and it may represents a secretion systems specifically evolved to interact with a complex immune system such as that of mammals.[22] While the role and function of ESX2 and ESX4 are still debated, the elucidation of the ESX systems on TB pathogenesis is certainly one of the major advancements of the last decade in the TB field, providing a new understanding of the host-pathogen interaction and very rewarding in terms of new diagnostics and potentially capable of providing new therapeutics and vaccines in the near future.
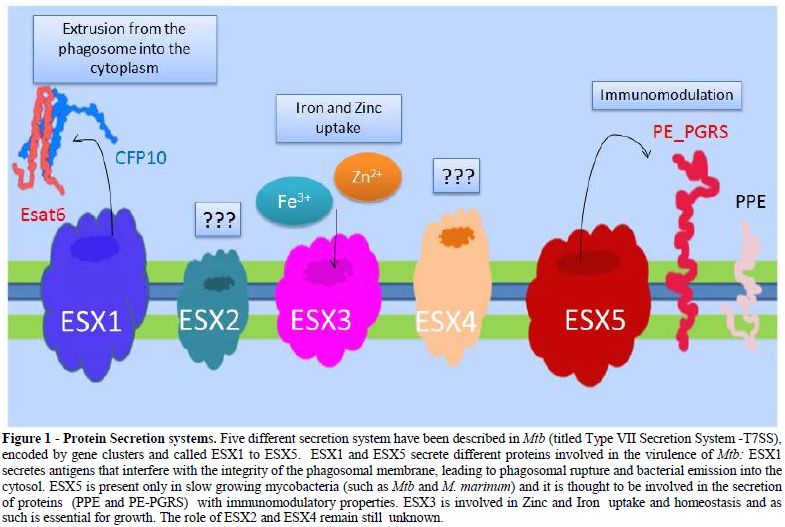
Figure 1. Protein Secretion systems. Five different secretion system have been described in Mtb (titled Type VII Secretion System -T7SS), encoded by gene clusters and called ESX1 to ESX5. ESX1 and ESX5 secrete different proteins involved in the virulence of Mtb: ESX1 secretes antigens that interfere with the integrity of the phagosomal membrane, leading to phagosomal rupture and bacterial emission into the cytosol. ESX5 is present only in slow growing mycobacteria (such as Mtb and M. marinum) and it is thought to be involved in the secretion of proteins (PPE and PE-PGRS) with immunomodulatory properties. ESX3 is involved in Zinc and Iron uptake and homeostasis and as such is essential for growth. The role of ESX2 and ESX4 remain still unknown.
The characterization of other Mtb surface constituents such as the mycobacterial adhesin HBHA[23] and PE_PGRS proteins[24,25] is starting to shed light on the molecular mechanisms involved in the interaction between the bacilli and host cells, and may lead to the development of “smart” tools capable of interfering with Mtb pathogenesis.
Another group of proteins known to play an important role in pathogenesis are those under the control of the dormancy survival regulon (Dos), which controls expression of more than 50 genes responsible for the Mtb hypoxic response.[26,27] Mtb senses the harsh environment in macrophages and granulomas, characterized by low oxygen and nutrient depletion, and responds by activating a dormant state, whereby the bacilli stops multiplying, down-regulate central metabolism and activate anaerobic metabolism, withinduction of stress proteins that provide Mtb with unique biological and immunological features.[28] These metabolically active but not replicating dormant bacilli can persist for a long time in vivo and may revert to an active state thanks to the resuscitating promoting factors (rpf), which act on the peptidoglycan to trigger a cascade of events that promotes bacterial growth.[29,30] Hence, Mtb persists in host tissues under different metabolic states, with important implications from a pathogenetic and clinical practical perspectives, sincedormant bacteria are susceptible only to certain antibiotics (pyrazinamide, rifampin and metronidazole) but resistant to other such as isoniazid.[31]
TB Pathogenesis
Mtb infection occurs when few tubercle bacilli dispersed in the air from a patient with active pulmonary TB reach the alveoli of the host. Here, Mtb is quickly phagocytized by professional alveolar macrophages that most often can kill the entering bacteria thanks to the innate immune response (Figure 2).[32] If the bacilli can survive this first line of defense, it starts actively replicating in macrophages, diffuse to nearby cells including epithelial and endothelial cells, reaching in few weeks of exponential growth a high bacterial burden.[33] During these early steps of infection, Mtb can diffuse to other organs through the lymphatics and by haematogenous dissemination where it can infect other cells.[34] Thereafter, once the adaptive immune response kicksin, migration to the site of primary infection of neutrophils, lymphocytes and other immune cells form a cellular infiltrate that later assume the typical structure of a granuloma.[35] Fibrotic components cover the granuloma that becomes calcified such that bacilli remain encapsulated inside and protected by the host immune response. This primary lesion, classically termed the Ghon complex,[36] was thought to be the “sanctuary” of Mtb during latent infection, with bacilli persisting in a dormant, non-metabolically active state, for years, decades, or most often for lifetime. In this scenario, when, during latent infection, for unknown reasons, bacilli would start replicating inside this primary lesion, active disease would ensue.[37] A major corollary of this hypothesis, with relevant pathophysiological and clinical implications, was that reactivation of TB originated from this very primary site of infection. This hypothesis was challenged since the early 20th century, when it was shown that viable and infective bacilli were found in unaffected portion of lung tissues of infected guinea pigs or human necropsy rather than from the central core of the tuberculous lesions.[37,38] Despite these early findings, only in 2000 Hernandez-Pando et al.,[39] using normal lung tissues isolated at necropsy from patients who had died for causes other than TB in a TB endemic country, were able to detect by in situ PCR Mtb DNA in non-phagocytic cells, fibroblasts and endothelial cells, clearly suggesting that in latent TB subjects Mtb bacilli can persists in tissues and cells not associated with the granuloma or the Ghon complex. Using similar experimental settings, Mtb was detected in the fat tissue surrounding several organs, residing intracellularly in adipocytes, where it can survive protected from the host immune response.[40] All these evidences suggest that during LTBI Mtb can reside in different organs, tissues and cell types, not associated with the site of primary infection and lacking any sign of the typical granulomatous lesions.
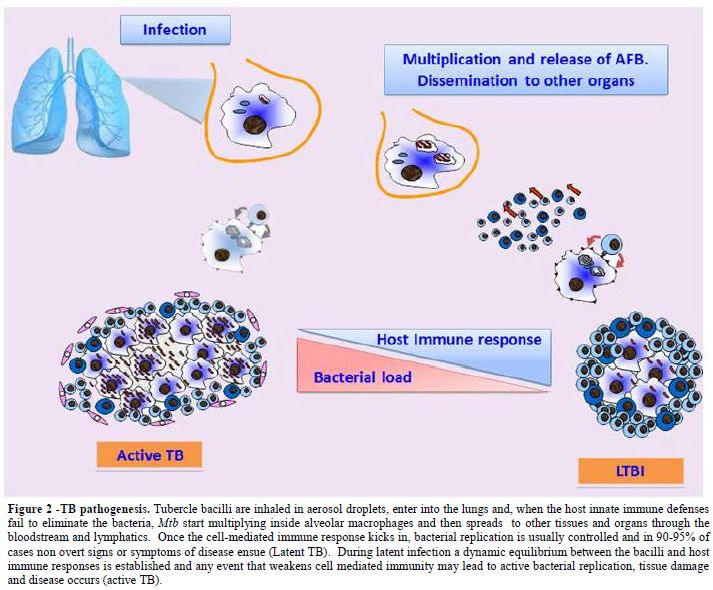
Figure 2. TB pathogenesis. Tubercle bacilli are inhaled in aerosol droplets, enter into the lungs and, when the host innate immune defenses fail to eliminate the bacteria, Mtb start multiplying inside alveolar macrophages and then spreads to other tissues and organs through the bloodstream and lymphatics. Once the cell-mediated immune response kicks in, bacterial replication is usually controlled and in 90-95% of cases non overt signs or symptoms of disease ensue (Latent TB). During latent infection a dynamic equilibrium between the bacilli and host immune responses is established and any event that weakens cell mediated immunity may lead to active bacterial replication, tissue damage and disease occurs (active TB).
Studies carried out in the non-human primate model of TB further corroborated these findings indicating that during latent infection Mtb is metabolically active and replicates in host tissues despite the lack of any clinical sign or symptom of disease.[41,42] Interestingly, in a single monkey with active TB it was possible to observe many different type of lesions, ranging from liquefied cavities with massive loads of bacilli, to necrotic or caseous hypoxic lesions with variable number of bacteria, to sterile lesions.[43] A similar scenario was observed in patients with pulmonary TB, where diverse lesions were observed simultaneously and with lesions responding differently to chemotherapy,[43] suggesting that they represent distinct Mtb subsets in different microenvironments.
Based on the new understanding of the biology of Mtb, its different metabolic states, the dynamic host immune responses occurring during infection and on the spectrum of conditions that are observed during infection, it has been proposed that during latent infection most bacilli persist in a dormant state with fewer Mtb found in an active replicating state. These replicating bacilli, named “scouts” are processed and killed by the host immune defenses and as a result they are responsible for the induction of the large number of effector/memory T cells directed against Mtb antigens that are found in the peripheral blood.[44] Hence, during latent TB dormant bacteria constantly replenish the bulk of actively replicating bacilli readily killed by thehost. When, for any reason, host immune responses fail to control these scouts, uncontrolled bacterial replication promotes diseases manifestations and active disease ensues.[45] Classical examples are highlighted by HIV infection that affects CD4 T cells that play a pivotal role in controlling Mtb replication;[46] treatment with biological therapies with anti-TNF that are known to increase the risk of developing TB disease up to 25 times in latent TB subjects as a result of the disruption of granuloma organization and depletion of certain populations of CD8 T cells known to play a role in controlling Mtb;[47,48] treatment with corticosteroids, vitamin D deficiency and any other condition affecting T cell function are also known to increase the risk of active TB in latent TB subjects, underscoring the clinical implications that any event capable of perturbing the host-pathogen dynamic equilibrium can have.
Cancer patients, including those with haematological diseases, are also at increased risk of developing TB and in these patients clinical outcomes are usually very aggressive, may present as systemic infections with a high fatality rate and diagnosis is usually delayed.[49,50] The context of the TB spectrum, with the immunological and biological implications previously discussed, clearly highlight the risk that an infection usually controlled by the host immune response with no clinical signs or symptoms, can reactivate once the subtle balance affecting the dynamic equilibrium between the host and the bacilli occurs. Hence, it is very important to deploy proper and effective diagnostic protocols capable of detecting latent infection in these high risk groups and very sensitive assays to identify active disease when TB is suspected.
TB Diagnosis
Direct diagnosis. Definitive diagnosis of TB requires the detection of Mtb from the biological sample by at least one of the current microbiological techniques: microscopical analysis, isolation in culture or molecular methods. These assays form the basis for the microbiological diagnosis of TB and the clinicians may require detection of Mtb in one or more specimens depending on the clinical symptoms, if any.[51] High sensitivity and specificity has been observed in the detection of Mtb in specimens such as sputum, bronchoalveolar lavage or induced sputum for the diagnosis of pulmonary TB.[52] The introduction of new, highly sensitive, fully automated molecular assays for the detection of Mtb has been recognized as a major achievement of the last decades,[53] though it is important to remind that molecular diagnosis should not be ordered routinely when the clinical suspicion of TB is too low.[54-56] Non-pulmonary forms of TB may be more problematic to diagnose because of the difficulties in identifying the proper specimens and the lower sensitivity of the microbiological assays in the non-pulmonary specimens, probably resulting from a lower bacterial concentration. Detection of Mtb in the urine or stools could be used to detect systemic infections and recently new assays capable of detecting mycobacterial components (lipoarabinomannan, LAM) in the urine were shown to be helpful to diagnose TB in HIV-infected subjects and immunocompromised patients, but not to diagnose pulmonary TB in immunocompetent subjects.[57,58]
