Matteo Chinello¹, Daniela Di
Carlo², Francesca Olivieri², Rita Balter¹, Massimiliano De Bortoli¹,
Virginia Vitale¹, Ada Zaccaron¹, Elisa Bonetti¹, Alice Parisi³ and
Simone Cesaro¹.
1 Pediatric Hematology Oncology, Azienda Ospedaliera Universitaria Integrata, Verona, Italy.
² Mother and Child Department, University of Verona.
³ Department of Pathological Anatomy, Azienda Ospedaliera Universitaria Integrata, Verona, Italy.
Corresponding
author: Matteo Chinello, M.D. Pediatric Hematology Oncology, Azienda
Ospedaliera Universitaria Integrata, Piazzale A. Stefani 1, 37126,
Verona, Italy. Fax: +390458127887, Tel: +390458127816. E-mail:
matteo.chinello@aovr.veneto.it
Published: July 1, 2018
Received: April 25, 2018
Accepted: June 15, 2018
Mediterr J Hematol Infect Dis 2018, 10(1): e2018043 DOI
10.4084/MJHID.2018.043
This article is available on PDF format at:

This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background:
Kaposiform Hemangioendothelioma (KHE) is a rare vascular tumour of the
infancy and the first decade of life. It is locally aggressive and
potentially life threatening when associated with consumptive
coagulopathy, known as Kasabach-Merritt syndrome (KMS). No consensus or
guideline for the therapy has been reached because of the lack of
prospective trials, and the different standard care suggestions are
based on retrospective case series.
Case report:
We report the case of a 9-month-old male with KHE and KMS in which the
initial response, obtained with prednisone and vincristine, was
subsequently consolidated and strengthened by long-term treatment with
sirolimus, a mTOR inhibitor. A summary of the published data is
presented as well.
Conclusions:
The inhibition of mTOR pathway represents the most important
therapeutic innovation introduced in the last few years for KHE. Our
case shows the effectiveness and good tolerance of long-term therapy
with sirolimus.
|
Introduction
Kaposiform
Hemangioendothelioma (KHE) is a rare vascular tumour of the infancy and
the first decade of life. KHE shows no sex predilection, is locally
aggressive and potentially life threatening when associated with
consumptive coagulopathy known as Kasabach-Merritt syndrome (KMS). KHE
