Mohsen S. Elalfy1, Fatma S.E. Ebeid1, Iman A. Elagouza1, Fatma A. Ibrahim2, Noura B.M. Hassan1 and Beshoy A. Botros1.
1 Paediatrics, Faculty of Medicine, Ain Shams University, Egypt.
2 Biochemistry Department, National research centre, Egypt.
Corresponding
author: Fatma Soliman Elsayed Ebeid.
Address: 2 Lotfy Elsayed st, Ain Shams University staff campus. Mobile
no.: 00201095569596. E-mail:
dr.fatma_ebeid@yahoo.com
Published: January 1, 2018
Received: November 11, 2017
Accepted: December 22, 2017
Mediterr J Hematol Infect Dis 2018, 10(1): e2018010 DOI
10.4084/MJHID.2018.010
This article is available on PDF format at:

This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background:
To evaluate the hazard of prolonged antibiotic therapy and/or
persistent diarrhea on vitamin K1 (VK1) level and bleeding profile in
infants (2-24 weeks).
Methods:
A one-year case-control study, conducted at Ain Shams University,
Egypt. 338 infants (2-24 weeks) were recruited and divided into 3
groups (1:1:3 ratios); group A (n=67) patients who received antibiotics
for ≥10 days, group B (n=67) who had persistent diarrhea ≥ 14 days and
group C (n=204) age- and gender- matched infants who had not either
received antibiotics nor had diarrhea. All subjected to clinical
assessment, bleeding history and had their complete blood count (CBC),
PT and PTT, liver transaminases and VK1 level assayed.
Results:
There was a significant increase in frequency of VKDB (vitamin K
deficiency bleeding) and abnormal bleeding profile in cases than
control group. There was significant negative correlation between VK1
level and duration of diarrhea, length of antibiotics used and bleeding
profile. Antibiotic usage has hazardous effect on VK1 level in those
with diarrhea; more patients were receiving antibiotic in those with
persistent diarrhea and VKDB (N=55) than those with persistent diarrhea
and normal VK1 (N=12). The longer duration of antibiotic therapy the
lower level of VK1. Combining cephalosporin/penicillin therapy and/or
diarrhea, in particular, had an impact on VK1 level.
Conclusion:
VKDB, a preventable cause of life-threatening hemorrhage, is still a
major health problem in Egyptian infants, where persistent diarrhea and
misuse of antibiotics are prevalent, necessitate a booster dose of VK
in those high risk infants.
|
Introduction
Hemorrhagic disease of newborn (HDN) is one of the most common causes of acquired hemostatic disorder in early infancy.[1] It is categorized as early, classical and late depending on the time of onset.[2]
The most common manifestation of late HDN reported are; intracranial
hemorrhage, deep ecchymosis, bleeding from gastrointestinal tract
and/or from the mucous membrane, skin punctures or surgical incisions.[3-4]
Vitamin
K (VK) plays an integral role in the clotting cascade; its deficiency;
specifically in vulnerable neonates with insufficient stores, can lead
to spontaneous bleeding and devastating effects. The American Academy
of Paediatrics recommends intramuscular (IM) VK prophylaxis for all
newborns to prevent early onset HDN.[5] Newborn babies
are at particular risk of vitamin K deficiency (VKD), has only 20-50%
of adult coagulation activity, as placental transfer is limited and
human milk is a poor source. A minimal amount of VK passes through the
placenta, and a negligible amount is also found in breast milk. Factors
including failure to administer VK at birth, exclusive breastfeeding
for a long period, prolonged or chronic diarrhea, and prolonged use of
antibiotics could lead to vitamin K deficiency bleeding (VKDB).[1]
Data
from a longitudinal household survey conducted in 1990–1991 in rural
Egypt show that treatment of acute diarrheal episodes is still far from
optimal, in particular, the prescription of antibiotics is still too
frequent. Children taken to the government clinics, private physicians
or pharmacies are more likely to be given antibiotics therapy.[6]
Egypt is one of the developing countries where there are many mistakes
from healthcare givers regarding management of diarrheal illness and
early detection of VKDB disorders. Moreover, in a recent Egyptian
study; exclusive breastfeeding, diarrhea lasting more than one week and
antibiotic consumption were more common in intracranial hemorrhage than
in the control group.[7] Consequently, the present
study was intended to assess the impact of persistent diarrheal disease
and prolonged use of antibiotics on the VK1 level in the infants aged
from 2 to 24 weeks. By providing evidence of the unsafe impact of abuse
of antibiotics on the VK1 level the study suggests the need for an
additional dose of VK to patients on prolonged courses of antibiotics
or persistent diarrhea.
Subjects and Methods
This
study was a case-control study, conducted at Ain Shams University,
Children Hospital throughout the period from May 2015 to May 2016. The
infants included in our study were recruited from the emergency and
outpatient clinic of Ain Shams University pediatrics hospital (tertiary
care hospital) they were seeking medical advice for a variety of