Detection of Mtb in clinical specimens has been observed in HIV patients not showing any clinical sign or symptom of the disease[59] and in a recent report on the diagnosis of TB in children it was shown that ≈25% of children positive for Mtb did not show any clinical sign or symptom.[60] These results highlight the challenges associated with TB diagnosis and provide clinical evidences for the TB spectrum concepts.[43]
Immunological Diagnosis
The immunological diagnosis of TB has been historically performed by the Mantoux test or tuberculin skin test (TST) and the introduction in the last decade of the interferon-gamma release assays (IGRAs), that measure T cell responses directed against Mtb specific antigens in peripheral whole blood, has provided a new and valuable tool in the diagnosis of Mtb infection. Discussion of the immunological diagnosis of TB is beyond the scope of this review, but it is worth mentioning that TST and IGRAs are aimed at detecting Mtb infection but cannot distinguish between LTBI subjects with non signs or symptoms of disease and active TB patients.[61,62] Despite many efforts, the prognostic value of IGRAs was shown to be insufficient and while many experimental assays are being devised and tested with the attempt to improve the current RD1-based assays,[63] it is important to remind that IGRAs can be used only as an “aid” in the diagnosis of TB and cannot be used alone to rule out TB nor to make conclusive diagnosis of TB. The concept of the TB spectrum discussed in this review provides the biological and immunological framework to support this statement.
Acknowledgment
This work was funded by MIUR PRIN (project number 2009N98ST4_001) awarded to MS and GF.
Tuberculosis (TB) is one of the ancient and deadliest disease of mankind, still posing a major health, social and economic burden at a global level and primarily in low and middle income countries.[1] The lack of an effective vaccine, the long and expensive drug regimens, the few diagnostic tools available in countries where TB is endemic and the dismantlement in several nations of the health systems and control measures that so effectively contributed to control TB throughout most of the XX century, led to the reemergence of TB as a global pandemic. The last twenty years have seen a renewed interest on TB by health authorities and governments which resulted in halving TB deaths. However, it is widely accepted that only a better understanding of the pathogenic processes associated with infection and disease will lead to the development of effective tools capable of conquering this ancient scourge. TB is one of the first and most studied infectious disease, as classically highlighted by the seminal work of R. Koch more than 100 years ago, but we have yet to answer many key questions on the mechanisms of pathogenesis and on the immunological correlates, if any, associated with protection from developing disease such as those posed by E.L. Trudeau more than a century ago.[2]
Mycobacterium tuberculosis
Evolution. TB is caused by members of the specie Mycobacterium tuberculosis complex (MTBC), which includes: Mycobacterium tuberculosis (Mtb), the etiologic agent of TB in humans; M. africanum, that causes TB in humans only in certain regions of Africa; M. bovis, M. caprae and M. pinnipedii, causing TB in wild and domesticated mammals; M. microti, that causes TB only in voles. Deciphering the ≅ 4 Mbp genome provided a new understanding of the biology of the tubercle bacillus, with the identification of new and somehow unexpected properties[3] and allowed the reconstruction of the history of Mtb as a global human infectious agent.[4] Mtb emerged as a human pathogen in Africa around 70.000 years ago and then spread out of the continent following human migrations.[5,6] It is now widely accepted that the ancients Mtb strains originated from environmental mycobacteria (smooth tubercle bacilli),[7] that can still be isolated from immunocompromised patients in certain parts of east Africa, are unable to cause chronic persistent infection in the immune-competent host and are not transmitted among humans. These ancient Mtb strains evolved, through a genetic bottleneck, so to persist in low density populations, causing disease reactivation following long period of latent infection.[8] Following domestication, humans were able to transmit the disease to animals and M. bovis emerged as a pathogen of domesticated and wild animals.[4] The introduction of agriculture, civilization and the increase in human population density in urban areas led to the selection of Mtb strains with enhanced virulence and transmissibility that are named modern Mtb strains.[9,10] The modern Mtb strains spread throughout the world causing the TB epidemics that ravaged mankind for centuries and these strains are responsible for most of the TB cases nowadays.[11]
The Bacillus. Mtb is a slow growing mycobacteria with a doubling time of 12-24 h under optimal conditions. A major feature of Mtb is the peculiar cell wall structure, that provides an exceptionally strong impermeable barrier to noxious compounds and drugs and that plays a fundamental role in virulence. The classical view of the mycobacterial cell wall structure has been revised thanks to the introduction of a new electron microscopy technique, cryo-electron tomography on vitreous section, that preserves cell wall organization by avoiding sample dehydration.[12,13] Thanks to these advancements it was shown that mycobacteria possess an outer membrane, functionally similar to what seen in gram-negative bacteria, consisting in an asymmetric lipid bilayer made of long fatty acids in the inner leaflet (mycolic acids) and of glycolipids and waxy components on the outer layer. The outer and inner membrane form a periplasmic space, with the presence of a thin layer of peptidoglycan in the innermost side covalently linked to arabinogalactan and lipoarabinomannan which in turn are bound to mycolic acids. Isoniazid and ethambutol, two of the most effective anti-TB drugs, target the synthesis of the mycolic acids and arabinogalactan, respectively, highlighting the importance of the mycobacterial cell wall in Mtb biology.
Protein secretion systems are the main virulence factors of pathogenic bacteria and in Mtb five type 7 secretion systems were identified (ESX1-5)(Figure1).[14] The best characterized of these is ESX1, which is missing in the attenuated M. bovis vaccine strain Bacille Calmette and Guerin.[15,16] ESX1 is required for the full virulence of Mtb, which uses this secretion system to translocate from the phagosome into the cytosol of infected macrophages where it may persist in a protected environment.[17-19] ESX1 secretes among many antigens, ESAT-6 and CFP-10, two small highly immunogenic proteins that form the basis of the immunological diagnosis of Mtb infection in the interferon-gamma release assays (IGRAs).[20] Since BCG lacks ESX1 and does not express ESAT-6 and CFP-10, IGRAs can be used to detect Mtb infection even in subjects previously immunized with BCG, which may not be otherwise distinguished with the classical Mantoux intradermal reaction. ESX3 is involved in the acquisition of iron and zinc by Mtb and is essential for growth also in culture.[21] ESX5 is found only in MTBC, M. marinum and M. ulcerans and it may represents a secretion systems specifically evolved to interact with a complex immune system such as that of mammals.[22] While the role and function of ESX2 and ESX4 are still debated, the elucidation of the ESX systems on TB pathogenesis is certainly one of the major advancements of the last decade in the TB field, providing a new understanding of the host-pathogen interaction and very rewarding in terms of new diagnostics and potentially capable of providing new therapeutics and vaccines in the near future.
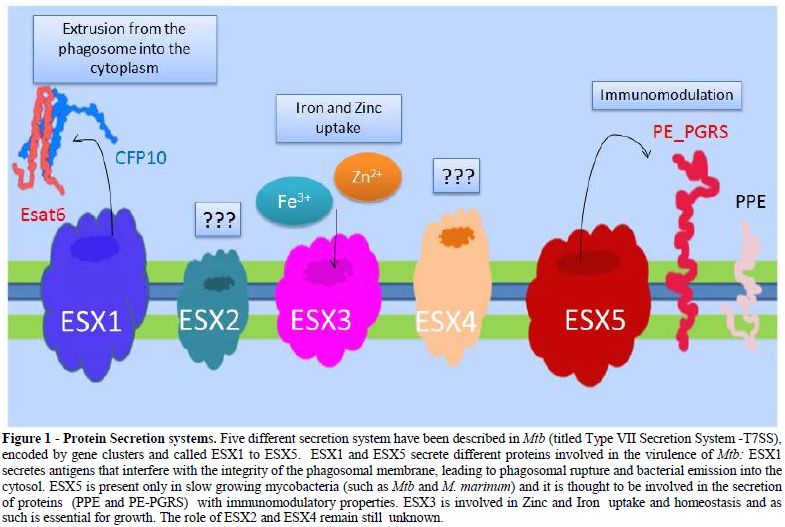
Figure 1. Protein Secretion systems. Five different secretion system have been described in Mtb (titled Type VII Secretion System -T7SS), encoded by gene clusters and called ESX1 to ESX5. ESX1 and ESX5 secrete different proteins involved in the virulence of Mtb: ESX1 secretes antigens that interfere with the integrity of the phagosomal membrane, leading to phagosomal rupture and bacterial emission into the cytosol. ESX5 is present only in slow growing mycobacteria (such as Mtb and M. marinum) and it is thought to be involved in the secretion of proteins (PPE and PE-PGRS) with immunomodulatory properties. ESX3 is involved in Zinc and Iron uptake and homeostasis and as such is essential for growth. The role of ESX2 and ESX4 remain still unknown.
The characterization of other Mtb surface constituents such as the mycobacterial adhesin HBHA[23] and PE_PGRS proteins[24,25] is starting to shed light on the molecular mechanisms involved in the interaction between the bacilli and host cells, and may lead to the development of “smart” tools capable of interfering with Mtb pathogenesis.
Another group of proteins known to play an important role in pathogenesis are those under the control of the dormancy survival regulon (Dos), which controls expression of more than 50 genes responsible for the Mtb hypoxic response.[26,27] Mtb senses the harsh environment in macrophages and granulomas, characterized by low oxygen and nutrient depletion, and responds by activating a dormant state, whereby the bacilli stops multiplying, down-regulate central metabolism and activate anaerobic metabolism, withinduction of stress proteins that provide Mtb with unique biological and immunological features.[28] These metabolically active but not replicating dormant bacilli can persist for a long time in vivo and may revert to an active state thanks to the resuscitating promoting factors (rpf), which act on the peptidoglycan to trigger a cascade of events that promotes bacterial growth.[29,30] Hence, Mtb persists in host tissues under different metabolic states, with important implications from a pathogenetic and clinical practical perspectives, sincedormant bacteria are susceptible only to certain antibiotics (pyrazinamide, rifampin and metronidazole) but resistant to other such as isoniazid.[31]