has an incidence of 0.7/100.000/year,[1] and it can
appear anywhere over the body with a wide range of clinical
presentations. Macroscopically KHE is characterised by the presence of
abundant vascular structures that infiltrate the surrounding soft
tissues, and it is structured as a tender mass that causes pain when
platelets congest within the vessels, and coagulation cascade is
activated. Tumour nodules have irregular borders and they are composed
of fascicles of spindle endothelial cells which are positive for
vascular markers like CD31 and CD34, and negative for Glut1, with a low
Ki67 proliferative index, rare mitosis, no nuclear atypia, no necrosis.
KHE shows no tendency to metastasize.[2] KMS is
usually associated with a reduction of platelets count and haemoglobin,
a lengthening of prothrombin time (PT), partial thromboplastin time
(PTT), and to a reduction of fibrinogen. No consensus or guideline for
the therapy has been reached because of the lack of prospective trials,
and the different standard care suggestions are based on retrospective
case series. We report a severe case of KHE with KMS successfully
treated with prednisone and vincristine, used to induce the initial
response and subsequently consolidated and strengthened by long-term
treatment with sirolimus. The inhibition of mTOR pathway by sirolimus
is an important therapeutic innovation introduced in the last few
years, and a review of the published data is discussed.
Case Report
A
9-month-old male was admitted to the emergency department several times
in three months for respiratory and urinary tract infections,
constipation, recurrent abdominal pain with globose abdomen, and
failure to thrive. The blood exams showed a recurrent thrombocytopenia
interpreted as resulting from infections. Screening for celiac disease
was negative. In the last access to the emergency department blood
exams showed thrombocytopenia (110 x109/L) and anaemia (Hb 8,9 g/dl) with white blood cell 8.3 x109/L,
PT 1.26 (n.v 0.80-1.17), PTT 1.17 (v.n 0.80-1.20), fibrinogen 0.83 g/L
(n.v 2-4), D-dimer >10.000 mcg/L (n.v < 0,25), antithrombin III
100% (n.v 70-130). In the following weeks, he manifested a progressive
decrease in the number of platelets, with a minimum value of 9 x 109/L.
