Maria Lucia De Luca1, Laura Lombardi2, Germana Tartaglia1, Francesca Fazio1, Alessio Di Prima1, Alessandra Serrao1, Martina Canichella1 and Alessandro Pulsoni1.
1 Division of Haematology, Department of Translational and Precision Medicine, Sapienza University of Rome, Italy.
2 Service D’Hématologie, Hôpital Simone Veil, Troyes, France.
Published: September 1, 2019
Received: May 23, 2019
Accepted: August 10, 2019
Mediterr J Hematol Infect Dis 2019, 11(1): e2019053 DOI
10.4084/MJHID.2019.053
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Many
epidemiological, biological and therapeutic studies have extensively
investigated the etiological link between HCV infection and B-cell
Non-Hodgkin Lymphoma (NHL).
Large experiences in the literature
demonstrated HCV-related indolent NHL regression after antiviral
therapy. While the response to interferon-ribavirin-based antiviral
therapy is well documented, evidence of the efficacy of interferon-free
Direct-Acting Antivirals (DAAs) in this subset of lymphoma is also
currently increasing. Splenic and Nodal Marginal zone Lymphoma (MZL)
are frequently associated with HCV chronic infection. In this article
we report two cases of HCV-related MZL with an unusual presentation,
subcutaneous “lipoma-like” nodules, treated with DAAs. Both patients, a
59-years-old woman and a 72-years-old man, were affected by HCV chronic
infection since several years and were referred to our Institute for a
diagnosis of MZL with subcutaneous presentation. Given the possible
etiological link with HCV infection, both patients were treated with
DAAS.
A Sustained virological response (SVR) was reached after few
weeks of therapy and at the end of treatment a clinically and
radiologically documented reduction of MZL localizations, persisting to
date, were obtained in both patients. The two clinical cases presented
in this article confirm the efficacy of DAA’s as first-line treatment
in HCV related NHL, also in this rare entity of MZL with subcutaneous
presentation.
|
Introduction
HCV
infection affects over 180 million people all over the world and Italy
is one of the countries with the highest prevalence (> 3%). The most
common genotype in the world is genotype 1 (46% of global infections)
followed by genotype 3 (22%) and genotype 2 and 4 (13% each).[1]
Large evidences in literature suggest the association between chronic
HCV infection and B-cell-non-Hodgkin’s lymphomas (NHL). In 2003 Mele et
al reported the incidence of 17.5% of NHL in HCV positive patients
compared to the 5.6% of controls.[2] The most likely
pathogenic mechanism of HCV-related NHL is the continuous chronic
stimulation of lymphocytes receptors by viral antigens which may induce
B cell proliferation and transformation in NHL.[3]
Marginal
zone lymphoma (MZL) is a low-grade B-Cell Non-Hodgkin Lymphoma whose
most frequent presentations are extranodal MZL of mucose-associated
lymphoid tissue (MALT), splenic MZL and nodal MZL. It is frequently
associated with an infectious etiology and among them, Hepatitis C
virus infection is implicated especially in the pathogenesis of splenic
and nodal MZL.[4]
Subcutaneous MZL is a rare presentation described in 2010 in 12 HCV chronically infected patients.[5]
This disease is characterized by solitary or multiple nodular MZL
lesions clinically resembling lipomas. No other similar cases were
subsequently described in the literature.
In the setting of HCV
related lymphoproliferative disorders, the antigen removal by antiviral
treatment represents the first-line therapeutic approach in indolent
forms not requiring an immediate chemo-immunotherapy approach,
achieving partial or complete regression of NHL.
Peg-Interferon +
Ribavirin has been the standard treatment of HCV-related indolent
lymphomas and many retrospective studies demonstrated B-NHL complete
(CR) or partial (PR) response after HCV eradication. Meta-analysis data
showed that lymphoma regression is related to the achievement of a
complete HCV-RNA clearance. In a retrospective study promoted by
Fondazione Italiana Linfomi (FIL), 100 patients with HCV-related NHL
treated with Peg-Interferon + Ribavirin were studied, demonstrating a
SVR rate of 80% with an overall hematological response rate of 77%.[6]
The introduction of direct-acting antivirals (DAAs) has changed the
treatment scenario for chronic HCV infection and extrahepatic
manifestations. Isolated case reports and a retrospective collection of
46 cases demonstrated the possibility of complete or partial regression
after DAAs therapy in HCV-related lymphoproliferative disorders.[7]
Here we describe two cases of response of subcutaneous MZL with lipoma-like presentation after DAAs treatment.