TB Pathogenesis
Mtb infection occurs when few tubercle bacilli dispersed in the air from a patient with active pulmonary TB reach the alveoli of the host. Here, Mtb is quickly phagocytized by professional alveolar macrophages that most often can kill the entering bacteria thanks to the innate immune response (Figure 2).[32] If the bacilli can survive this first line of defense, it starts actively replicating in macrophages, diffuse to nearby cells including epithelial and endothelial cells, reaching in few weeks of exponential growth a high bacterial burden.[33] During these early steps of infection, Mtb can diffuse to other organs through the lymphatics and by haematogenous dissemination where it can infect other cells.[34] Thereafter, once the adaptive immune response kicksin, migration to the site of primary infection of neutrophils, lymphocytes and other immune cells form a cellular infiltrate that later assume the typical structure of a granuloma.[35] Fibrotic components cover the granuloma that becomes calcified such that bacilli remain encapsulated inside and protected by the host immune response. This primary lesion, classically termed the Ghon complex,[36] was thought to be the “sanctuary” of Mtb during latent infection, with bacilli persisting in a dormant, non-metabolically active state, for years, decades, or most often for lifetime. In this scenario, when, during latent infection, for unknown reasons, bacilli would start replicating inside this primary lesion, active disease would ensue.[37] A major corollary of this hypothesis, with relevant pathophysiological and clinical implications, was that reactivation of TB originated from this very primary site of infection. This hypothesis was challenged since the early 20th century, when it was shown that viable and infective bacilli were found in unaffected portion of lung tissues of infected guinea pigs or human necropsy rather than from the central core of the tuberculous lesions.[37,38] Despite these early findings, only in 2000 Hernandez-Pando et al.,[39] using normal lung tissues isolated at necropsy from patients who had died for causes other than TB in a TB endemic country, were able to detect by in situ PCR Mtb DNA in non-phagocytic cells, fibroblasts and endothelial cells, clearly suggesting that in latent TB subjects Mtb bacilli can persists in tissues and cells not associated with the granuloma or the Ghon complex. Using similar experimental settings, Mtb was detected in the fat tissue surrounding several organs, residing intracellularly in adipocytes, where it can survive protected from the host immune response.[40] All these evidences suggest that during LTBI Mtb can reside in different organs, tissues and cell types, not associated with the site of primary infection and lacking any sign of the typical granulomatous lesions.
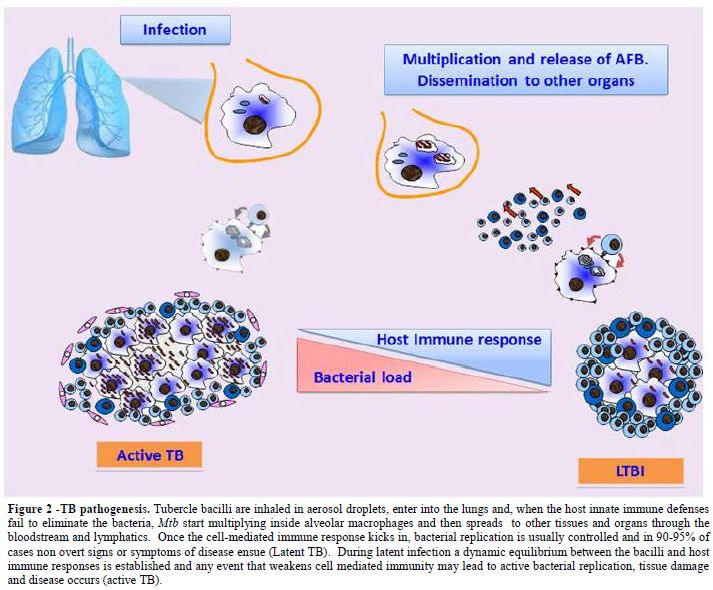
Figure 2. TB pathogenesis. Tubercle bacilli are inhaled in aerosol droplets, enter into the lungs and, when the host innate immune defenses fail to eliminate the bacteria, Mtb start multiplying inside alveolar macrophages and then spreads to other tissues and organs through the bloodstream and lymphatics. Once the cell-mediated immune response kicks in, bacterial replication is usually controlled and in 90-95% of cases non overt signs or symptoms of disease ensue (Latent TB). During latent infection a dynamic equilibrium between the bacilli and host immune responses is established and any event that weakens cell mediated immunity may lead to active bacterial replication, tissue damage and disease occurs (active TB).
Studies carried out in the non-human primate model of TB further corroborated these findings indicating that during latent infection Mtb is metabolically active and replicates in host tissues despite the lack of any clinical sign or symptom of disease.[41,42] Interestingly, in a single monkey with active TB it was possible to observe many different type of lesions, ranging from liquefied cavities with massive loads of bacilli, to necrotic or caseous hypoxic lesions with variable number of bacteria, to sterile lesions.[43] A similar scenario was observed in patients with pulmonary TB, where diverse lesions were observed simultaneously and with lesions responding differently to chemotherapy,[43] suggesting that they represent distinct Mtb subsets in different microenvironments.
Based on the new understanding of the biology of Mtb, its different metabolic states, the dynamic host immune responses occurring during infection and on the spectrum of conditions that are observed during infection, it has been proposed that during latent infection most bacilli persist in a dormant state with fewer Mtb found in an active replicating state. These replicating bacilli, named “scouts” are processed and killed by the host immune defenses and as a result they are responsible for the induction of the large number of effector/memory T cells directed against Mtb antigens that are found in the peripheral blood.[44] Hence, during latent TB dormant bacteria constantly replenish the bulk of actively replicating bacilli readily killed by thehost. When, for any reason, host immune responses fail to control these scouts, uncontrolled bacterial replication promotes diseases manifestations and active disease ensues.[45] Classical examples are highlighted by HIV infection that affects CD4 T cells that play a pivotal role in controlling Mtb replication;[46] treatment with biological therapies with anti-TNF that are known to increase the risk of developing TB disease up to 25 times in latent TB subjects as a result of the disruption of granuloma organization and depletion of certain populations of CD8 T cells known to play a role in controlling Mtb;[47,48] treatment with corticosteroids, vitamin D deficiency and any other condition affecting T cell function are also known to increase the risk of active TB in latent TB subjects, underscoring the clinical implications that any event capable of perturbing the host-pathogen dynamic equilibrium can have.
Cancer patients, including those with haematological diseases, are also at increased risk of developing TB and in these patients clinical outcomes are usually very aggressive, may present as systemic infections with a high fatality rate and diagnosis is usually delayed.[49,50] The context of the TB spectrum, with the immunological and biological implications previously discussed, clearly highlight the risk that an infection usually controlled by the host immune response with no clinical signs or symptoms, can reactivate once the subtle balance affecting the dynamic equilibrium between the host and the bacilli occurs. Hence, it is very important to deploy proper and effective diagnostic protocols capable of detecting latent infection in these high risk groups and very sensitive assays to identify active disease when TB is suspected.
TB Diagnosis
Direct diagnosis. Definitive diagnosis of TB requires the detection of Mtb from the biological sample by at least one of the current microbiological techniques: microscopical analysis, isolation in culture or molecular methods. These assays form the basis for the microbiological diagnosis of TB and the clinicians may require detection of Mtb in one or more specimens depending on the clinical symptoms, if any.[51] High sensitivity and specificity has been observed in the detection of Mtb in specimens such as sputum, bronchoalveolar lavage or induced sputum for the diagnosis of pulmonary TB.[52] The introduction of new, highly sensitive, fully automated molecular assays for the detection of Mtb has been recognized as a major achievement of the last decades,[53] though it is important to remind that molecular diagnosis should not be ordered routinely when the clinical suspicion of TB is too low.[54-56] Non-pulmonary forms of TB may be more problematic to diagnose because of the difficulties in identifying the proper specimens and the lower sensitivity of the microbiological assays in the non-pulmonary specimens, probably resulting from a lower bacterial concentration. Detection of Mtb in the urine or stools could be used to detect systemic infections and recently new assays capable of detecting mycobacterial components (lipoarabinomannan, LAM) in the urine were shown to be helpful to diagnose TB in HIV-infected subjects and immunocompromised patients, but not to diagnose pulmonary TB in immunocompetent subjects.[57,58]
Detection of Mtb in clinical specimens has been observed in HIV patients not showing any clinical sign or symptom of the disease[59] and in a recent report on the diagnosis of TB in children it was shown that ≈25% of children positive for Mtb did not show any clinical sign or symptom.[60] These results highlight the challenges associated with TB diagnosis and provide clinical evidences for the TB spectrum concepts.[43]
Immunological Diagnosis
The immunological diagnosis of TB has been historically performed by the Mantoux test or tuberculin skin test (TST) and the introduction in the last decade of the interferon-gamma release assays (IGRAs), that measure T cell responses directed against Mtb specific antigens in peripheral whole blood, has provided a new and valuable tool in the diagnosis of Mtb infection. Discussion of the immunological diagnosis of TB is beyond the scope of this review, but it is worth mentioning that TST and IGRAs are aimed at detecting Mtb infection but cannot distinguish between LTBI subjects with non signs or symptoms of disease and active TB patients.[61,62] Despite many efforts, the prognostic value of IGRAs was shown to be insufficient and while many experimental assays are being devised and tested with the attempt to improve the current RD1-based assays,[63] it is important to remind that IGRAs can be used only as an “aid” in the diagnosis of TB and cannot be used alone to rule out TB nor to make conclusive diagnosis of TB. The concept of the TB spectrum discussed in this review provides the biological and immunological framework to support this statement.
Acknowledgment
This work was funded by MIUR PRIN (project number 2009N98ST4_001) awarded to MS and GF.
References
- World Health Organization. Global Tuberculosis report 2012.
- Collins, H.L., Schaible, U.E. and Kaufmann,
S.H. Early IL-4 induction in bone marrow lymphoid precursor cells by
mycobacterial lipoarabinomannan. J. Immunol. 161, 5546-5554.
PMid:9820531