An
ultrasound of the abdomen revealed a solid mass of about 6 x 2,3 cm in
the retroperitoneal space, without clear margin, locally spread around
the mesenteric vessels’ origins. The lesion was confirmed by magnetic
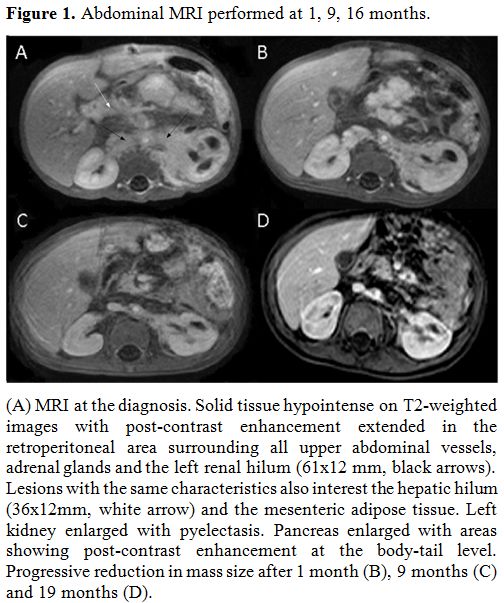
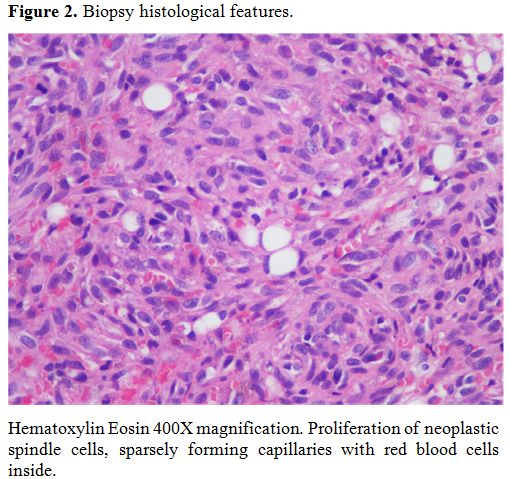
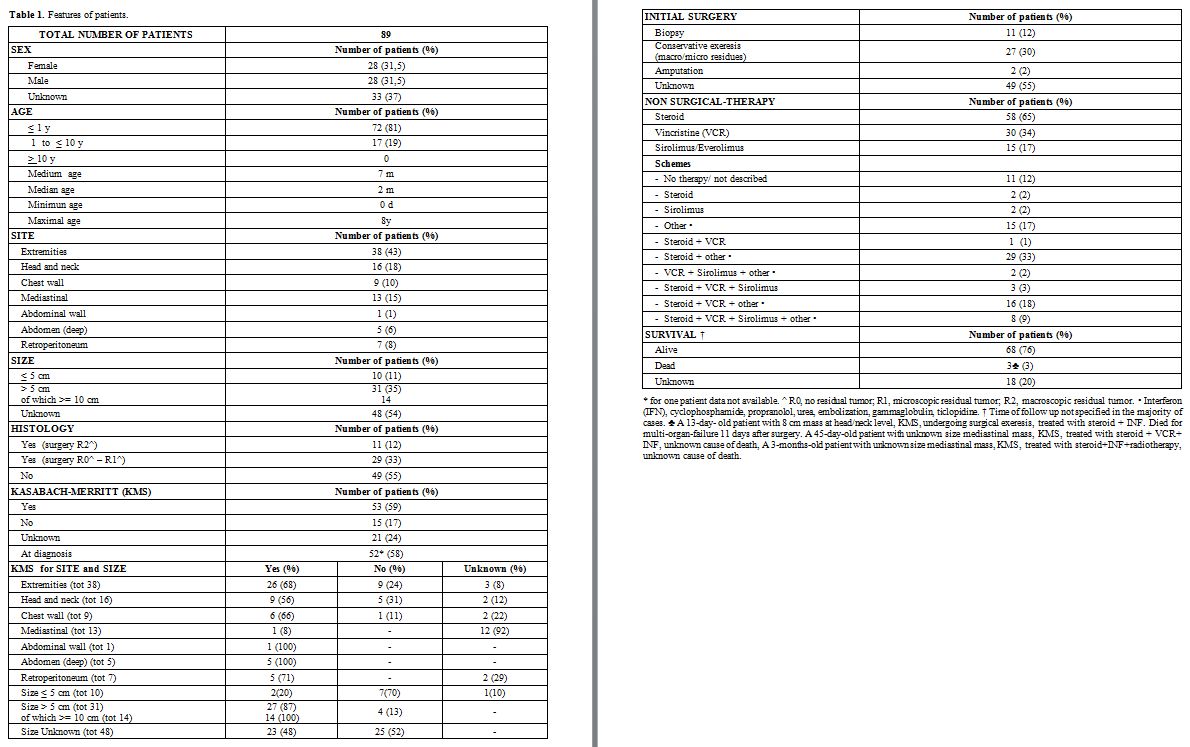
resonance imaging (MRI) (Figure 1). A biopsy was performed: the histological features (Figure 2)
and the immunophenotype with CD 31 (JC/70A) +, CD 34 (QBEND/10)+, GLUT1
-/+, PODOPLANIN (D2-40) +, PROTEIN S100 -, Herpes virus 8 (13B10) -
were diagnostic for KHE and the clinical and laboratory features were
indicative of KMS. The child started a 6-week therapy with prednisone
at the dose of 2 mg/kg/d (with a slow tapering), an 8-week course of
vincristine (0,05 mg/kg/week) associated with sirolimus (3 mg/m2),
modulated to maintain a blood concentration within the therapeutic
range of 7,5-10 ng/ml. During the following months, there was a
progressive clinical improvement with a 4 kg weight increase in 5
months. Platelet count increased to > 50 x109/L after 15 days of therapy and normalized (> 150 x109/L) after 4 months. As of 31st
January 2018, the patient was being treated with sirolimus for 20
months without any clinical or biochemical side effects or infection
complication. The MRI performed at 1, 9, 16 months showed a progressive
reduction of the mass (Figure 1).
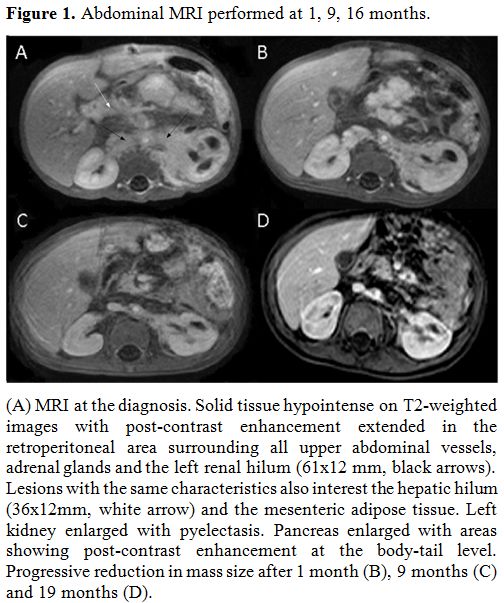 |
Figure 1.
Abdominal MRI performed at 1, 9, 16 months. |
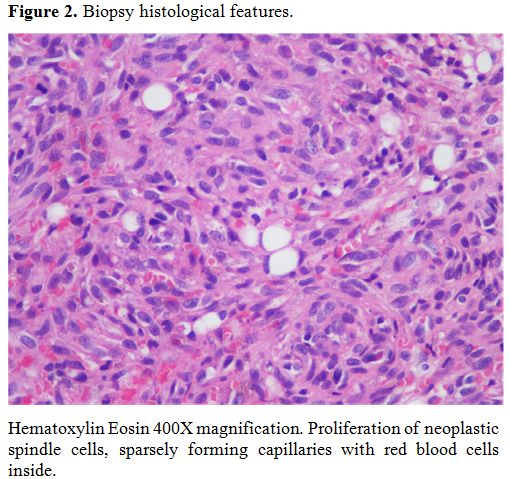 |
Figure 2. Biopsy histological features. |
Discussion
We report a case of KHE with KMS that
continues to respond to long-term treatment with sirolimus without side
effects. We performed a review of the literature of all cases of KHE in
patients under the age of 18 with the aim of defining typical
characteristics of the disease. We analysed 42 papers [1-3,8,9,11,12,15-49]
including case reports, brief reports, case series, consensus, clinical
letters, short communications, letters to the editor, retrospective
studies, reviews and research letters. Data are summarised in table 1.
The number of patients with KHE is 89 even if in 55% of cases the
