Received: April 28, 2014
Accepted: July 10, 2014
Meditterr J Hematol Infect Dis 2014, 6(1): e2014055, DOI 10.4084/MJHID.2014.055
This article is available on PDF format at:

Abraham T. Yacoub1, Lysenia Mojica1, Lily Jones2, Andrea Knab2, Sally Alrabaa2 and John Greene1,2
1 DH.
Lee Moffitt Cancer Center and Research Institute. 12902 Magnolia Drive,
Tampa, Florida 33612-9497.
2 University of South Florida, Division of
Infectious Diseases. 1 Tampa General Circle, G323, Tampa, FL 33606.

|
This
is an Open Access article distributed
under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract In
the past decades, viridans group Streptococci (VGS) have emerged as an
important cause of bacteremia in neutropenic patients with cancer. The
clinical course of VGS bacteremia can be devastating including septic
shock and adult respiratory distress syndrome (ARDS). It has been
suggested that septicemia with VGS triggers the development of
noncardiogenic pulmonary edema in patients with pre-existing damage of
the lungs due to aggressive cytotoxic treatment. Thus, the preemptive
administration of corticosteroid to patients diagnosed with VGS
bacteremia with early onset of respiratory failure has been employed to
prevent ARDS. While this management strategy has been suggested in the
literature, little published data are available to validate this
practice. In this study, we sought to review the benefit of early
administration of corticosteroid to patients who developed symptom or
early signs of respiratory failure while being neutropenic with VGS
bacteremia.
|
Introduction
During
the last decades, gram-positive bacteremia has increased dramatically.
Gram-positive cocci are the most frequent cause of nosocomial
bloodstream infections. Among Gram-positive cocci, Viridans
streptococci are a common cause of bacteremia in cancer patients with
neutropenia, causing serious complications such as pneumonia, septic
shock, and ARDS.[1-6] We present a
series of cases of
VGS bacteremia complicated with ARDS; early initiation of
corticosteroids resulted in complete recovery.
Materials and Methods
A retrospective chart review of patients with hematologic malignancy
diagnosed with VGS bacteremia admitted to the Moffitt Cancer Center in
Tampa, Florida between 1/1/2001 and 4/1/2012 was completed. Data was
collected about respiratory symptoms, diagnosis of adult respiratory
syndrome, results of blood cultures, medications received and outcome.
Sepsis was defined as suspected or microbiologically proven infection
together with Systemic inflammatory response system (SIRS). The SIRS
criteria was defined as temperature less than or equal to 36°C or
greater than or equal to 38°C. Heart rate greater than or equal to 90.
Respiratory rate greater than 20 breaths per minute or a partial
pressure of carbon dioxide (PaCO2) less than 32 mmHg and a white blood
cell (WBC) count greater than or equal to 12,000 cell/mm3 or less than
or equal to 4,000 cell/mm3
or greater than 10% bands. VGS bacteremia was defined as growth of
viridans streptococci from at least one peripheral or central blood
sample. Neutropenia was defined as having an ANC lower than 500/μL
Results
In this study, 70 cases of VGS bacteremia in neutropenic patients were
reviewed. The most common adverse event of VGS bacteremia in this group
of patients is the development of serious pulmonary complications such
as ARDS. In our study (Table
1),
7 patients developed ARDS. The ages of all 7 patients ranged from 22 to
75. There were 4 females and 3 males. There were 3 Caucasian patients,
1 African American patient, 1 Hispanic patient, and 1 Middle Eastern
patient. Acute lymphoblastic leukemia was found in 4 patients and acute
myelogenous leukemia was found in 3 patients. The type of chemotherapy
for the management of the hematological malignancies was not available.
All of the patients were neutropenic. The average length of neutropenia
was 11 days. The average of the length of stay in the hospital was 35
days. The most common identifies streptococcal species were Streptococcus mitis
and Streptococcus oralis,
isolated in 4 of 7 patients. The most common antibiotics administered
after positive blood cultures were cefepime, vancomycin, and meropenem.
All 7 patients received corticosteroids early with the onset of
respiratory failure. The most commonly prescribed regimen was
methylprednisolone 60 mg intravenously every 12 hour for an average of
3 days. All patients received comparable supportive care, appropriate
antibiotics, ventilation and hemodynamic support. All patients (100%)
recovered from respiratory failure after receiving corticosteroids. One
patient expired due to Graft-versus-Host Disease complication post
chemotherapy treatment. There were no significant adverse events
attributable to steroids use.