- Cole, S.T., Brosch, R., Parkhill, J.,
Garnier, T., Churcher, C., Harris, D., Gordon, S.V., Eiglmeier, K.,
Gas, S., Barry, C.E., III, Tekaia, F., Badcock, K., Basham, D., Brown,
D., Chillingworth, T., Connor, R., Davies, R., Devlin, K., Feltwell,
T., Gentles, S., Hamlin, N., Holroyd, S., Hornsby, T., Jagels, K. and
Barrell, B.G. Deciphering the biology of Mycobacterium tuberculosis
from the complete genome sequence. Nature 393, 537-544. http://dx.doi.org/10.1038/31159 PMid:9634230

- Brosch, R., Gordon, S.V., Marmiesse, M.,
Brodin, P., Buchrieser, C., Eiglmeier, K., Garnier, T., Gutierrez, C.,
Hewinson, G., Kremer, K., Parsons, L.M., Pym, A.S., Samper, S., van
Soolingen, D. and Cole, S.T. A new evolutionary scenario for the
Mycobacterium tuberculosis complex. Proc. Natl. Acad. Sci. U. S. A 99,
3684-3689. http://dx.doi.org/10.1073/pnas.052548299 PMid:11891304 PMCid:PMC122584

- Gutierrez, M.C., Brisse, S., Brosch, R.,
Fabre, M., Omais, B., Marmiesse, M., Supply, P. and Vincent, V. Ancient
origin and gene mosaicism of the progenitor of Mycobacterium
tuberculosis. PLoS. Pathog. 1, e5. http://dx.doi.org/10.1371/journal.ppat.0010005 PMid:16201017 PMCid:PMC1238740