clinical symptoms.
A total number of 338 infants aged two to 24
weeks of both sexes were recruited. Exclusion criteria were infants or
their mother who were on any treatment that will affect their bleeding
profile, infants who had history of bleeding tendency or those who had
an underlying condition that could affect their bleeding profile or
those who had platelet count <100,000/mm3
or elevated liver enzymes or direct bilirubin > double high normal.
They were categorized into three groups: group (A) included 67 patients
who received antibiotics for ten days or more, group (B) included 67
had persistent diarrhea more than 14 days according to the World Health
Organization (WHO).[8] Group (C) included 204 age- and
gender-matched infants and were neither on antibiotics nor had diarrhea
this group acted as control group.
A verbal informed consent was
obtained from the guardian of each patient or control before
participation. The procedures applied in this study were approved by
the institutional, regulatory board Pediatric Hospital, Faculty of
Medicine, Ain Shams University, on 23 March 2015, and are in accordance
with the Helsinki Declaration of 1975.
All patients were
subjected to thorough clinical assessment with special emphasis on
antenatal history of any maternal illness or medication, mode and place
of delivery, history of VK administration at birth, neonatal ICU
admission, dietetic history, family history of consanguinity and
bleeding tendency in siblings and relatives were inquired. In addition,
a history of prolonged diarrhea or antibiotic use, or bleeding, liver
or kidney diseases was stressed. They were also thoroughly examined for
any signs of bleeding tendencies or liver disease to be excluded from
the study.
Laboratory assessment: Six milliliters of venous blood
was collected from the studied subjects under complete aseptic
conditions for the evaluation of the following:
1. Complete blood
count (CBC), samples were obtained on potassium-ethylene diamine acetic
acid (K2EDTA) vacutainer and assessed using Beckman Coulter counter
(Coulter Corporation, Florida, USA). Complete blood count was evaluated
for all the recruited infants to exclude different causes of bleeding
as thrombocytopenia.
2. Liver transaminases (ALT and AST): Liver
enzymes were done to prohibit liver disease as a cause of VK
insufficiency and all patients had ALT and AST inside of the ordinary
levels.
3. Prothrombin time (PT) and partial thromboplastin time
(PTT) assessment (using platelet poor plasma (PPP) preparation).
Samples were obtained on Na citrated vacutainer (1 part citrated sodium
(0.11 mol/L) with nine parts venous blood, (PPP) was collected by
centrifugation at 3000 × g for 15 minutes. PT, PTT, and INR were done
as determinants of the VK1 level of the included infants. According to
our Ain Shams University, Children Hospital laboratory reference range;
the control for PT was 14 seconds (s) classifying any result above 14
as drawn out, PTT control was 44s, and INR standard values were
distributed within 1.4.
4. Vitamin K 1 level: samples were
obtained on heparin, centrifuged for 30 minutes at 3000 rpm at 2-8°C
and then stored at -20°C or -80°C for later assessment at national
research centre by double antibody sandwich enzyme-linked
immune-sorbent assay (ELISA) (Glory Science Co., Ltd, Del Rio, TX
78840, USA). According to manufacturer manual, standard and
testing samples were singularly added to the conventional wells, then
of HRP-conjugate reagent was also added to each well, covered and
incubated and then washed. Next chromogen solution A and B were added,
were gently mixed and were incubated. Afterward, stop solution was
added to each well, the colour in the wells should then change from
blue to yellow. Finally, the optical density (O.D.) was measured
spectrophotometrically at a wavelength of 450 nm. The concentration of
VK1 was determined by comparing the O.D. of the samples to the standard
curve. Our cut-off, mean value of standards multiply by three, was 300
Pg/ml. The sensitivity of this assay is 1.0 pmol/mL.
Statistical analysis.
Data were collected, coded and entered into the Statistical Package for
Social Science (IBM SPSS). Qualitative data presented as number and
percentages while quantitative data presented as mean, standard
deviations and ranges when parametric and median with interquartile
ranges (IQR) (IQR; 75th and 25th
percentiles) when nonparametric. Kolmogorov Smirnov test was used for
testing the distribution of normality. The comparison between two
groups was performed by using Chi-square test and/or Fisher exact test
(when the expected count in any cell was found less than five) when the
data were qualitative, independent t-test when the data were
quantitative with parametric distribution and Mann-Whitney test when
data were non-parametric. The one-way analysis of variance (ANOVA) is
used to test for differences among at least three groups; then a post
hoc test was used whenever a significant difference between three or
more sample means was revealed by ANOVA. The Kruskal–Wallis test is a
