Khaldoun Masoud1*, Rima Hanna-Wakim1,2*, Hassan Zaraket1,3*, Samer Kharroubi4, George F Araj1,5, Ghassan M Matar1,3 and Ghassan Dbaibo1, 2 .
1 The Center for Infectious Diseases Research, American University of Beirut, Beirut, Lebanon.
2 Department of Pediatrics and Adolescent Medicine, American University of Beirut, Beirut, Lebanon.
3 Department of Experimental Pathology, Immunology and Microbiology, American University of Beirut, Beirut, Lebanon.
4
Department of Nutrition and Food Sciences, Faculty of Agricultural and
Food Sciences, American University of Beirut, Beirut, Lebanon
5
Department of Pathology and Laboratory Medicine, American University of
Beirut, Beirut, Lebanon. *Authors participated equally in this work
*Authors participated equally in this work
Correspondence to: Project Investigator, Pr. Ghassan Dbaibo. The Center
for Infectious Diseases Research, American University of Beirut,
Beirut, Lebanon. E-mail:
gdbaibo@aub.edu.lb
Published: November 1, 2019
Received: June 24, 2019
Accepted: September 25, 2019
Mediterr J Hematol Infect Dis 2019, 11(1): e2019059 DOI
10.4084/MJHID.2019.059
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background: Acute
respiratory infections (ARI) are the leading cause of death worldwide,
especially among children. The majority of these infections in children
are of viral etiology. In this study, we evaluated the incidence of
viral ARI among children in Lebanon.
Patients and Methods:
Children presenting with symptoms of ARI were prospectively recruited
between September 2009 to February 2012. Nasopharyngeal aspirates were
obtained from patients and screened for 11 respiratory viruses using a
multiplex Luminex-based PCR assay.
Results:
Two hundred twenty-one patients were recruited with a median age of 1
year (IQR: 0 - 5). Out of 221 patients, 116 (52.5%) were positive for
at least one virus, the majority (103/116; 88.8%) of which were in
children under 6-year of age. Overall, 188 viruses were detected.
Rhinovirus (RhV) was the most common virus detected in 81 (69.8%)
patients followed by coxsackie virus and echovirus (CVEV) which were
detected as one target in the panel in 45 (38.8%), and parainfluenza
viruses (PIV types: 1, 2, 3, 4) in 24 (20.7%) patients. Coinfection
with more than one virus was detected in 49 (42.9%) patients. RhV and
CVEV were the most common viruses associated with co-infections and
higher risk of rhinorrhea.
Conclusions: Viral pathogens account for at least half of the ARIs in Lebanon, with a high frequency of co-infections being detected.
|
Introduction
Acute respiratory tract infections (ARIs) are among the most common reasons for primary care consultations.[1]
The World Health Organization (WHO) ranks ARIs as the fourth major
killer after cardiovascular diseases, general infections, parasitic
diseases, and cancer.[2] ARIs cause 4 million deaths
globally. The burden is especially high in children where ARIs are
responsible for 11-22% of deaths.[3] ARIs can lead to severe complications requiring hospitalizations and can have fatal outcomes.[4,5]
Viruses
are the most common etiology of ARIs in children.[6,7] These include
rhinovirus (RhV), respiratory syncytial virus (RSV), influenza (IFN),
parainfluenza virus (PIV), coronavirus (CoV), human metapneumovirus
(hMPV), enteroviruses (EV), adenovirus (AdV), and human bocavirus
(HBoV).[6,8,9] Each of these viruses poses a significant health burden.
Nair et al. estimated that 111 500 deaths in children <5 years were
attributable to influenza-associated lower respiratory tract infections
(LRI) in 2008, the vast majority of which occurred in developing
countries.[9] A study by Fendrik et al. estimated the
total economic impact of non-influenza-related viral RTIs in the United
States at $40 billion annually.[10] RSV was estimated to have caused 33.8 million LRI
episode in children under five, of which 3.4 million were severe
causing up to 199 000 deaths.[11] In addition to the health burden of
viral respiratory tract infections (RTIs), the economic impact is also
high if we account for health care costs (direct cost) and loss of
productivity (indirect cost). [12]
The advancements that have
been achieved in developing antiviral drugs, some of which have already
been approved, against respiratory viruses allow for targeted therapy
of viral ARIs.[13-15] This possibility calls for better and faster
diagnosis of the etiologic agents in ARI patients to benefit from the
full potential of these drugs.[6]
Furthermore, ARIs are
associated with the greatest amount of excess use of antibiotics that
has led to unprecedented increase in antimicrobial drug
resistance;[16] therefore, proper and timely diagnosis of viral
infections can help reduce unnecessary antibiotic prescriptions.[5,6]
In
Lebanon, studies investigating the viral etiologies of ARIs are very
scarce. In this study, we determined the viral etiologies among ARI
patients at a tertiary care hospital that serves an ethnically and
socio-economically diverse patient population.