- Hershberg, R., Lipatov, M., Small, P.M.,
Sheffer, H., Niemann, S., Homolka, S., Roach, J.C., Kremer, K., Petrov,
D.A., Feldman, M.W. and Gagneux, S. High functional diversity in
Mycobacterium tuberculosis driven by genetic drift and human
demography. PLoS. Biol. 6, e311. http://dx.doi.org/10.1371/journal.pbio.0060311 PMid:19090620 PMCid:PMC2602723
- Supply, P., Marceau, M., Mangenot, S.,
Roche, D., Rouanet, C., Khanna, V., Majlessi, L., Criscuolo, A., Tap,
J., Pawlik, A., Fiette, L., Orgeur, M., Fabre, M., Parmentier, C.,
Frigui, W., Simeone, R., Boritsch, E.C., Debrie, A.S., Willery, E.,
Walker, D., Quail, M.A., Ma, L., Bouchier, C., Salvignol, G., Sayes,
F., Cascioferro, A., Seemann, T., Barbe, V., Locht, C., Gutierrez,
M.C., Leclerc, C.,
Bentley, S.D., Stinear, T.P., Brisse, S., Medigue, C., Parkhill, J., Cruveiller, S. and Brosch, R. Genomic analysis of smooth tubercle bacilli provides insights into ancestry and pathoadaptation of Mycobacterium tuberculosis. Nat. Genet. 45, 172-179. http://dx.doi.org/10.1038/ng.2517 PMid:23291586
- Blaser, M.J. and Kirschner, D. The equilibria that allow bacterial persistence in human hosts. Nature 449, 843-849. http://dx.doi.org/10.1038/nature06198 PMid:17943121