Case Presentation
The
first case concerns a 59-year-old woman affected by chronic HCV
infection (genotype 1b) since 2007. In January 2008 the patient started
alpha-Interferon therapy, suspended after 6 months for subclinical
thyroiditis, obtaining a partial response of HCV infection. In May 2014
the patient developed right gluteus and right intercostal palpable soft
nodules of 7 and 3 cm of diameter respectively. Ultrasound showed
hypoechoic nodular lesions with intrinsic vascularization. A biopsy
specimen of the right intercostal nodule revealed a subcutaneous MZL.
The lymphoma cells were CD20 +, CD5-, annexin 1-, BCL1-, BCL6-, CD10-,
with low proliferative Ki67/MIB-1 index. The same histology was found
in the bone marrow. MR and PET/CT scans showed multiple subcutaneous
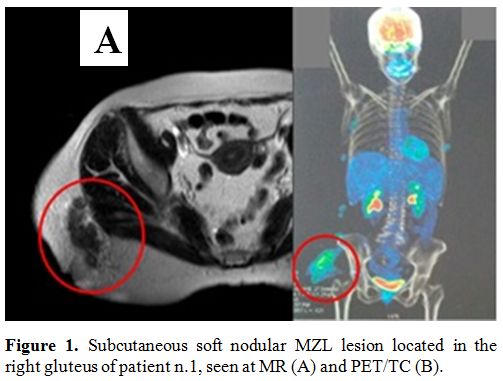
localizations in the right gluteus (SUV max 6, diameter 6 cm, figure 1A and 1B)
and right intercostal region (SUV max 4, diameter 4 cm) without any
lymph node and /or splenic involvement. At the time of lymphoma’s
diagnosis, HCV-RNA was 346.143 UI/mL.
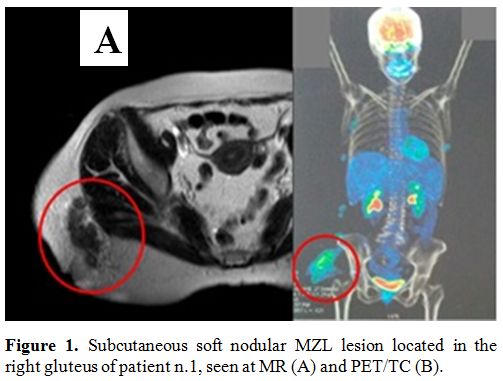 |
Figure 1. Subcutaneous soft nodular MZL lesion located in the right gluteus of patient n.1, seen at MR (A) and PET/TC (B). |
Supposing
an etiological link between HCV infection and MZL, even if in a rare
presentation, the patient received DAAs treatment with sofosbuvir (400
mg/day) and ribavirin (1000 mg/day) for 24 weeks from November 2014.
HCV-RNA decreased rapidly after only one month and during the
treatment, a progressive clinical reduction of the palpable
subcutaneous nodules was observed. Six months after the end of the
antiviral treatment, PET/CT scan showed a reduced FDG uptake (SUV max
2.5) and size of MZL localizations described at the onset (right
gluteus 4.5 cm, right intercostal region 1 cm) while HCV-RNA remained
undetectable in the serum. After 22 months, the patient developed a new
lesion of the right leg with a similar aspect (soft palpable
subcutaneous lesion) but with inflammatory features (painful, with
cutaneous warmth and redness). Unfortunately, a biopsy was not
performed, but the lesion regressed after two weeks of oral steroid
treatment. At present, the patient maintained the lymphoma’s partial
response (PR) with persistent small asymptomatic subcutaneous nodules
42 months after the end of DAAs treatment while in SVR and has never
yet received specific treatment for MZL.