Materials and Methods
Patients and samples collection.
Infants and children younger than 18 years of age with symptoms of ARI
disease presenting to the emergency department or the departments of
pediatrics of the American University of Beirut Medical Center (AUBMC),
Beirut, Lebanon were prospectively recruited between September 2009 to
February 2012. An ARI was defined as an acute infection of the upper
and lower respiratory airways. Recruited patients had one or more of
the following symptoms: fever, cough, sore throat, rhinorrhea,
headache, conjunctivitis, wheezing, dyspnea, and vomiting.
Medical
history and demographic data were obtained from the patients and their
medical records. A respiratory sample was collected and stored at -80°C
for viral assessment. The study was approved by the Institutional
Review Board (IRB) of the AUBMC, and written informed consent was
obtained from all parents.
Nucleic acid extraction and viral
detection. Nucleic acid was extracted from clinical specimens by using
the QIAamp MinElute Virus Spin kit (Qiagen) according to the
manufacturer’s protocol. A 200 µl aliquot of each specimen was used for
nucleic extraction. Specimens were then analyzed by the ResPlex II
panel (Qiagen) using the manufacturer’s protocol.
The ResPlex II
panel can detect 11 viral targets: RSVA, RSVB, INFA, INFB, PIV1, PIV2,
PIV3, PIV4, hMPV, CVEV (coxsackie virus and echovirus), and RhV.
Briefly, 10 µl of each specimen were added to 40 µl reverse
transcription-PCR (ResPlex II) master mix, including the supplied
primers. Targets were detected by mixing 5 µl portions of amplification
products with ResPlex II bead in hybridization buffer at 52°C for10
min. Streptavidin-phycoerythrin conjugate was added, and mixtures were
incubated at 52°C for a further 5 min before the addition of stop
buffer. The samples were then analyzed on a Luminex Bio-Rad BioPlex 200
System (Bio-Rad Laboratories) using Bio-Rad BioPlex Manager software.
The cutoff value for each target was determined, as previously
described by Li et al.[17]
Statistical analysis.
The data were checked for completeness, and responses were coded and
entered into the Statistical Package for the Social Sciences (SPSS)
software version 23 for Windows, which was later used for statistical
analyses.[32] Descriptive statistics were presented to summarize the
study variables of interest as counts and percentages for the
categorical variables and as medians and Interquartile Range (IQR) for
the continuous ones. The Chi-square test was used to calculate the
association between two categorical variables. Pearson's chi-square
analysis with Bonferroni-Holm p-value correction was used for multiple
comparisons to assess infectivity enhancing correlations. Univariate
and multivariate logistic regression analyses were applied to determine
which factors are associated with rhinorrhea. In the regression model,
rhinorrhea was used as the dependent variable. Odds ratios and their
respective 95% confidence intervals were calculated. For all analysis
done, a p-value of less than 0.05 was considered statistically
significant.
Results
Patient characteristics.
A total of 221 specimens were collected from children presenting with
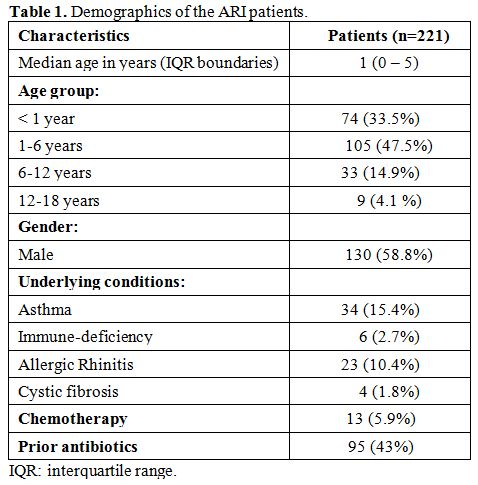
symptoms of ARI between September 2009 and February 2012 (Table 1). The socio-demographic characteristics of the study patients are presented in Table 1.