- Wirth, T., Hildebrand, F., Allix-Beguec,
C., Wolbeling, F., Kubica, T., Kremer, K., van, S.D., Rusch-Gerdes, S.,
Locht, C., Brisse, S., Meyer, A., Supply, P. and Niemann, S. Origin,
spread and demography of the Mycobacterium tuberculosis complex. PLoS.
Pathog. 4, e1000160. http://dx.doi.org/10.1371/journal.ppat.1000160 PMid:18802459 PMCid:PMC2528947

- Comas, I., Coscolla, M., Luo, T., Borrell,
S., Holt, K.E., Kato-Maeda, M., Parkhill, J., Malla, B., Berg, S.,
Thwaites, G., Yeboah-Manu, D., Bothamley, G., Mei, J., Wei, L.,
Bentley, S., Harris, S.R., Niemann, S., Diel, R., Aseffa, A., Gao, Q.,
Young, D. and Gagneux, S. Out-of-Africa migration and Neolithic
coexpansion of Mycobacterium tuberculosis with modern humans. Nat.
Genet. 45, 1176-1182. http://dx.doi.org/10.1038/ng.2744 PMid:23995134

- Gagneux, S. Host-pathogen coevolution in human tuberculosis. Philos. Trans. R. Soc. Lond B Biol. Sci. 367, 850-859. http://dx.doi.org/10.1098/rstb.2011.0316 PMid:22312052 PMCid:PMC3267123

- Hoffmann, C., Leis, A., Niederweis, M.,
Plitzko, J.M. and Engelhardt, H. Disclosure of the mycobacterial outer
membrane: cryo-electron tomography and vitreous sections reveal the
lipid bilayer structure. Proc. Natl. Acad. Sci. U. S. A 105, 3963-3967.
http://dx.doi.org/10.1073/pnas.0709530105 PMid:18316738 PMCid:PMC2268800

- Zuber, B., Chami, M., Houssin, C.,
Dubochet, J., Griffiths, G. and Daffe, M. Direct visualization of the
outer membrane of mycobacteria and corynebacteria in their native
state. J. Bacteriol. 190, 5672-5680. http://dx.doi.org/10.1128/JB.01919-07 PMid:18567661 PMCid:PMC2519390

- Abdallah, A.M., Gey van Pittius, N.C.,
Champion, P.A., Cox, J., Luirink, J., Vandenbroucke-Grauls, C.M.,
Appelmelk, B.J. and Bitter, W. Type VII secretion--mycobacteria show
the way. Nat. Rev. Microbiol. 5, 883-891. http://dx.doi.org/10.1038/nrmicro1773 PMid:17922044

- Pym, A.S., Brodin, P., Brosch, R., Huerre,
M. and Cole, S.T. Loss of RD1 contributed to the attenuation of the
live tuberculosis vaccines Mycobacterium bovis BCG and Mycobacterium
microti. Mol. Microbiol. 46, 709-717. http://dx.doi.org/10.1046/j.1365-2958.2002.03237.x PMid:12410828

- Hsu, T., Hingley-Wilson, S.M., Chen, M.,
Dai, A.Z., Morin, P.M., Marks, C.B., Padiyar, J., Goulding, C.,
Gingery, M., Eisemberg, D., Russell, R.G., Derrick, S.C., Collins,
F.M., Morris, S.L., King, C.H. and Jacobs, W.R., Jr. The primary
mechanism of attenuation of bacillus Calmette-Guerin is a loss of
secreted lytic function required for invasion of lung interstitial
tissue. Proc. Natl. Acad. Sci. U. S. A. 2003, 12420-12425.

- van der, W.N., Hava, D., Houben, D.,
Fluitsma, D., van, Z.M., Pierson, J., Brenner, M. and Peters, P.J. M.
tuberculosis and M. leprae translocate from the phagolysosome to the
cytosol in myeloid cells. Cell 129, 1287-1298.

- Simeone, R., Bobard, A., Lippmann, J.,
Bitter, W., Majlessi, L., Brosch, R. and Enninga, J. Phagosomal rupture
by Mycobacterium tuberculosis results in toxicity and host cell death.
PLoS. Pathog. 8, e1002507. http://dx.doi.org/10.1371/journal.ppat.1002507 PMid:22319448 PMCid:PMC3271072

- Romagnoli, A., Etna, M.P., Giacomini, E.,
Pardini, M., Remoli, M.E., Corazzari, M., Falasca, L., Goletti, D.,
Gafa, V., Simeone, R., Delogu, G., Piacentini, M., Brosch, R., Fimia,
G.M. and Coccia, E.M. ESX-1 dependent impairment of autophagic flux by
Mycobacterium tuberculosis in human dendritic cells. Autophagy.
8, 1357-1370. http://dx.doi.org/10.4161/auto.20881 PMid:22885411 PMCid:PMC3442882

- Diel, R., Goletti, D., Ferrara, G.,
Bothamley, G., Cirillo, D., Kampmann, B., Lange, C., Losi, M., Markova,
R., Migliori, G.B., Nienhaus, A., Ruhwald, M., Wagner, D., Zellweger,
J.P., Huitric, E., Sandgren, A. and Manissero, D. Interferon-{gamma}
release assays for the diagnosis of latent M. tuberculosis infection: A
systematic review and meta-analysis. Eur. Respir. J.