diagnosis is not supported by the histology. The most frequent sites
are the extremities (43%). KMS is described in 59% of patients and it
always occurs in the abdominal sites (100%). In nearly all cases it is
already present at the diagnosis; when KMS is not present at the onset
the risk to develop it over time is low. Moreover, KMS occurs in 87% of
the masses > 5 cm and 100% of those > 10 cm, suggesting that
dimensions are related to the risk of developing KMS (Table 1).
No guideline has been defined, and different therapeutic medical and
surgical treatments have been used for KHE with and without KMS.
Radical surgery is one of possible treatment, and in cases of KMS it
can resolve the coagulopathy, but unfortunately, most of the lesions
are not surgically attackable, or they are only partially resectable.
Embolization and sclerotherapy are other techniques rarely used due to
the difficulty to cannulate small vessels and because of the risk of
complications.[3] Radiotherapy has proven to be effective, but it is limited by important side effects.[4,5]
Steroid therapy, even at high doses, is widely used for this type of
pathology and the literature data showed that 65% of the patients took
a steroid (table 1). The most
commonly used steroid is methylprednisolone (dose of 2 mg/kg/day)
followed by prednisone and dexamethasone. This therapy often gives good
results, but it is burdened by significant side effects especially when
used for long time.[21,24,31,49]
Vincristine is an effective chemotherapeutic drug, administered once a
week at a dosage of 0.05 mg/kg/dose. Vincristine has been used in 34%
of patients especially in association with steroid therapy in patients
with KMS. Vincristine resulted effective although the complete
remission was rare and the duration of therapy is limited by side
effects.[6,7,8] Propranolol has been shown to be effective in the treatment of KHE,[9] but the use in monotherapy is not able to control the disease.[3] Interferon, antiangiogenic drugs such as bevacizumab[10] and aspirin[11]
have been tested. Sirolimus is a mTOR inhibitor that is a
serine/threonine kinase regulated by phosphoinositide-3-kinase. It is
an important therapeutic option that has been increasingly used in the