non-parametric method for comparing two or more independent samples.
Pearson correlation coefficients were used to assess the association
between two normally distributed variables. When a variable was not
normally distributed, a Spearman correlation test was performed.
Multivariable linear regression analysis was employed to determine the
relation between VK1 level and other variables. The confidence interval
was set to 95% and the margin of error accepted was set to 5%.
Therefore, the p-value was considered significant < 0.05 Results
The
study included 338 children with mean age of 11.69 ± 6.88 weeks (2 -
24), they were 221 males and 117 females with a ratio of 1.89:1. Table 1
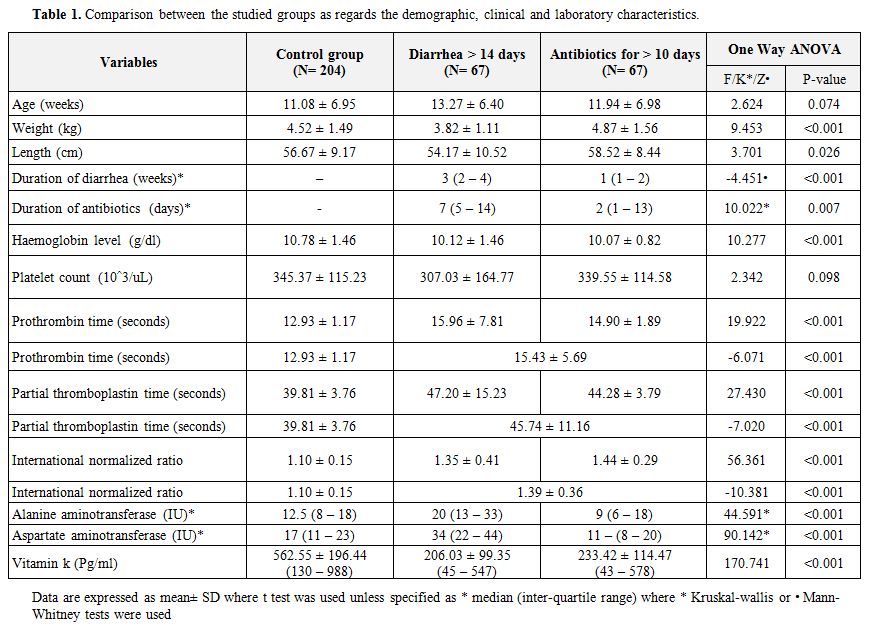
showed the demographic data of the studied infants; the three groups
had comparable mean age and gender distribution. Some growth
parameters, mean weight was 3.82 ± 1.11, showed delayed growth in the
group with persistent diarrhea in comparison to control and those on
antibiotics as shown in Table 1.
Furthermore, mild anemia; statistically significant drop of
hemoglobin level in the group on prolonged antibiotic use either due to
underlying illness or prolonged antibiotic use.
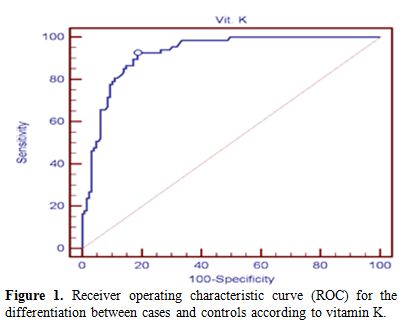
To assess the
cut-off level of VK1, a graph of sensitivity against 1 – specificity, a
receiver operating characteristic (ROC) curve had been done. Although
the ROC curve (Figure 1) showed
that the best cut-off point between cases and control group according
to vitamin k was ≤ 412 Pg/ml with sensitivity 95% (CI) of 92.54% and
specificity 95% (CI) of 81.40% while area under the curve (AUC) 95%
(CI) was 0.923, and +PV was 72.1 and –PV is 95.5, we used the cut-off
of 300 Pg/ml which is the cut-off of the used kits in our study.
The
mean VK1 (Pg/ml) level ± SD (Range) for the control group was 562.55 ±
196.44 (130 – 988), for those who suffer from diarrhea more than 14
days was 206.03 ± 99.35 (45 – 547), and for those receiving antibiotics
therapy for more than ten days was 233.42 ± 114.47 (43 – 578). There
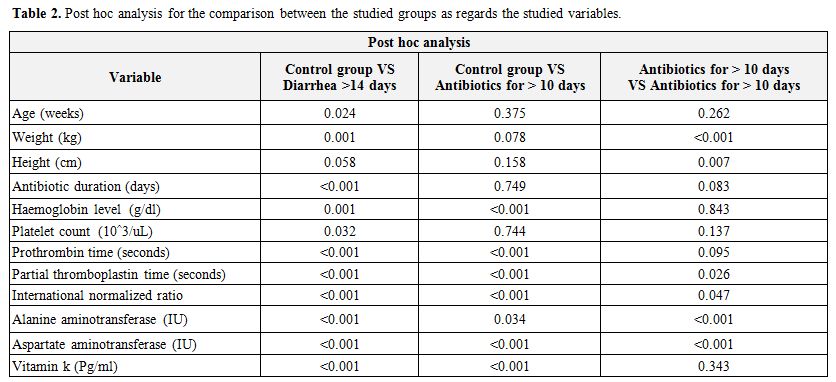
was statistically significant lower VK1 level in both patients groups
than control group as illustrated in Table 1 and 2.
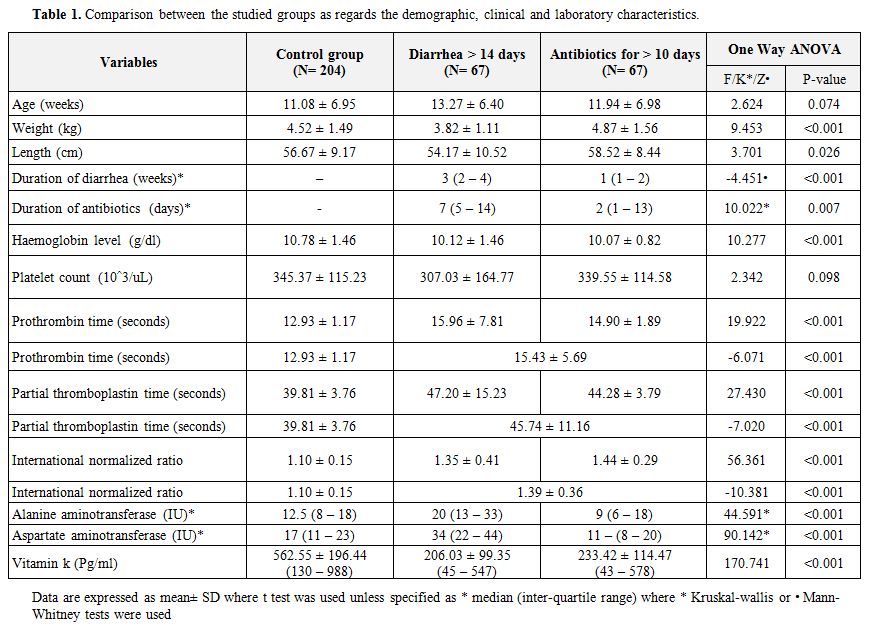 |
Table 1.
Comparison between the studied groups as regards the demographic, clinical and laboratory characteristics. |
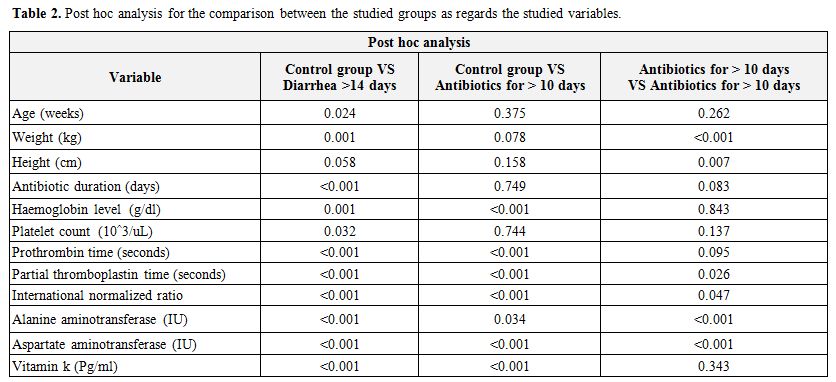 |
Table 2.
Post hoc analysis for the comparison between the studied groups as regards the studied variables. |
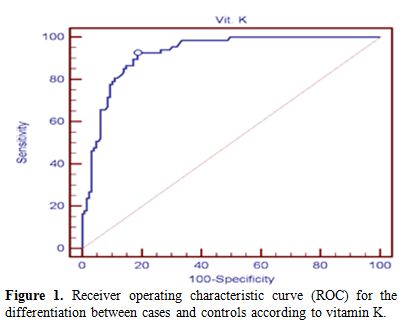 |
Figure 1 Receiver operating characteristic
curve (ROC) for the differentiation between cases and controls
according to vitamin K. |
Characteristics of patients who received antibiotics therapy for ≥ ten days (group A).
Ninety-nine of the studied patients were on antibiotic treatment
(74.6%) with median (IQR) of 7 (1 – 13.5); of them 28 (20.9%) were
treated with cephalosporins, 26 (19.4%) were on penicillins, 12 (9%)
were on metronidazole, 34 (25.4%) were treated with a combination.
Sixty-seven patients received antibiotic therapy for ten days or more
with a median duration of 12 days (10 – 18). Of them, 14 (21.2%) were
treated with cephalosporins, 7 (9.8%) received penicillins, 3 (4.2%)
metronidazole and 4 (2%) a combination.
Three main classes of
antibiotics that were observed have indistinguishable impact on VK1.
Thirty-five %, 32% and 40% of infants received cephalosporins,
penicillins and metronidazole had serum VK1 below cut-off value
respectively (but the aggregate sum of patients on metronidazole was
only five infants). The group which received a combination of
cephalosporins and penicillins had the most astounding occurrence of
VK1 inadequacy (24 out of the 30 infants (80%).
The leading causes for the administration of the antibiotic treatment more than ten days were upper
respiratory
tract infection, pneumonia, and gastroenteritis. Twenty-one infants had
gastroenteritis; 18 of them (85%) had low VK1 serum level, which was
also found low in 76% of infants with pneumonia and in 71% of infants
with upper respiratory tract infection (URTI).
Almost half of
patients who received antibiotics for 10 days or more, 35 out of the 67
infants (52%) had abnormal coagulation profile in the form of prolonged
PT, PTT and INR, which demonstrates the connection between prolonged
usage of antibiotics and the variations from the norm in the
coagulation profile and the bleeding that could ensue.
Fifty-two
of the 67 (77%) who received antibiotics for ten days or more had lower
serum level of VK1 than the predicted for age (300 Pg/ml). Duration of
antibiotic utilization influenced VK1 level by a significant negative
correlation as illustrated in Figure 2,
and there was statistically significant negative correlation between
VK1 and INR (r: -0.313, p: 0.001), and PT, PTT. Out of 18 children
on 14 days or more of antibiotic therapy, 17 had levels underneath the
cut off value (94%) (VKD), extremely low levels of VK1 were detected