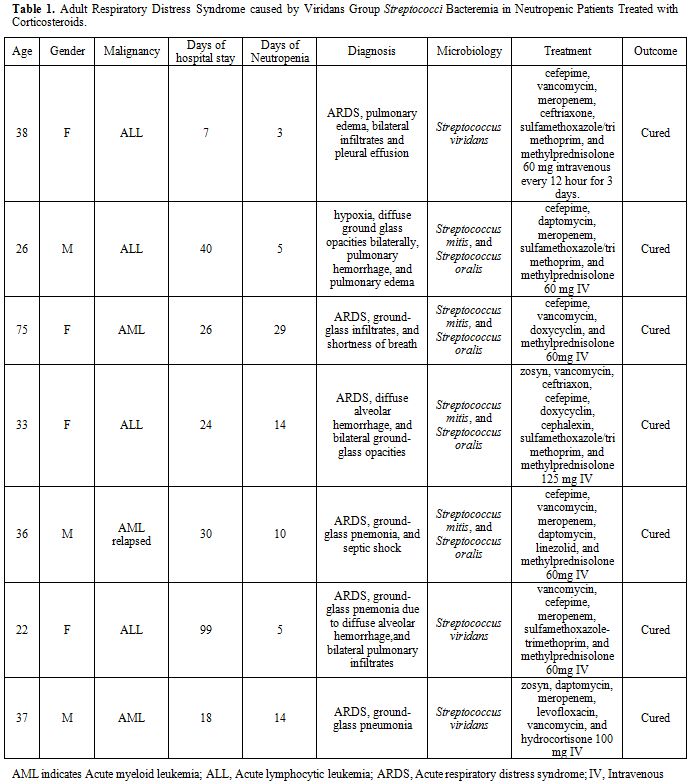 | Table 1. Adult Respiratory Distress Syndrome caused by Viridans Group Streptococci Bacteremia in Neutropenic Patients Treated with Corticosteroids. |
Discussion
Viridans streptococci are gram-positive spherical bacteria that
characteristically form pairs or chains during growth. They are
catalase-negative, facultative anaerobic, non-motile, and do not
produce spores or gas.[5]
The viridans streptococci include S
mitis, S
mutans, S
salivarius, S
sanguis,
and others. Viridans streptococci typically are alpha-hemolytic,
optochin-resistant, their colonies are not soluble in bile, and they
have carbohydrate fermentation patterns.[7]
They are
the most prevalent members of the oral normal flora, other areas of the
upper respiratory tract, and are important for the healthy state of the
mucous membranes there. They also commonly inhabit the gastrointestinal
and female genital tracts.[7,8] The
viridians
streptococci are described as organisms of low virulence, however these
organisms may invade sterile body sites, which can lead to
life-threatening diseases (e.g., endocarditis, meningitis, and
pneumonia).[5-7]
Viridans streptococcal bacteremia occurs frequently in neutropenic
patients, who have impaired host defense mechanisms and especially when
the oral mucosa is disrupted, causing serious complications. Serious
complications described include: a shock syndrome, characterized by
hypotension, rash, palmar desquamation, and adult respiratory distress
syndrome.[2,3,5,6,16,20]
The mortality rate among patients with viridans streptococcal
bacteremia who develop complications is high, up to 80% in some case
series.[2,3,6]
Streptococcus mitis
is the species most frequently isolated from the patients who have
developed serious complications from viridans bacteremia like sepsis
and/or adult respiratory distress syndrome (ARDS).[3,6,9,10,17-19]
The incidence of viridans streptococcal bacteremia has increased during
the last decades.[2,3]
In a study conducted in a university hospital for adults in Barcelona,
Spain, of 485 episodes of bacteremia in neutropenic patients, viridans
streptococci caused a total of 88 episodes (18%), and 10 of these
patients developed serious complications such as ARDS and septic shock.
From the 10 patients that developed complications, 7 involved Streptococcus mitis.[3] These complications were associated
with a high mortality rate (80%), secondary to the development of
multi-organ failure.