last few years. It affects cell growth and angiogenesis; it is also a
powerful immunosuppressor and an antitumoral drug.[1,12] In multiple studies the effectiveness of the use of Sirolimus and other mTOR inhibitor has been described,[3,12,13,14]
proving to be particularly active in vascular and lymphoproliferative
disorders. Moreover, the mTOR inhibitors can be used in monotherapy
even for long periods, being able to control cases of the
non-completely regressed disease, and in spite of the necessity of
constant control of blood levels, they resulted manageable and with
little side effect. Literature data reported in table 1
show that 17% of patients received mTOR inhibitors, especially as
second-line therapy after the use of steroids, vincristine, and others.[8,19,20,21]
It has been administered for months every day, in some cases twice a
day, modulating the dose according to blood concentration (range 7-10
ng / ml).[1,3,8,12,16,19,20,21,25,28,32,34,49] According to the data summarised in table 1, the
most used therapeutic schemes are: steroid + other (33%) and steroid +
vincristine + other (18%). In our case, the initial therapy of
vincristine and prednisone was combined with sirolimus to obtain a
regression of the KMS. Long-term therapy with sirolimus has shown to be
effective in controlling the disease without side effects.
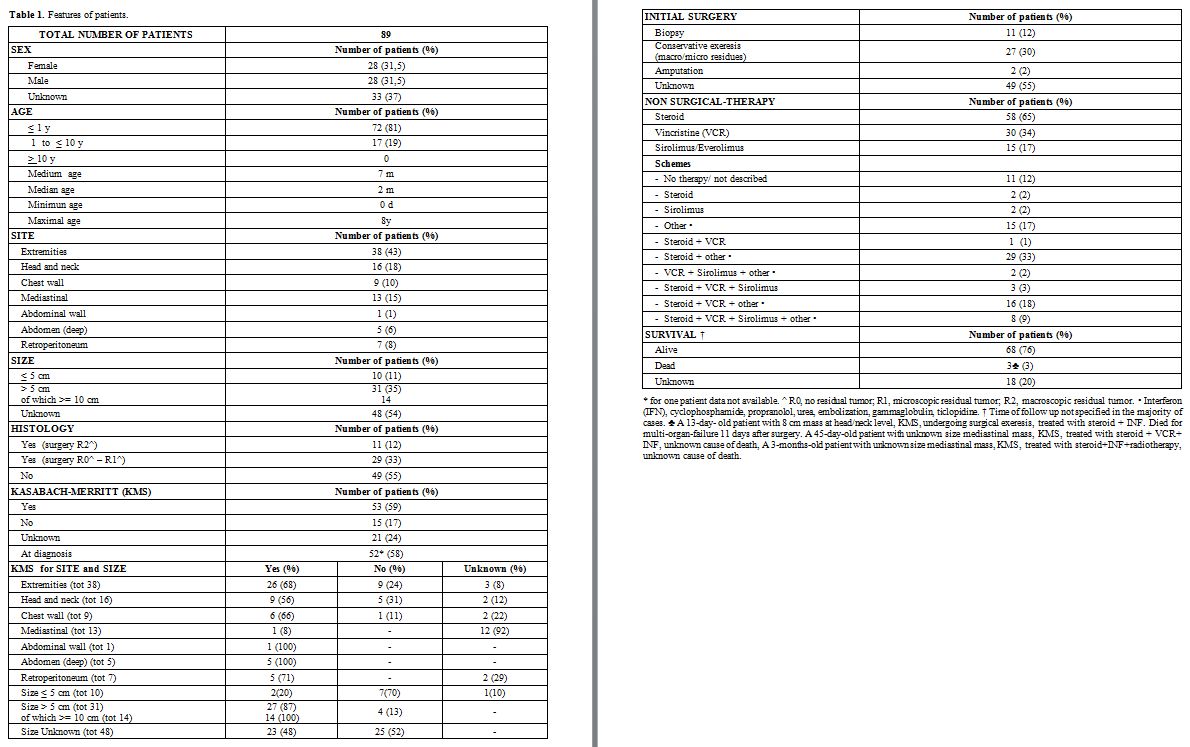 |
Table 1. Features of patients. |
Conclusions
KHE
is a locally aggressive tumor, and it is potentially life threatening
when associated with consumptive coagulopathy known as KMS. Although
there is no univocal consensus on the therapy, our case shows that in
cases of KHE with KMS a multidrug therapy (steroid + vincristine + mTOR
inhibitor) followed by maintenance with the mTOR inhibitor monotherapy
is a valuable option, with effective disease control and no relevant
side effects. Future studies are needed to validate this approach and
define the best duration of treatment.
References
- Uno T, Ito S, Nakazawa A, Miyazaki O, Mori T,
Terashima K. Successful treatment of kaposiform hemangioendothelioma
with everolimus. Pediatr Blood Cancer. 2015;62(3):536-538 https://doi.org/10.1002/pbc.25241