(<15% of the calculated low cutoff level), and one infant had a
marginal value of 320 Pg/ml.
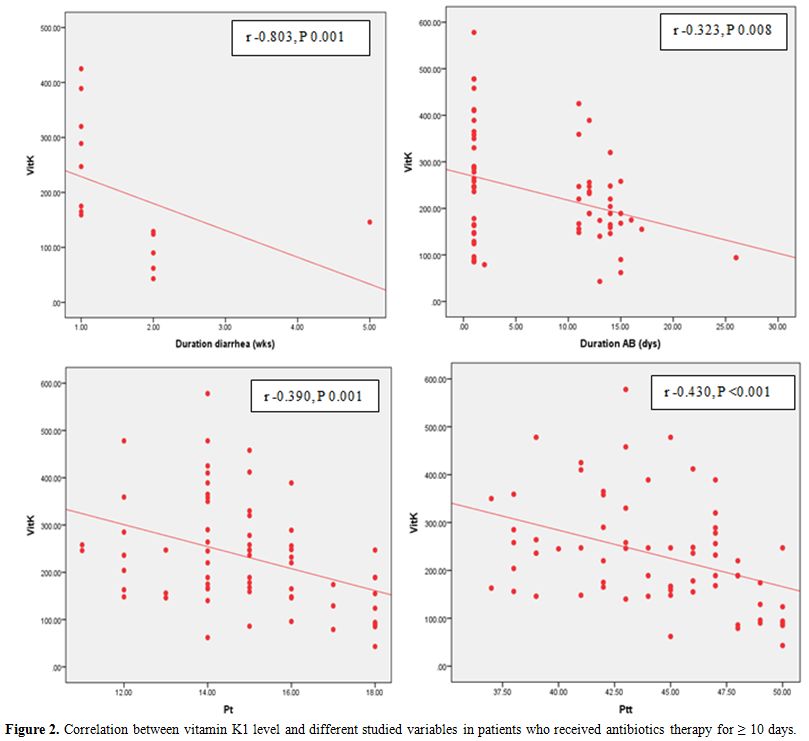 |
Figure 2. Correlation
between vitamin K1 level and different studied variables in patients
who received antibiotics therapy for ≥ 10 days. for the comparison
between the studied groups as regards the studied variables.
|
Characteristics of patients who received pronged use of diarrhea ≥14days (Group B).
Sixty-seven patients had diarrhea for ≥14 days with a median (IQR) 3
weeks (2 – 4). Fifty-five patients (82.1%) out of them had serum level
of VK1 lower than predicted for age (300 Pg/ml), and 31.3% had abnormal
coagulation profile in the form of prolonged PT, PTT, and INR.
Almost
half of the infants who suffered from persistent diarrhea received
antibiotics (n=33, 49.3%); ten of them was on cephalosporins, ten on
metronidazole, five on penicillin, and eight on mixed antibiotics
regimens. There is a significant difference between those on different
type of antibiotics and those on none (F=4.868, p=0.002)
When
patients having suffered from persistent diarrhea and having VKD (N=55)
were compared to those who suffered from persistent diarrhea but had
normal VK1 level (N=12), a statistically significant higher incidence
of antibiotic therapy was found in patients with VK1 deficient (31
patients (93.9%)) than in those with normal VK1 (2 patients (6.1%)) [x2=6.211, p=0.012].
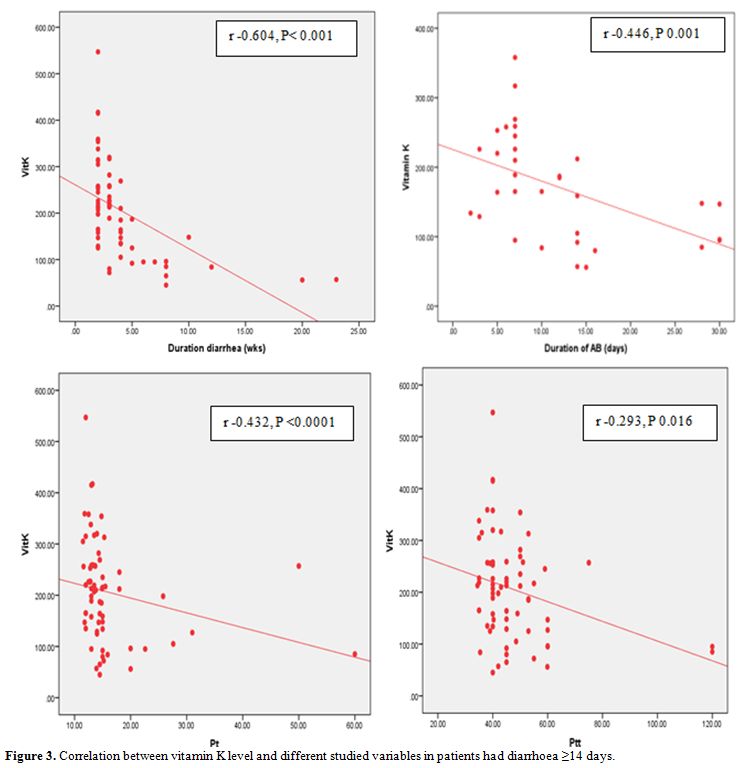
Patients
who suffered from diarrhea for ≥14 days have statistically significant
negative correlation between VK1 and INR (r: -0.446, p: 0.001) and
coagulation profile illustrated in Figure 3 and statistically significant positive correlation with haemoglobin level (r: 0.292, p: 0.016).
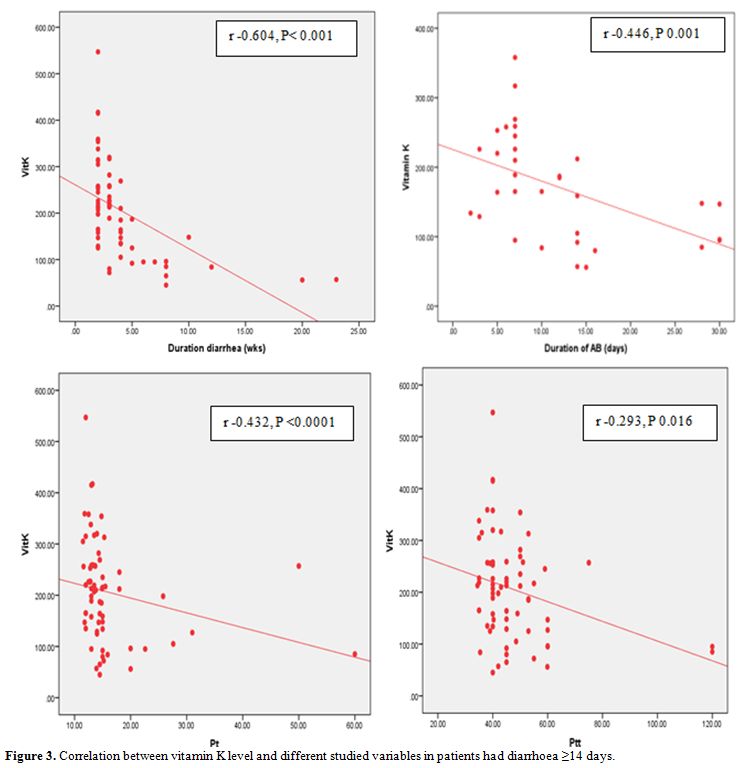 |
Figure 3. Correlation between vitamin K level and different studied variables in patients had diarrhoea ≥14 days.
|
Discussion
Vitamin
K deficiency is an important cause of acquired bleeding diathesis in
neonates and infants and its deficiency does not develop in healthy
infants receiving a normal diet. However, in the presence of diarrhea
and/or antibiotic usage leading to suppression of intestinal bacteria,
and consequently VKD may occur.[9] A systematic review
reported that the median burden of late VKD bleeding was 35 per 100 000
live births in infants who had not received prophylaxis at birth; the
burden was much higher in low- and middle-income countries as compared
with high-income countries.[10]
The studied
population in the present study was infants aged from 2 to 24 weeks; we
were guided by the fact that more than 50% of the patients with low
serum VK1 level was in the age group from one month to one year.[11] In addition, late HDN usually occurs between 2-12 weeks and manifests after the second week of life[12] up to 6 months of age.[13]
Other causes of bleeding tendency like liver disease and
thrombocytopenia or congenital clotting factors deficiency were ruled
out by the simple investigations (liver function tests and platelet
count). In addition, patients did not receive any dosages of VK in the
preceding weeks to the study, and most parents of infants included did
not recall if their infants received VK prophylaxis at birth.
It
is important to highlight that VK occurred in two biologically
active forms: phylloquinone (VK1), and menaquinones (VK2). The VK1, the
type of plant origin, is predominantly transported to the liver and
mediates in the maturation of several blood coagulation factors.[14] The VK2 is synthesized by bacteria in human and animal intestine.[15] It is the form almost exclusively stored in the liver in the neonates,[16]
and it has a more widespread tissue distribution and is thus more
specifically involved in the carboxylation of matrix Gla protein (MGP).[17] Vitamin K circulates in the human bloodstream at very low levels because of a weak intake in the diet.[18] It could be detected in human plasma using high-performance liquid chromatography-tandem mass spectrometry.[19]
In the current study, we measure VK1 directly using the ready available
ELISA technique. This method is superior to measuring proteins induced
by vitamin K absence (PIVKA) and synthesized as a result of vitamin K
deficiency, whose level is related to the severity of the deficiency.[20]
The
impact of diarrheal illnesses in elaborating VKD was related to
insufficient intake; failure of synthesis owing to a shift in the
bacterial flora caused by diarrhea and/or administration of antibiotics
and decreased absorption from the intestinal tract.[21] In agreement with other studies,[22-24]
we found that persistent diarrhea impairs VK1 level, and by that
adversely affecting the coagulation profile of those infants,
especially in the age less than 24 weeks old. Deficiency of VK in
infants with diarrhea is likely to be more frequent and more severe in
developing countries because of malnutrition and lack of vitamin K
supplementation at birth.[1] Discovering of VKD in
children with persistent diarrhea especially in those who sought