The second patient, a
72-year-old man, was affected by HCV infection since 1998 (genotype
2a/2c) but at that time he did not receive any treatment for HCV
infection because of no evidence of active hepatitis. On November 2015
the patient presented multiple subcutaneous palpable nodular lesion in
the left lumbar region (diameter 11 cm), in the right gluteus (diameter
1,4 cm), in the right leg (3,6 cm,) and in the left popliteal region
(diameter 2,5 cm). On Ultrasound, these nodular lesions were described
as hypoechoic with inhomogeneous echostructure and vascularization. A
biopsy specimen on the right leg nodule documented a subcutaneous MZL.
The lymphoma cells were CD20+, CD79+, BCL2, BCL6-/+, CD10-, CD3-, CD5-,
CD23-, cyclin D-, with a low ki67/MIB-1 index. Bone marrow histology
did not document a lymphoma infiltration. When the patient was referred
to our center, HCV-RNA was 1.263.000 UI/ml without signs or symptoms of
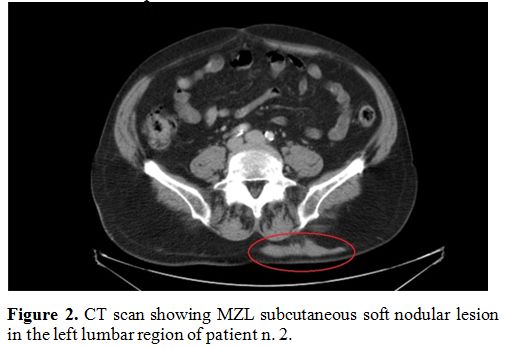
liver cirrhosis. A CT scan documented the subcutaneous nodules (Figure 2)
excluding any other involvement. The patient received treatment with
sofosbuvir (400 mg/day) and ribavirin (1000 mg/day) for six months. On
May 2016, the end therapy revaluation showed SVR, and a partial
response of the lymphoma with a >50% reduction of the nodules
evaluated both clinically and by ultrasound and CT. Periodical imaging
and blood tests confirmed the MZL PR in the absence of symptoms with
persisting SVR after 30 months. At present, in both patients, a
specific chemo-immunotherapy treatment was never performed while
continuing a watch and wait policy.
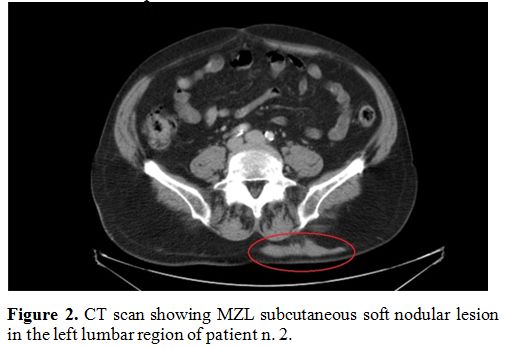 |
Figure 2. CT scan showing MZL subcutaneous soft nodular lesion in the left lumbar region of patient n. 2. |
Both patients signed informed consent to their data publication and collaborated in diagnostic imaging production.
Discussion
Our
report describes two cases of HCV-related subcutaneous MZL with the
lipoma-like presentation, a probably underdiagnosed entity.
Clinical
presentation of subcutaneous MZL is similar to lipomas and therefore
can be underestimated. Ultrasound characterization of lipomas is
typical of benign solid masses: they appear well-circumscribed with
variable echogenicity and absent or poor vascularization.[8]
In
our two patients, nodular subcutaneous lesions, even if clinically
comparable to lipomas, showed dubious ultrasound features such as
inhomogeneous echostructure and increased blood flow on color doppler.
Therefore,
in the case of nodular lesions similar to lipomas, an ultrasound is
mandatory to evaluate the presence of echographic characteristics of
benignity. Any lesion with dubious ultrasound features must be
investigated with HCV testing, second-level imaging, and histological
characterization.
Although based on only two cases, our
experience suggests that the use of DAAs is a valid first-line
therapeutic approach also in this rare presentation of HCV related MZL,
showing excellent tolerability as well as high and persistent
anti-lymphoma effect. A chemo-immunotherapy approach should be only
considered in case of the clinical need for immediate treatment or no
response to DAAs.