- Serafini, A., Boldrin, F., Palu, G. and
Manganelli, R. Characterization of a Mycobacterium tuberculosis ESX-3
conditional mutant: essentiality and rescue by iron and zinc. J.
Bacteriol. 191, 6340-6344. http://dx.doi.org/10.1128/JB.00756-09 PMid:19684129 PMCid:PMC2753049

- Houben, E.N., Bestebroer, J., Ummels, R.,
Wilson, L., Piersma, S.R., Jimenez, C.R., Ottenhoff, T.H., Luirink, J.
and Bitter, W. Composition of the type VII secretion system membrane
complex. Mol. Microbiol. 86, 472-484. http://dx.doi.org/10.1111/j.1365-2958.2012.08206.x PMid:22925462

- Delogu, G., Fadda, G. and Brennan, M.J.
Impact of Structural Domains of the Heparin Binding Hemagglutinin of
Mycobacterium tuberculosis on Function. Protein Pept. Lett. 19,
1035-1039. http://dx.doi.org/10.2174/092986612802762697 PMid:22533618

- Iantomasi, R., Sali, M., Cascioferro, A.,
Palucci, I., Zumbo, A., Soldini, S., Rocca, S., Greco, E., Maulucci,
G., De, S.M., Fraziano, M., Fadda, G., Manganelli, R. and Delogu, G.
PE_PGRS30 is required for the full virulence of Mycobacterium
tuberculosis. Cell Microbiol. 14, 356-367. http://dx.doi.org/10.1111/j.1462-5822.2011.01721.x PMid:22050772

- Zumbo, A., Palucci, I., Cascioferro, A.,
Sali, M., Ventura, M., D'Alfonso, P., Iantomasi, R., Di, S.G., Ria, F.,
Sanguinetti, M., Fadda, G., Manganelli, R. and Delogu, G. Functional
dissection of protein domains involved in the immunomodulatory
properties of PE_PGRS33 of Mycobacterium tuberculosis. Pathog. Dis
 .
.
- Kumar, A., Toledo, J.C., Patel, R.P.,
Lancaster, J.R., Jr. and Steyn, A.J. Mycobacterium tuberculosis DosS is
a redox sensor and DosT is a hypoxia sensor. Proc. Natl. Acad. Sci. U.
S. A 104, 11568-11573. http://dx.doi.org/10.1073/pnas.0705054104 PMid:17609369 PMCid:PMC1906723

- Voskuil, M.I., Visconti, K.C. and
Schoolnik, G.K. Mycobacterium tuberculosis gene expression during
adaptation to stationary phase and low-oxygen dormancy. Tuberculosis.
(Edinb.) 84, 218-227. http://dx.doi.org/10.1016/j.tube.2004.02.003 PMid:15207491

- Korch, S.B., Contreras, H. and
Clark-Curtiss, J.E. Three Mycobacterium tuberculosis Rel
toxin-antitoxin modules inhibit mycobacterial growth and are expressed
in infected human macrophages. J. Bacteriol. 191, 1618-1630. http://dx.doi.org/10.1128/JB.01318-08 PMid:19114484 PMCid:PMC2648211

- Hett, E.C., Chao, M.C. and Rubin, E.J.
Interaction and modulation of two antagonistic cell wall enzymes of
mycobacteria. PLoS. Pathog. 6, e1001020. http://dx.doi.org/10.1371/journal.ppat.1001020 PMid:20686708 PMCid:PMC2912383

- Mukamolova, G.V., Turapov, O., Malkin, J.,
Woltmann, G. and Barer, M.R. Resuscitation-promoting factors reveal an
occult population of tubercle Bacilli in Sputum. Am. J. Respir. Crit
Care Med. 181, 174-180. http://dx.doi.org/10.1164/rccm.200905-0661OC PMid:19875686 PMCid:PMC2809243

- Fox, W., Ellard, G.A. and Mitchison, D.A.
Studies on the treatment of tuberculosis undertaken by the British
Medical Research Council tuberculosis units, 1946-1986, with relevant
subsequent publications. Int. J. Tuberc. Lung Dis. 3, S231-S279.
PMid:10529902

- Urdahl, K.B., Shafiani, S. and Ernst, J.D.
Initiation and regulation of T-cell responses in tuberculosis. Mucosal.
Immunol. 4, 288-293. http://dx.doi.org/10.1038/mi.2011.10 PMid:21451503 PMCid:PMC3206635

- Wolf, A.J., Desvignes, L., Linas, B.,
Banaiee, N., Tamura, T., Takatsu, K. and Ernst, J.D. Initiation of the
adaptive immune response to Mycobacterium tuberculosis depends on
antigen production in the local lymph node, not the lungs. J. Exp. Med.
205, 105-115. http://dx.doi.org/10.1084/jem.20071367 PMid:18158321 PMCid:PMC2234384

- Balasubramanian, V., Pavelka, M.S., Jr.,
Bardarov, S.S., Martin, J., Weisbrod, T.R., McAdam, R.A., Bloom, B.R.
and Jacobs, W.R., Jr. Allelic exchange in Mycobacterium tuberculosis
with long linear recombination substrates. J. Bacteriol. 178, 273-279.
PMid:8550428 PMCid:PMC177649

- Ottenhoff, T.H. and Kaufmann, S.H.
Vaccines against tuberculosis: where are we and where do we need to go?
PLoS. Pathog. 8, e1002607. http://dx.doi.org/10.1371/journal.ppat.1002607 PMid:22589713 PMCid:PMC3349743

- Ghon, N. The primary complex in human tuberculosis and its significance. American Review of Tuberculosis 7, 314-317.

- Bishai, W.R. Rekindling old controversy on elusive lair of latent tuberculosis. Lancet 356, 2113-2114. http://dx.doi.org/10.1016/S0140-6736(00)03485-1

- Feldman, W.H. and Baggenstoss, A.H. (1938)
The residual infectivity of the primary complex of tuberculosis. Am. J.
Pathol. 14, 473-490. PMid:19970404 PMCid:PMC1964987

- Hernandez-Pando, R., Jeyanathan, M.,
Mengistu, G., Aguilar, D., Orozco, H., Harboe, M., Rook, G.A. and
Bjune, G. Persistence of DNA from Mycobacterium tuberculosis in
superficially normal lung tissue during latent infection. Lancet 356,
2133-2138. http://dx.doi.org/10.1016/S0140-6736(00)03493-0

- Neyrolles, O., Hernandez-Pando, R.,
Pietri-Rouxel, F., Fornes, P., Tailleux, L., Barrios Payan, J.A.,
Pivert, E., Bordat, Y., Aguilar, D., Prevost, M.C., Petit, C. and
Gicquel, B. Is adipose tissue a place for Mycobacterium tuberculosis
persistence? PLoS. ONE. 1, e43. http://dx.doi.org/10.1371/journal.pone.0000043
PMid:17183672 PMCid:PMC1762355
- Ford, C.B., Lin, P.L., Chase, M.R., Shah,
R.R., Iartchouk, O., Galagan, J., Mohaideen, N., Ioerger, T.R.,
Sacchettini, J.C., Lipsitch, M., Flynn, J.L. and Fortune, S.M. Use of
whole genome sequencing to estimate the mutation rate of Mycobacterium
tuberculosis during latent infection. Nat. Genet. 43, 482-486. http://dx.doi.org/10.1038/ng.811 PMid:21516081 PMCid:PMC3101871

- Gideon, H.P. and Flynn, J.L. Latent tuberculosis: what the host "sees"? Immunol. Res. 50, 202-212. http://dx.doi.org/10.1007/s12026-011-8229-7 PMid:21717066 PMCid:PMC3788603

- Barry, C.E., III, Boshoff, H.I., Dartois,
V., Dick, T., Ehrt, S., Flynn, J., Schnappinger, D., Wilkinson, R.J.
and Young, D. The spectrum of latent tuberculosis: rethinking the
biology and intervention strategies. Nat. Rev. Microbiol. 7, 845-855.
PMid:19855401

- Chao, M.C. and Rubin, E.J. Letting
sleeping dos lie: does dormancy play a role in tuberculosis? Annu. Rev.
Microbiol. 64, 293-311. http://dx.doi.org/10.1146/annurev.micro.112408.134043 PMid:20825351

- Gengenbacher, M. and Kaufmann, S.H. Mycobacterium tuberculosis: success through dormancy. FEMS Microbiol. Rev. 36, 514-532. http://dx.doi.org/10.1111/j.1574-6976.2012.00331.x PMid:22320122 PMCid:PMC3319523

- Pawlowski, A., Jansson, M., Skold, M.,
Rottenberg, M.E. and Kallenius, G. Tuberculosis and HIV co-infection.
PLoS. Pathog. 8, e1002464.