medical advice shows that physicians lack the notion that correlates
persistent diarrhea and VKD bleeding. Consequently, it is highly
advisable to monitor coagulation profile (VK testing) to identify
risk factors related to VKD of patients in which the diarrheal process
is perpetuating.
Also, it is to be mentioned that none of our
patients suffered from any bleeding incidents, or had any hemorrhagic
episodes during the treatment or afterward except a three months old
male who suffered from intracranial hemorrhage after 20 days of
intractable watery diarrhea with 10-15 motions per day. He has no
history of VK supplementation at birth and has no bleeding history
previously. A previous Egyptian study found that not only VKD bleeding
is more prevalent than in developed countries (21 in 158,608 live
births), but also it was the most common cause of intracranial
hemorrhage in that age group, occurs in 50% of VKD cases.[7]
The
role of antibiotics in the pathogenesis of VKD is produced by
inhibition of intestinal microorganisms with loss of healthy bowel
flora, which synthesizes the vitamin.[25] In
addition, cephalosporins containing side chains of
N-methylthiotetrazole are inhibitors of hepatic vitamin K epoxide
reductase and that a lower nutritional-vitamin K status predisposes to
hypoprothrombinemia.[26] In our study, we concluded
that infants receiving antibiotics ≥ more than ten days showed the most
astounding occurrence of VKD and the longer the antibiotic course was,
the more affected the VK1 level. In agreement with other studies,[27-28]
we found that treatment with combination of cephalosporins and
penicillins showed the highest frequency of VKD and led to abnormal
coagulation parameters. Furthermore, we found a higher incidence of VKD
in those who had diarrhea and on antibiotic therapy (94%) than those
who had diarrhea and not on antibiotics therapy (70%), this is showing
the fact that both diarrhea and prolonged antibiotic usage have a
double impact on VK1 levels. This association is crucial the antibiotic
misuse alone can cause diarrhea further affecting the vitamin K status
of the affected infant.
Our study spots the light on some health
problems. The abuse of antibiotics seems most incriminated in the Arab
region, and although not sufficiently investigated, studies performed
in Jordan[29-30] revealed that just less than
one-half of all dispensed antibacterial drugs were without a
prescription (46%), either via self-medication (23.2%) or pharmacist
recommendation (23.1%). The high prevalence of antibiotics misused
in our cohort may be explained by the availability of over the counter
antibiotics along with the low price of some antimicrobials encourage
their consumption leading to numerous cases of antibiotic abuse and the
prescription of antimicrobials for treatment of viral infections and
inappropriate usage regarding duration of therapy.
Furthermore,
although VK is obligatory administration to all newborns in our country
yet the efficiency of VK prophylaxis program cannot be reliably
assessed because the majority of the parents did not recall the
information and also birth records are not sufficient to verify whether
VK prophylaxis has been administrated or not. Similarly, in Turkey VKDB
is one of the most common causes of acquired hemostatic disorder in
early infancy. Although VK is practiced routinely after every birth,
the compliance of prophylactic measures does not seem to be
satisfactory.[31] As a further measure of tomorrow,
we vigorously emphasize that a national surveillance program should be
initiated. An additional intramuscular dose or oral supplementation of
vitamin K especially for exclusively breastfed infants may reduce this
catastrophic problem in our country. Thus, care providers need to give
accurate information to families regarding the risks and benefits of VK
prophylaxis and should be registered, and home births should be
monitored for VK prophylaxis. Vitamin K prophylaxis status, date, dose,
and route of administration should be documented on vaccination cards
as it is being done for hypothyroid screening in our country. An
inter-professional approach for education can be useful in increasing
acceptance of VK prophylaxis and decreasing the incidence of VKD.
Limitations
In
the study cohort, the area under the curve was chosen to determine VKD.
The underlying condition of persistent diarrhea was not mentioned which
could affect the VKD status. Including the data of an infant with ICH.
The sample size is relatively small to use the data to be generalized
to a population-based study.
Conclusions
Vitamin
K deficiency, a preventable cause of life-threatening bleeding, is
still a major health problem in Egyptian infants, where high incidence
of persistent diarrhea and misuse of antibiotics is prevalent.
Large-scale study to assess the value of booster prophylactic VK might
avoid a preventable cause of life-threatening hemorrhage.
References
- Pooni, P.A., Singh, D., Singh, H., Jain. B.K.
Intracranial hemorrhage in late hemorrhagic disease of the newborn.
Indian Pediatrics. 2003; 40, 243-248.