The risk factors associated with viridans streptococcal bacteremia that
have been identified are oral mucositis, profound neutropenia,
high-dose chemotherapy like cytosine arabinoside, bone marrow
transplantation, antimicrobial prophylaxis with
trimethoprim-sulfamethoxazole or a fluoroquinolone, and the use of
antacids, histamine type 2 receptor antagonists or proton pump
inhibitors.[1-3,6,11-13]
Some studies propose that the administration of
trimethoprim-sulfamethoxazole or fluoroquinolone, as well as the use of
antacids to prevent chemotherapy induce gastritis may predispose to
overgrowth of viridans streptococci in the gastrointestinal tract.[5]
One study found that the significant risk factors to developed serious
complications were: severe oral mucositis, high-dose chemotherapy with
cyclophosphamide, and allogenic bone marrow transplantation.[3]
The pathogenesis of these complications remains unknown. It is believed
that neutrophils play a key role in the development of ARDS.[10]
There is evidence that viridans streptococci can induce proinflammatory
cytokines including TNF-α, TNF-β, IL-6, and IL-8. The up-regulation of
intercellular adhesion molecule (ICAM)-1 by Streptococcus mitis
has also been demonstrated. Of note, IL-8 has an important association
with lung damage in patients with ARDS. Viridans streptococci do not
produce lipopolysaccharide (endotoxin), and there is no substantial
information reported regarding the ability of these microorganisms to
produce exotoxins. Therefore, it has been postulated that the
pathogenesis of streptococcus viridans causing septic shock and/or ARDS
is of host immune etiology.[5,9-11,14,15]
One study conducted in Germany, found much higher levels of IL-6 in 2
patients with lethal alpha-hemolytic streptococcus septic shock, than
in controls with uncomplicated gram-positive bacteremia.[15]
Another study using enzyme-linked immunoabsorbent assays compared the
ability of cell-free bacterial supernatants derived from commensal and
clinical strains of viridans streptococci to induce pro-inflammatory
cytokines. In their results they reported that supernatants from
clinical isolates induced significantly more TNF-β, and IL-8 than did
supernatants from commensal strains.[10]
Given the
fact that IL-8 is a chemoattractant cytokine for neutrophils, and
neutrophils are involved in the pathogenesis of ARDS, some studies have
proposed the association between the increased levels of IL-8 in
viridans streptococcal bacteremia and the development of ARDS.[10]
One study found that of 52 viridans streptococcus strains isolated from
the blood of neutropenic patients, all induced the production of TNF-α,
IL-1β, and IL-8. This study also suggested the ability of viridans
streptococcus to cause the up-regulation of ICAM-1 and subsequent
development of shock.[9]
The administration of moderate dose corticosteroids may be beneficial
in preventing the development of ARDS in patients with Streptococcus
mitis bacteremia. Our findings reflect 100% recovery from a
complication (ARDS) that carries between 30-80% mortality. Furthermore,
moderate doses of steroids with short duration of administration were
not associated with significant adverse events in our case series. At
University Hospital St. Radboud, Nijmegen at The Netherlands, 11
patients with Streptococcus
mitis bacteremia following chemotherapy received high
doses of corticosteroids pre-emptively. None of them developed ARDS.[14]
These findings and our observation of improved mortality with early
administration of corticosteroids with Streptococcus viridans
bacteremia in neutropenic cancer patients who develop respiratory
complications, are of great clinical interest. Further studies are
warranted.
Conclusion
Streptococcus mitis is the species most frequently isolated from the patients who have developed ARDS from Streptococci viridans group bacteremia. Our data suggest that the early administration of corticosteroids to neutropenic patients who develop early signs of respiratory failure with VGS bacteremia can prevent the progression of ARDS and improve survival. Moderate doses of steroids with short duration of administration were not associated with significant adverse events in our case series. While the use of corticosteroids in this setting has been described in the literature since the early 1990s, there remains a scarcity of data and our study help shed some light on this area. Moreover there is little recognition among clinicians of the association between ARDS and VGS bacteremia (particularly mitis species in neutropenic cancer patients) and thus this treatment modality is used late in the course of illness which may reduce benefit. Further studies are warranted to validate these findings and to further examine the utility of preemptive use of corticosteroids in cancer patients who develop VGS bacteremia, in regards to ARDS incidence reduction.
References




















[TOP]