- Beham, A.W., Puellmann, K., Laird, R.,
Fuchs, T., Streich, R., Breysach, C., Raddatz, D., Oniga, S.,
Peccerella, T., Findeisen, P., Kzhyshkowska, J., Gratchev, A.,
Schweyer, S., Saunders, B., Wessels, J.T., Mobius, W., Keane, J.,
Becker, H., Ganser, A., Neumaier, M. and Kaminski, W.E. A TNF-regulated
recombinatorial macrophage immune receptor implicated in granuloma
formation in tuberculosis. PLoS. Pathog. 7, e1002375.

- Bruns, H., Meinken, C., Schauenberg, P.,
Harter, G., Kern, P., Modlin, R.L., Antoni, C. and Stenger, S. Anti-TNF
immunotherapy reduces CD8+ T cell-mediated antimicrobial activity
against Mycobacterium tuberculosis in humans. J. Clin. Invest 119,
1167-1177. http://dx.doi.org/10.1172/JCI38482 PMid:19381021 PMCid:PMC2673881

- Cordonnier, C., Martino, R., Trabasso, P.,
Held, T.K., Akan, H., Ward, M.S., Fabian, K., Ullmann, A.J., Wulffraat,
N., Ljungman, P., Alessandrino, E.P., Pretnar, J., Gmur, J., Varela,
R., Vitek, A., Sica, S. and Rovira, M. Mycobacterial infection: a
difficult and late diagnosis in stem cell transplant recipients. Clin.
Infect. Dis. 38, 1229-1236. http://dx.doi.org/10.1086/383307 PMid:15127333

- Maartens, G. and Wilkinson, R.J. Tuberculosis. Lancet 370, 2030-2043. http://dx.doi.org/10.1016/S0140-6736(07)61262-8

- Delogu, G. and Herrmann, J.L. Mycobacterium species. In: European Manual of Clinical Microbiology (Cornaglia, G., Courcol, R., Herrmann, J.L., Kahlmeter, G., Peigue-Lafeuille, H. and Vila, J., Eds.), pp. 297-307. ESCMID.
- Drouillon, V., Delogu, G., Dettori, G.,
Lagrange, P.H., Benecchi, M., Houriez, F., Baroli, K., Ardito, F.,
Torelli, R., Chezzi, C., Fadda, G. and Herrmann, J.L. Multicenter
evaluation of a transcription-reverse transcription concerted assay for
rapid detection of Mycobacterium tuberculosis complex in clinical
specimens. J. Clin. Microbiol. 47, 3461-3465. http://dx.doi.org/10.1128/JCM.01730-08 PMid:19741080 PMCid:PMC2772632

- Evans, C.A. GeneXpert--a game-changer for tuberculosis control? PLoS. Med. 8, e1001064.

- Updated guidelines for the use of nucleic
acid amplification tests in the diagnosis of tuberculosis. MMWR Morb.
Mortal. Wkly. Rep. 58, 7-10.

- Lawn, S.D., Brooks, S.V., Kranzer, K.,
Nicol, M.P., Whitelaw, A., Vogt, M., Bekker, L.G. and Wood, R.
Screening for HIV-associated tuberculosis and rifampicin resistance
before antiretroviral therapy using the Xpert MTB/RIF assay: a
prospective study. PLoS. Med. 8, e1001067.
- Dowdy, D.W., Cattamanchi, A., Steingart,
K.R. and Pai, M. Is scale-up worth it? Challenges in economic analysis
of diagnostic tests for tuberculosis. PLoS. Med. 8, e1001063. http://dx.doi.org/10.1371/journal.pmed.1001067 PMid:21818180 PMCid:PMC3144215

- Lawn, S.D. Point-of-care detection of
lipoarabinomannan (LAM) in urine for diagnosis of HIV-associated
tuberculosis: a state of the art review. BMC. Infect. Dis. 12, 103. http://dx.doi.org/10.1186/1471-2334-12-103 PMid:22536883 PMCid:PMC3423001

- Lawn, S.D., Kerkhoff, A.D., Vogt, M. and
Wood, R. Diagnostic accuracy of a low-cost, urine antigen,
point-of-care screening assay for HIV-associated pulmonary tuberculosis
before antiretroviral therapy: a descriptive study. Lancet Infect. Dis.
12, 201-209. http://dx.doi.org/10.1016/S1473-3099(11)70251-1

- Lawn, S.D., Wood, R. and Wilkinson, R.J.
Changing concepts of "latent tuberculosis infection" in patients living
with HIV infection. Clin. Dev. Immunol. 2011.

- Buonsenso, D., Lancella, L., Delogu, G.,
Krzysztofiak, A., Testa, A., Ranno, O., D'Alfonso, P. and Valentini, P.
A 20-Year Retrospective Study of Pediatric Tuberculosis in Two Tertiary
Hospitals in Rome. Pediatr. Infect. Dis. J.

- Goletti, D., Carrara, S., Butera, O.,
Amicosante, M., Ernst, M., Sauzullo, I., Vullo, V., Cirillo, D.,
Borroni, E., Markova, R., Drenska, R., Dominguez, J., Latorre, I.,
Angeletti, C., Navarra, A., Petrosillo, N., Lauria, F.N., Ippolito, G.,
Migliori, G.B., Lange, C. and Girardi, E. Accuracy of immunodiagnostic
tests for active tuberculosis using single and combined results: a
multicenter TBNET-Study. PLoS. ONE. 3, e3417.

- Andersen, P., Doherty, T.M., Pai, M. and
Weldingh, K. The prognosis of latent tuberculosis: can disease be
predicted? Trends Mol. Med. 13, 175-182. http://dx.doi.org/10.1016/j.molmed.2007.03.004 PMid:17418641

- Delogu, G., Chiacchio, T., Vanini, V.,
Butera, O., Cuzzi, G., Bua, A., Molicotti, P., Zanetti, S., Lauria,
F.N., Grisetti, S., Magnavita, N., Fadda, G., Girardi, E. and Goletti,
D. Methylated HBHA produced in M. smegmatis Discriminates between
Active and Non-Active Tuberculosis Disease among RD1-Responders. PLoS.
ONE. 6, e1815.