Overall, the study consisted of 130 males (58.8%) and 91 females
(41.2%) with patients’ median age of 1 (IQR: 0 - 5) years. Seventy-four
patients (33.5%) were children under one year of age, 105 (47.5%) were
between 1 to 6 years old, 33 (14.9%) were 6 to 12 years old, and 9
(4.1%) were 12 to 18 years old. Sixty-seven (30.3%) of the children had
an underlying disease (asthma, immune-deficiency, allergic rhinitis, or
cystic fibrosis). At the time of diagnosis 13 (5.8%) patients were
receiving chemotherapy, and 95 (43%) had received an antibiotic.
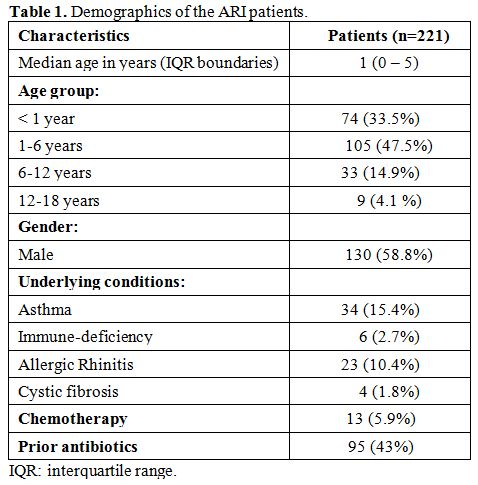 |
Table 1. Demographics of the ARI patients. |
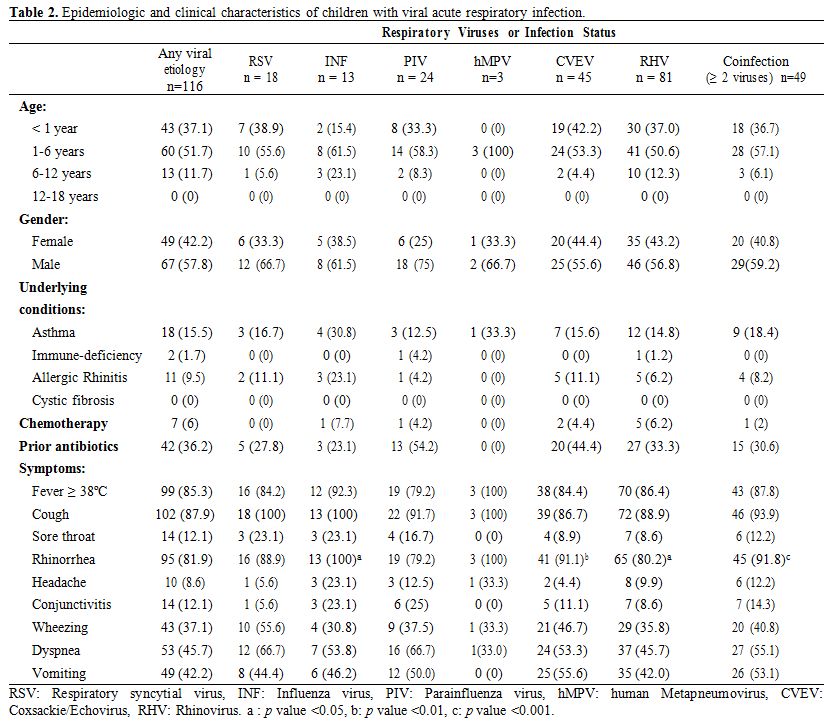
Virological characterization.
Samples were screened for 11 virus targets included in the ResPlexII
respiratory panel. Of the 221 ARI episodes, 116 (52.5%) were confirmed
to be of viral etiology being positive for at least one of the virus
targets tests (Table 2). The majority (n=103; 88%) of viral ARI episodes were observed in children under 6-year of age (chi-square, p<0.05).