- Sutor, A. Vitamin K Deficiency Bleeding in Infants and Children. Semin Thromb Hemost.1995; 21(3), 317-329. https://doi.org/10.1055/s-2007-1000653

- Enz,
R., Anderson, R.S Jr. A Blown Pupil and Intracranial Hemorrhage in a
4-Week-Old: A Case of Delayed Onset Vitamin K Deficiency Bleeding, a
Rare "Can't Miss" Diagnosis. J Emerg Med. 2016; 51(2), 164-7. https://doi.org/10.1016/j.jemermed.2015.06.089

- Wolpert,
K., Szadkowski, M., Miescier, M., Hewes, H.A. The Presentation of a
Fussy Infant With Bruising: Late-Onset Vitamin K Deficiency Bleeding.
Pediatr Emerg Care. 2017; [Epub ahead of print ]

- Hamrick,
H.J., Gable, E.K., Freeman, E.H., Dunn, L.L., Zimmerman, S.P., Rusin,
M.M., Linthavong, O.R., Wright, M.E., Moss LA, Skinner, A.C. Reasons
for Refusal of Newborn Vitamin K Prophylaxis: Implications for
Management and Education. Hosp Pediatr. 2016; 6 (1), 15-21. https://doi.org/10.1542/hpeds.2015-0095