- Liu
Q, Jiang L, Wu D, Kan Y, Fu F, Zhang D, Gong Y, Wang Y, Dong C, Kong L.
Clinicopathological features of Kaposiform hemangioendothelioma. Int J
Clin Exp Pathol. 2015 Oct 1;8(10):13711-8. eCollection 2015.

- Chiu
YE, Drolet BA, Blei F, et al. Variable response to propranolol
treatment of kaposiform hemangioendothelioma, tufted angioma, and
Kasabach-Merritt phenomenon. Pediatr Blood Cancer. 2012;59(5):934-938. https://doi.org/10.1002/pbc.24103 PMid:22648868 PMCid:PMC3528889

- Wang
Z, Li K, Dong K, Xiao X, Zheng S. Refractory Kasabach-Merritt
phenomenon successfully treated with sirolimus, and a mini-review of
the published work. J Dermatol. 2015;42(4): 401-404. https://doi.org/10.1111/1346-8138.12797 PMid:25728547

- Kasabach HH, Merritt KK. Capillary hemangioma with extensive purpura: report of a case. Am J Dis Child. 1940; 59(5):1063-1070. https://doi.org/10.1001/archpedi.1940.01990160135009

- Fahrtash
F, McCahon E, Arbuckle S. Successful treatment of kaposiform
hemangioendothelioma and tufted angioma with vincristine. J Pediatr
Hematol Oncol 2010;32:506–510. https://doi.org/10.1097/MPH.0b013e3181e001a9 PMid:20523249

- Vivas-Colmenares
GV, Ramirez-VillarGL, Bernabeu-Wittel J,Matute de Cardenas JA,
Fernandez-Pineda I. The importance of early diagnosis and treatment of
kaposiform hemangioendothelioma complicated by Kasabach-Merritt
phenomenon. Dermatol Pract Concept. 2015;5(1):91-93. https://doi.org/10.5826/dpc.0501a18 PMid:25692091 PMCid:PMC4325701

- Jahnel
J, Lackner H, Reiterer F, Urlesberger B, Urban C. Kaposiform
hemangioendothelioma with Kasabach-Merritt phenomenon: from vincristine
to sirolimus. Klin Peadiatr. 2012;224(6):395-397. https://doi.org/10.1055/s-0032-1323823 PMid:23070861

- Filippi
L, Tamburini A, Berti E, Perrone A, Defilippi C, Favre C, Calvani M,
Della Bona ML, la Marca G, Donzelli G. Successful Propranolol Treatment
of a Kaposiform Hemangioendothelioma Apparently Resistant to
Propranolol. Pediatr Blood Cancer. 2016 Jul;63(7):1290-2. doi:
10.1002/pbc.25979. Epub 2016 Apr 21. https://doi.org/10.1002/pbc.25979

- O'Rafferty
C, O'Regan GM, Irvine AD, et al. Recent advances in the pathobiology
and management of Kasabach-Merritt phenomenon. Br J Haematol.
2015;171:38–51. https://doi.org/10.1111/bjh.13557 PMid:26123689

- MacFarland
SP, Sullivan LM, States LJ, Bailey LC, Balamuth NJ, Womer RB, Olson TS.
Management of Refractory Pediatric Kaposiform Hemangioendothelioma With
Sirolimus and Aspirin. J Pediatr Hematol Oncol. 2017 Dec 12. https://doi.org/10.1097/MPH.0000000000001046

- Blatt
J, Stavas J, Moats-Staats B, Woosley J, Morrell D. Treatment of
childhood kaposiform hemangioendothelioma with sirolimus. Pediatr Blood
Cancer. 2010;55(7):1396-1398. https://doi.org/10.1002/pbc.22766 PMid:20730884

- Fernandez-Pineda
I, Lopez-Gutierrez JC, Chocarro G, et al. Long-term outcome of
vincristine-aspirin-ticlopidine (VAT) therapy for vascular tumors
associated with Kasabach-Merritt phenomenon. Pediatr Blood Cancer.
2013;60:1478–1481. https://doi.org/10.1002/pbc.24543 PMid:23609996

- Matsumoto
H1, Ozeki M, Hori T, Kanda K, Kawamoto N, Nagano A, Azuma E, Miyazaki
T, Fukao T. Successful Everolimus Treatment of Kaposiform
Hemangioendothelioma With Kasabach-Merritt Phenomenon: Clinical
Efficacy and Adverse Effects of mTOR Inhibitor Therapy. J Pediatr
Hematol Oncol. 2016 Nov;38(8):e322-e325. https://doi.org/10.1097/MPH.0000000000000509 PMid:26907642

- Croteau
et al. Kaposiform hemangioendothelioma: atypical features and risks of
Kasabach-Merritt phenomenon in 107 referrals.J Pediatr. 2013 January;
162(1): 142 147. https://doi.org/10.1016/j.jpeds.2012.06.044 PMid:22871490 PMCid:PMC3494787

- Nakib
et al.Chemotherapy and Surgical Approach with Repeated Endovascular
Embolizations: Safe Interdisciplinary Treatment for Kasabach-Merritt
Syndrome in a Small Baby. Case Rep Oncol 2014;7:23–28 https://doi.org/10.1159/000357300 PMid:24575011 PMCid:PMC3934804