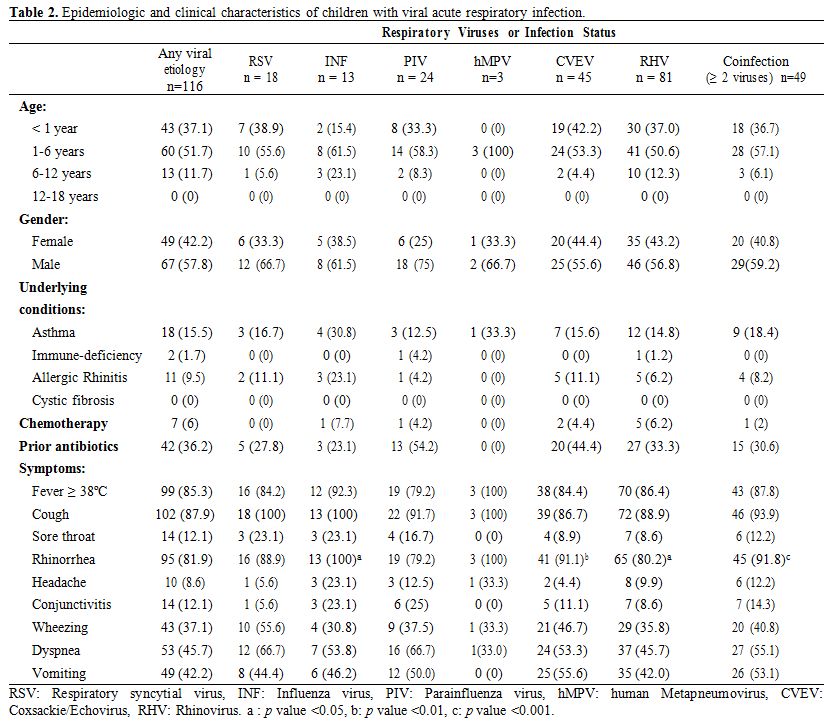 |
Table 2. Epidemiologic and clinical characteristics of children with viral acute respiratory infection. |
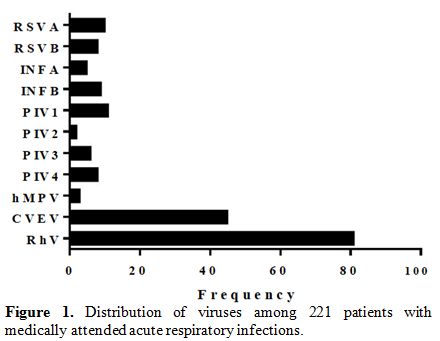
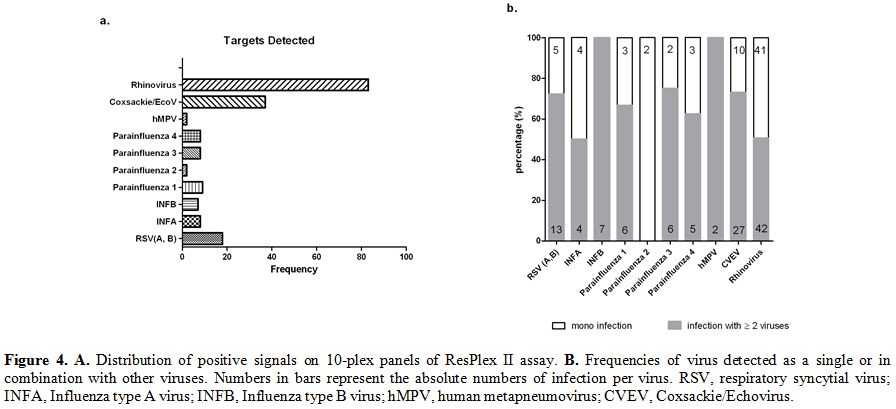
Figure 1
shows the frequency of each of the viruses detected in the study
population. Overall 188 viruses were detected. Rhinovirus (RhV) was the
most common virus detected in 81 (69.8%) patients followed by coxsackie
virus and echovirus (CVEV) which were detected as one target in the
panel in 45 (38.8%) patients, parainfluenza viruses (PIV types: 1, 2,
3, 4) in 24 (20.7%) and respiratory syncytial virus (RSV types A and B)
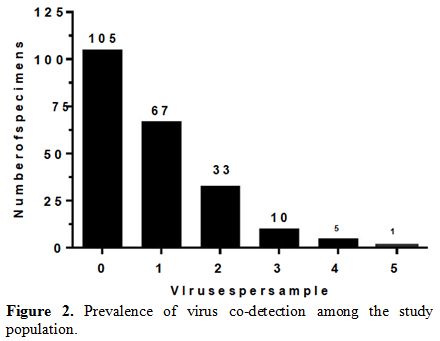
in 18 (15.5%). Coinfection with more than one virus was detected in 49
(42.9%) patients (Figure 2). A
significant majority (n=46; 93.9%; chi-square p-value<0.05) of
coinfections occurred in children under six years of age. The most
frequent viral co-infections involved two viruses (n=33), 10 cases had
a triple infection, 5 had four viruses detected, and one case had five
viruses. Almost half cases of Rhinovirus (50.6%) were positive for at
least another virus in the panel. CVEV positive cases also had a high
rate of co-infection (73%). Moreover, hMPV and INFB were detected in 9
samples, and all were co-infected.