- Langsten, R. and Hill, K. Treatment of childhood diarrhea in rural Egypt. Social Science & Medicine. 1995; 40 (7), 989-1001 https://doi.org/10.1016/0277-9536(94)00163-N

- Elalfy,
M., Elagouza, I., Ibrahim, F., Abdelmessieh, S., Gadallah, M.
Intracranial haemorrhage is linked to late onset vitamin K deficiency
in infants aged 2–24 weeks. Acta Paediatr.2014; 17, 12598. https://doi.org/10.1111/apa.12598

- Bhandari,
M.K., Bhan, M.K. and Sazawal, S. Mortality associated with acute watery
diarrhea, dysentery and persistent diarrhea in rural North India. Acta
Paediatr Suppl. 1992; 381:3-6. https://doi.org/10.1111/j.1651-2227.1992.tb12363.x

- Corrigan, J.J. Jr. The vitamin K dependent proteins. Adv Pediatr. 1981; 28, 57-74.

- Sankar,
M.J., Chandrasekaran, A., Kumar, P., Thukral, A., Agarwal, R., Paul,
V.K. Vitamin K prophylaxis for prevention of vitamin K deficiency
bleeding: a systematic review. J Perinatol. 2016; 36 Suppl 1, S29-35. https://doi.org/10.1038/jp.2016.30

- Bhat,
R.V. and Deshmukh, C.T. A study of vitamin K status in children on
prolonged antibiotic therapy. Indian Pediatrics. 2003; 40, 36-40.