- Kim
et al.Excellent outcome of medical treatment for Kasabach-Merritt
syndrome: a single-center experience.Blood research 2016;51:256-60. https://doi.org/10.5045/br.2016.51.4.256 PMid:28090488 PMCid:PMC5234231

- Drolet
et al.Consensus-Derived Practice Standards Plan for Complicated
Kaposiform Hemangioendothelioma. Jpeds 2013;163;1:285-91. https://doi.org/10.1016/j.jpeds.2013.03.080 PMid:23796341

- Hammill et al.Sirolimus for the Treatment of Complicated Vascular Anomalies in Children.Pediatr Blood Cancer 2011;57:1018–1024 https://doi.org/10.1002/pbc.23124 PMid:21445948

- Reichel
et al.Kaposiform hemangioendothelioma with Kasabach-Merritt syndrome:
successful treatment with sirolimus. Deutsche Dermatologische
Gesellschaft (DDG) 2017;1610-0379/2017/1503:329-31.

- Alaqeel
et al.Sirolimus for treatment of kaposiform hemangioendothelioma
associated with Kasabach-Merritt phenomenon. Jaad case reports
2016;11:457-61. https://doi.org/10.1016/j.jdcr.2016.06.005 PMid:27981218 PMCid:PMC5148769

- Schaefer
et al.Long-term outcome for kaposiform hemangioendothelioma: A report
of two cases. Pediatr Blood Cancer 2017; 64: 284–2 https://doi.org/10.1002/pbc.26224 PMid:27701822

- Mac-Mourne
et al.Kaposiform Hemangioendothelioma: Five Patients with Cutaneous
Lesion and Long Follow-Up.Mod Pathol 2001;14(11):1087–1092 https://doi.org/10.1038/modpathol.3880441 PMid:11706068

- Pascal et al.Successful surgical management of congenital Kasabach–Merritt syndrome. Pediatrics International.2017;59:89–102 https://doi.org/10.1111/ped.13171 PMid:28102622

- Iacobas
et al.Decreased vascularization of retroperitoneal kaposiform
hemangioendothelioma induced by treatment with sirolimus explains
relief of symptoms.Clinical Imaging 39;2015:529–532 https://doi.org/10.1016/j.clinimag.2015.01.003 PMid:25662209

- Lackner
et al.Sirolimus for the treatment of children with various complicated
vascular anomalies.Eur J Pediatr. 2015 Dec;174(12):1579-84. https://doi.org/10.1007/s00431-015-2572-y PMid:26040705

- Wa
Due et al.Vascular tumors have increased p70 S6-kinase activation and
are inhibited by topical rapamycin.Laboratory Investigation.2013;93:
1115–1127 https://doi.org/10.1038/labinvest.2013.98 PMid:23938603

- Adams
et al.Efficacy and Safety of Sirolimus in the Treatment of Complicated
Vascular Anomalies.Pediatrics. 2016 Feb;137(2):e20153257. https://doi.org/10.1542/peds.2015-3257 PMid:26783326 PMCid:PMC4732362

- Shabtaie
et al.Neonatal Kaposiform Hemangioendothelioma of the Spleen associated
with Kasabach-Merritt Phenomenon.Journal of Pediatric Surgery 2016 https://doi.org/10.1016/j.jpedsurg.2016.03.014 PMid:27342010

- Adams
et al.Comment on: Steroid-Resistant Kaposiform Hemangioendothelioma: A
Retrospective Study of 37 Patients Treated With Vincristine and
Long-Term Follow Up.Pediatr Blood Cancer 2015;62:2056–2056 https://doi.org/10.1002/pbc.25609 PMid:26052679

- Wang
et al.Steroid-Resistant Kaposiform Hemangioendothelioma: A
Retrospective Study of 37 Patients Treated With Vincristine and
Long-Term Follow-up.Pediatr Blood Cancer 2015;62:577–580 https://doi.org/10.1002/pbc.25296 PMid:25346262

- Wang
et al.Variable Response to Propranolol Treatment of Kaposiform
Hemangioendothelioma, Tufted Angioma, and Kasabach–Merritt
Phenomenon.Pediatr Blood Cancer 2014;61:1518–1519 https://doi.org/10.1002/pbc.24957 PMid:24482015