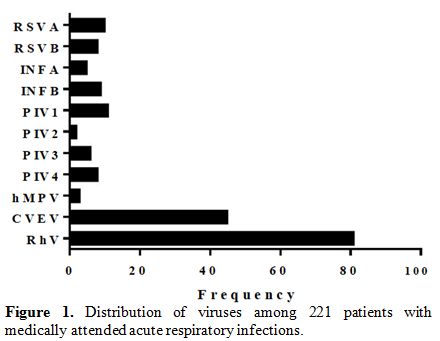 |
Figure 1. Distribution of viruses among 221 patients with medically attended acute respiratory infections. |
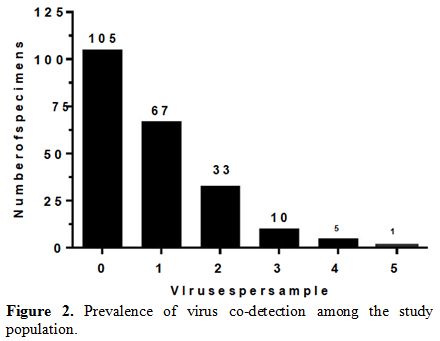 |
Figure 2. Prevalence of virus co-detection among the study population. |
Table 3
summarizes the correlation of different viruses among our patients.
Several correlations enhancing infectivity were evident in our
analysis. Of note, RhV was the most frequently detected virus in
co-infections and was significantly associated with RSVB, INFB, PIV3,
hMPV, and CVEV.
 |
Table 3. Cross-tabulation of the virus frequency among ARI patients. |
Underlying conditions and clinical presentation. We next analyzed the correlation between each of the viral etiologies or co-infection with the underlying conditions (Table 2).
To simplify the analysis, we treated subtypes or genotypes of a virus
as a single group (e.g. RSV for RSVA and RSVB, etc.). Having an
underlying condition or receiving chemotherapy or a course of
antibiotics were not found to be a risk factor for having a viral
etiology or co-infection (Table 2).
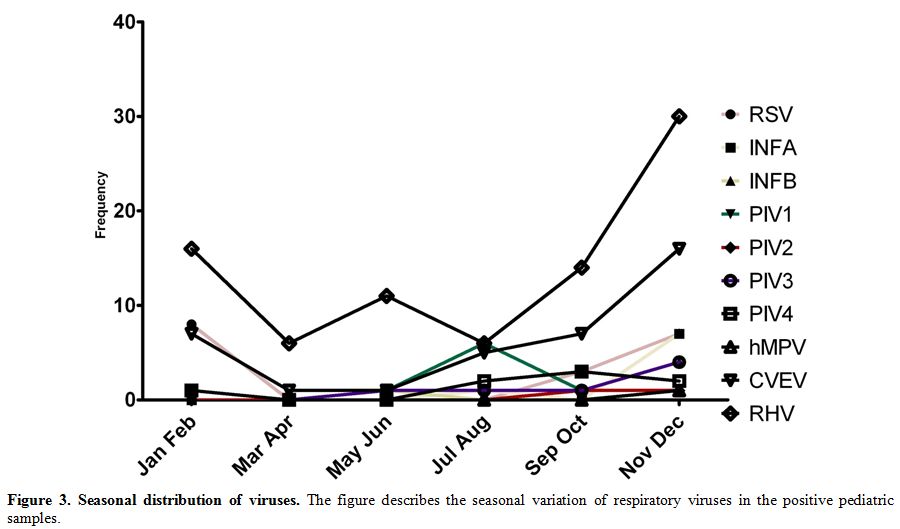
Additionally, we investigated the seasonal variation of viruses.
Rhinovirus infections were detected throughout the year however the
peak rate occurred during the main rainy months (November, December),
likely for Coxsackie/Echovirus and RSV. On the other hand, Influenza A
virus infections had a peak in the fall (September, October); (Figure 3).