- Cekinmez,
M., Cemil, T., Cekinmez, E.K., Altinors, N. Intracranial hemorrhages
due to late – type vitamin K deficiency. Child's Nervous System. 2008;
24 (7), 821-25. https://doi.org/10.1007/s00381-007-0537-9

- Sutor,
A.H., von Kries, R., Cornelissen, E.A.M., McNinich, A.W. and Andrew, M.
ISTH Pediatric/Perinatal Subcommittee International Society on
Thrombosis and Haemostasis. Vitamin K deficiency bleeding (VKDB) in
infancy. Thromb Haemost. 1999; 81, 456–61

- Thaiss,
H. (1986) Vorkommen, Resorption und Transport von Vitamin K. In: Sutor,
A.H, W Künzer (Eds): Physiologie und Pathophysiologie des Vitamins K.
Editiones Roche, Basel Grenzach-Wyhlen; 21-27.
- Shearer, M.J. Vitamin K. Lancet. 1995; 345, 229–34. https://doi.org/10.1016/S0140-6736(95)90227-9

- Shearer, M.J. Vitamin K metabolism and nutriture. Blood Rev.1992; 6, 92–104. https://doi.org/10.1016/0268-960X(92)90011-E

- Thijssen,
H.H., Drittij-Reijnders, M.J. Vitamin K status in human tissues:
tissue-specific accumulation of phylloquinone and menaquinone. Br J
Nutr. 1996; 75, 121-127. https://doi.org/10.1079/BJN19960115

- Gentili,
A., Cafolla, A., Gasperi, T., Bellante, S., Caretti, F., Curini, R.,
Fernández, V.P. Rapid, high performance method for the determination of
vitamin K (1), menaquinone-4 and vitamin K (1) 2,3-epoxide in human
serum and plasma using liquid chromatography-hybrid quadrupole linear
ion trap mass spectrometry. J Chromatogr A. 2014; 1338, 102-10. https://doi.org/10.1016/j.chroma.2014.02.065

- Suhara,
Y., Kamao, M., Tsugawa, N., and Okano, T. Method for the Determination
of Vitamin K Homologues in Human Plasma Using High-Performance Liquid
Chromatography-Tandem Mass Spectrometry. Anal. Chem. 2005; 77 (3),
757–763. https://doi.org/10.1021/ac0489667

- Widdershoven,
J., van Munster, P., de Abreu, R., Bosman, H., van Lith, T., van der
Putten-van Meyel, M., Motohara, K. and Matsuda, I. Four methods
compared for measuring des-carboxy-prothrombin (PIVKA-II). Clin Chem
1987; 33:2074–2078.

- Kumar,
R., Marwaha, N., Marwaha, R.K., Garewal, G. Vitamin K deficiency in
diarrhoea. The Indian Journal of Pediatrics. 2001; 68 (3), 235-238. https://doi.org/10.1007/BF02723197

- Ozdemir,
M.A., Karakukcu, M., Per, H., Unal, E., Gumus, H., Patiroglu, T.
Late-type vitamin K deficiency bleeding: experience from 120 patients.
Childs Nerv Syst. 2012; 28 (2), 247-51. https://doi.org/10.1007/s00381-011-1575-x

- Ahmet,
F.O., Ali, B., Vefik, C. and Abdurahman, U. Evaluation of Vitamin K
Deficiency in Children with Acute and Intractable Diarrhea. Advances in
Therapy. 2006; 2 (3), 469-474.

- Izquierdo,
R.J., Arriaga, G.M., Kuri, N.J., et al. Blood coagulation disorders in
infants with infectious gastroenteritis. Bol Med Hosp Infant Mex. 1977;
34, 981-992.

- Firkin,
F., Chesterman, C., Penington, D. (1989) Coagulation Disorders. In: de
Gruchy's Clinical Hematology in Medical Practice, 5th ed. Delhi: Oxford
university pres; 436-437.

- Shearer,
M.J., Bechtold, H., Andrassy, K., Koderisch, J., McCarthy, P.T., Trenk,
D., Jähnchen, E., Ritz, E. Mechanism of cephalosporin-induced
hypoprothrombinemia: relation to cephalosporin side chain, vitamin K
metabolism, and vitamin K status. J Clin Pharmacol. 1988; 28(1), 88-95 https://doi.org/10.1002/j.1552-4604.1988.tb03106.x

- Fainstein,
V., Bodey, G.P., McCredie, K.B., Keating, M.J., Estey, E.H., Bolivar,
R., Elting, L. Coagulation abnormalities induced by beta-lactam
antibiotics in cancer patients. J Infect Dis. 1983; 148(4), 745-50. https://doi.org/10.1093/infdis/148.4.745

- Bolat,
A., Vurucu, S., Tascilar, E., Gursel, O., Karaoglu, A., Kurekci, A.E.
Late Type Vitamin K Deficiency Related with Prolonged Antibiotic
Therapy in a 7-month-old Infant. International Journal of Hematology
and Oncology. 2010; 20 (2), 106-109.

- Darwish,
D.A., Abdelmalek, S., Dayyih, W.A., Hamadi, S. Awareness of antibiotic
use and antimicrobial resistance in the Iraqi community in Jordan. J
Infect Dev Countries. 2014; 8 (5), 616-623. https://doi.org/10.3855/jidc.4086

- Al-Bakri,
A.G., Bustanji, Y.B., Yousef, A.M. Community consumption of
antibacterial drugs within the Jordanian population: sources, patterns
and appropriateness. International Journal of Antimicrobial Agents.
2005; 26, 389–395. https://doi.org/10.1016/j.ijantimicag.2005.07.014

- Unal,
E., Ozsoylu, S., Bayram, A., Ozdemir, M.A., Yilmaz, E., Canpolat, M.,
Tumturk, A., Per, H. Intracranial hemorrhage in infants as a serious,
and preventable consequence of late form of vitamin K deficiency: a
selfie picture of Turkey, strategies for tomorrow. Childs Nerv Syst.
2014; 30(8):1375-82. https://doi.org/10.1007/s00381-014-2419-2