- Wallenstein
et al.Mediastinal Kaposiform Hemangioendothelioma and Kasabach Merritt
Phenomenon in a Patient with no Skin Changes and a Normal Chest CT,
Pediatric Hematology and Oncology, Early Online:1–5, 2013

- Chan et al. Rapidly Enlarging "Bruise" on the Back of an Infant.JAMA Dermatology;2013;149;11:1337-8. https://doi.org/10.1001/jamadermatol.2013.519 PMid:24005816

- Mahotra
et al. Congenital Kaposiform Hemangioendothelioma with Kasabach Merritt
Phenomenon Successfully Treated with Low-Dose Radiation
Therapy.Pediatric Dermatology 2014;31; 5 595–598.

- Garcia-Monaco
et al.Kaposiform Hemangioendothelioma with Kasabach-Merritt Phenomenon:
Successful Treatment with Embolization and Vincristine in Two Newborns.
J Vasc Interv Radiol 2012; 23:417–422. https://doi.org/10.1016/j.jvir.2011.12.007 PMid:22365299

- Brabash-Neila
et al.Kaposiform Hemangioendothelioma with Kasabach-Merritt phenomenon:
Successful Treatment with Vincristine and Ticlopidine.Indian J Pediatr
(October 2012) 79(10):1386–1387 https://doi.org/10.1007/s12098-011-0625-4 PMid:22161581

- Jiang
et al.Successful treatment of Kasabach–Merritt syndrome arising from
kaposiform hemangioendothelioma by systemic corticosteroid therapy and
surgery.Int J Clin Oncol 2012 Oct, 17(5):512-6 https://doi.org/10.1007/s10147-011-0321-4 PMid:21947597

- Adams
et al. Vascular anomaly cases for the pediatric hematologist
oncologists—An interdisciplinary review. Pediatr Blood Cancer.
2017;e26716.

- Yasui
et al.Kasabach-Merritt Phenomenon: A Report of 11 Cases From a Single
Institution.J Pediatr Hematol Oncol 2013;35:554–558. https://doi.org/10.1097/MPH.0b013e318281558e PMid:23389504

- Bota et al.Infantile hemangiomas:a 7-year experience of a single-center.Clujul Medical 2017;.90;4: 396-400

- Kee Youn et al.Intestinal obstruction due to Kaposiform Hemagioendothelioma in a 1-month-old infant.Medicine;2017: 96:37

- Triana et al.Pancreatic Kaposiform Hemangioendothelioma Not Responding to Sirolimus.Eur J Pediatr Surg Rep 2017;5:e32–e35. https://doi.org/10.1055/s-0037-1604358 PMid:28761800 PMCid:PMC5533608

- Zhang
et al.Kaposiform haemangioendothelioma in a nine-year-old boy with
Kasabach–Merritt phenomenon.Br J Haematol. 2017 Oct;179(1):9. https://doi.org/10.1111/bjh.14837 PMid:28714059

- Wlodeck
et al.A case of kaposiform haemangioendothelioma successfully and
safely treated with sirolimus.Clin Exp Dermatol. 2017
Oct;42(7):825-827. https://doi.org/10.1111/ced.13168 PMid:28703334

- Tasani
et al.Sirolimus therapy for children with problematic Kaposiform
haemangioendothelioma and tufted angioma.Br J Dermatol. 2017
Dec;177(6):e344-e346. https://doi.org/10.1111/bjd.15640 PMid:28485019

- Alonso
Arroyo et al.Identical Presentation of Scapular Osteolysis in Two
Patients with Thoracic Kaposiform Hemangioendothelioma. Pediatric
Dermatology 2017;1-4"

- Sobrino-Fernandez et al.Kaposiform Hemangioendothelioma Presenting as Hydrops Fetalis.Pediatric Dermatology 2017;1-2 https://doi.org/10.1111/pde.13101

- Li
Kai et al.Sirolimus, a promising treatment for refractory Kaposiform
hemangioendothelioma.J Cancer Res Clin Oncol (2014) 140:471–476 https://doi.org/10.1007/s00432-013-1549-3 PMid:24464150

[TOP]