In terms of clinical symptoms, fever, cough and rhinorrhea were major
symptoms observed in most of the patients infected with one or more
respiratory virus (Table 2). Chi-square analysis revealed a significant correlation between rhinorrhea and INF, CVEV, and RhV and co-infection (Table 2).
Bivariate logistic regression was then performed to determine the risk
associated with these infections. Our analysis revealed that RhV or
CVEV infected patients or patients infected with more than one virus
were more likely to have rhinorrhea (OR for RhV: 2.25; CI: 1.18 - 4.31;
OR for CVEV: 5.57; CI: 1.90 – 16.28; OR for co-infection: 6.34; CI:
2.17-18.44).
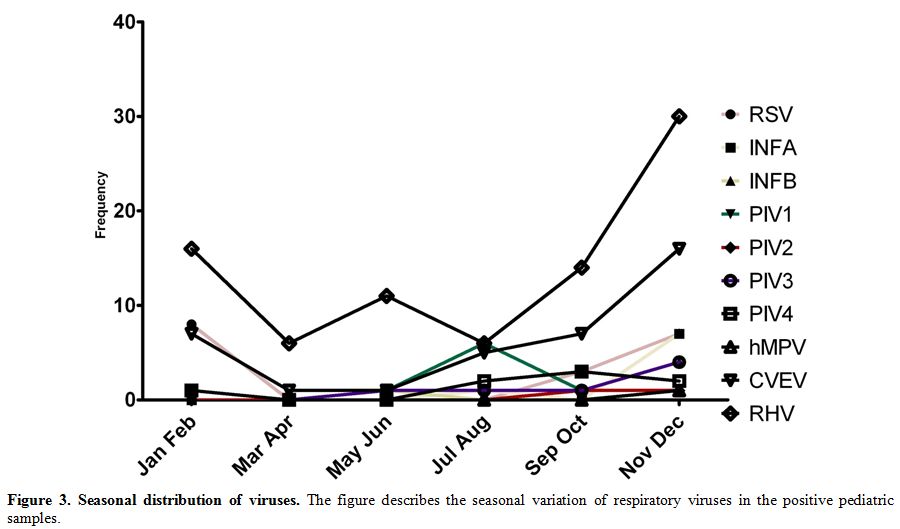 |
Figure 3. Seasonal distribution of
viruses. The figure describes the seasonal variation of respiratory
viruses in the positive pediatric samples. |
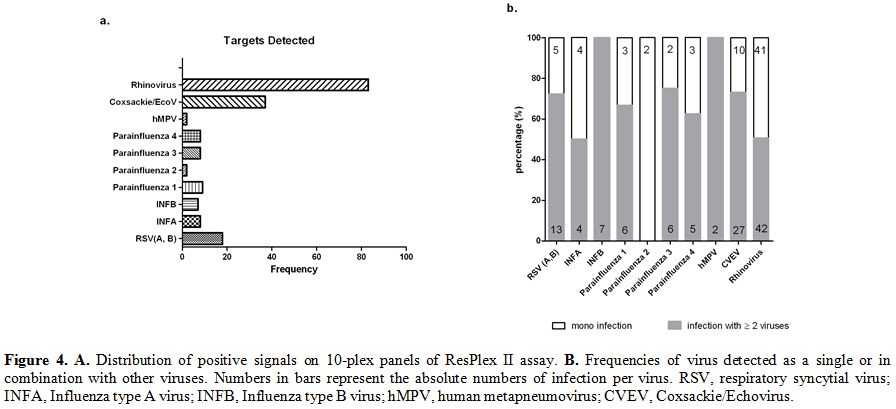 |
Figure 4. A. Distribution
of positive signals on 10-plex panels of ResPlex II assay. B.
Frequencies of virus detected as a single or in combination with other
viruses. Numbers in bars represent the absolute numbers of infection
per virus. RSV, respiratory syncytial virus; INFA, Influenza type A
virus; INFB, Influenza type B virus; hMPV, human metapneumovirus; CVEV,
Coxsackie/Echovirus. |
.A
multivariate logistic regression model was used to examine the
correlates of rhinorrhea in the study patients. Variables were put in
the model in order of strength of their correlation with rhinorrhea as
per the bivariate analysis. The effect of each variable on the model
was assessed, and the variable was kept if it significantly contributed
to a better fit of the model. The final model included the following
variables: RhV and CVEV. The results of the multivariate model showed
that CVEV was independently associated with rhinorrhea (OR: 4.73; CI:
1.59 – 14.07). CVEV infected patients were 4.73 times more likely to
have rhinorrhea compared to none-CVEV patients controlling for RhV.