References
- Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi
H. Global epidemiology and genotype distribution of the hepatitis C
virus infection. J Hepatol. 2014 Nov;61(1 Suppl):S45-57 https://doi.org/10.1016/j.jhep.2014.07.027 PMid:25086286
- Mele
A, Pulsoni A, Bianco E, Musto P, Szklo A, Sanpaolo MG, Iannitto E, De
Renzo A, Martino B, Liso V, Andrizzi C, Pusterla S, Dore F, Maresca M,
Rapicetta M, Marcucci F, Mandelli F, Franceschi S. Hepatitis C virus
and B-cell non-Hodgkin lymphomas: an Italian multicenter case-control
study. Blood. 2003 Aug 1;102(3):996-9 https://doi.org/10.1182/blood-2002-10-3230 PMid:12714514
- Peveling-Oberhag
J, Arcaini L, Hansmann ML, Zeuzem S. Hepatitis C-associated B-cell
non-Hodgkin lymphomas. Epidemiology, molecular signature and clinical
management. J Hepatol. 2013 Jul;59(1):169-77 https://doi.org/10.1016/j.jhep.2013.03.018 PMid:23542089
- Perrone
S, D'Elia GM, Annechini G, Pulsoni A. Infectious Aetiology of Marginal
Zone Lymphoma and Role of Anti-Infective Therapy. Mediterr J Hematol
Infect Dis. 2016 Jan 1;8(1):e2016006. doi: 10.4084/MJHID.2016.006. https://doi.org/10.4084/mjhid.2016.006 PMid:26740867 PMCid:PMC4696464
- Paulli
M, Arcaini L, Lucioni M, Boveri E, Capello D, Passamonti F, Merli M,
Rattotti S, Rossi D, Riboni R, Berti E, Magrini U, Bruno R, Gaidano G,
Lazzarino M. Subcutaneous 'lipoma-like' B-cell lymphoma associated with
HCV infection: a new presentation of primary extranodal marginal zone
B-cell lymphoma of MALT. Ann Oncol. 2010 Jun;21(6):1189-95 https://doi.org/10.1093/annonc/mdp454 PMid:19858084
- Arcaini
L, Vallisa D, Rattotti S, Ferretti VV, Ferreri AJ, Bernuzzi P, Merli M,
Varettoni M, Chiappella A, Ambrosetti A, Tucci A, Rusconi C, Visco C,
Spina M, Cabras G, Luminari S, Tucci M, Musto P, Ladetto M, Merli F,
Stelitano C, d'Arco A, Rigacci L, Levis A, Rossi D, Spedini P, Mancuso
S, Marino D, Bruno R, Baldini L, Pulsoni A. Antiviral treatment in
patients with indolent B-cell lymphomas associated with HCV infection:
a study of the Fondazione Italiana Linfomi. Ann Oncol. 2014
Jul;25(7):1404-10. https://doi.org/10.1093/annonc/mdu166 PMid:24799461
- Arcaini
L, Besson C, Frigeni M, Fontaine H, Goldaniga M, Casato M, Visentini M,
Torres HA, Loustaud-Ratti V, Peveling-Oberhag J, Fabris P, Rossotti R,
Zaja F, Rigacci L, Rattotti S, Bruno R, Merli M, Dorival C, Alric L,
Jaccard A, Pol S, Carrat F, Ferretti VV, Visco C, Hermine O.
Interferon-free antiviral treatment in B-cell lymphoproliferative
disorders associated with hepatitis C virus infection. Blood. 2016 Nov
24;128(21):2527-2532. https://doi.org/10.1182/blood-2016-05-714667 PMid:27605512
- DiDomenico
P, Middleton W. Sonographic evaluation of palpable superficial masses.
Radiol Clin North Am. 2014 Nov;52(6):1295-305. doi:
10.1016/j.rcl.2014.07.011. Epub 2014 Nov 4. Review. https://doi.org/10.1016/j.rcl.2014.07.011 PMID: 25444107.