Unlike the bivariate analysis, RhV was not significantly associated
with rhinorrhea (OR: 1.78; CI: 0.91 – 3.48). RhV infected patients were
1.78 times more likely to have rhinorrhea compared to none-RhV patients
controlling for CVEV; however, this was not statistically significant.
Discussion
We
demonstrated that viral infections are responsible for at least half of
the ARIs in children in Lebanon. Rhinovirus infection was the most
common etiology of ARI consistent with other studies from Lebanon and
other countries.[18-21] In neighboring Jordan and Egypt rhinovirus
incidence was second to RSV, but the population captured in these
studies was younger than that included in our study.[21,22] The overall
viral ARI incidence (52.5%) in our study lower than that recently
reported by Finianos et al. (70%) in Lebanon.[18] Both studies targeted
children; however, Finianos et al. screened their specimens for more
viral targets than those included in our analysis. In our study we did
not test for HCoV, AdV, EV, and HBoV which collectively accounted for
50% of viral ARI in the study by Finianos et al.
The coinfection
rate in our study (42.9%) was higher than that previously reported in
Lebanon (37%), Qatar (21.4%), and Egypt (10.8%).[18,22,23] This
incongruence could be because CVEV, which was frequently detected with
other viruses in our study, was not screened in the previous studies
from the region.[18] CVEV infections are not commonly reported in
studies investigating respiratory infections. In our study, CVEV
infection constituted 38.8% of all viral ARI cases and was
independently associated with rhinorrhea. This incidence is much higher
than that reported in other countries. A recent study in Latin America
reported that CVEV was associated with 3% of the ARI cases.[24] In
Central America, CVEV was even much lower (0.3%).[25] The very low
prevalence of CVEV in other regions might have discouraged its testing.
Given the high prevalence of CVEV in Lebanon, we recommend testing for
enteroviruses, including (CVEV).
Co-infections were found to be
more common younger children in Lebanon, and that is similar to a
previous study done in Mexican children showing that the majority of
coinfections occur in children <6 months of age.[26] Younger
children are likely to be more prone to infections due to their lack or
still weak immunity to respiratory viruses. The effect of coinfections
on disease outcomes is not well understood.[27] Patients coinfected
with pandemic H1N1 influenza and rhinovirus tended to have milder
clinical severity when compared with non-rhinovirus coinfections;[28]
while the patients coinfected with HMPV and RSV were prone to a higher
risk of severe bronchiolitis.[29] Additionally, the prevalence and
severity of obstructive airway disease were higher in patients with
coinfections.[30] In our study, coinfection was associated with higher
risk of rhinorrhea but not with more severe symptoms like dyspnea. In
contrast, some studies showed no correlation between coinfection status
and clinical severity.[31,32]
The complexity of viral coinfections
and the large number of respiratory viruses involved make challenging
to study the effect of coinfection on disease outcome in a clinical
setting. Therefore, there is a need for developing in vitro or in vivo
models to allow a better understanding of coinfections. For example,
dual infection with INF was shown to suppress RSV growth in vitro.[33]
The suppression of RSV by INF was suggested to be due to competition
for protein synthesis and budding from the cell surface. Further
studies are warranted to investigate the interactions among respiratory
viruses during coinfection and their effect on the host.
Our study
had a couple of limitations. First, we have not screened for HBoV, and
HCoV which are not included in ResPlex II kit and thus the prevalence
of viral ARI is expected to be higher than 52%. Another limitation was
our inability to rule out bacterial etiologies which were not tested
for in the current study. In conclusion, viral etiologies contribute to
a large proportion of ARIs many of which involve more than one viral
agent.
References
- Bellos A, Mulholland K, O'Brien KL, Qazi SA, Gayer
M, Checchi F. The burden of acute respiratory infections in
crisis-affected populations: a systematic review. Confl Health.
2010;4:3. https://doi.org/10.1186/1752-1505-4-3 PMid:20181220 PMCid:PMC2829474
- WHO | The global burden of disease: 2004 update [Internet]. WHO. [cited 2016 May 11]. Available from: http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/
- Williams
BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide
distribution of child deaths from acute respiratory infections. Lancet
Infect Dis. 2002 Jan;2(1):25-32. https://doi.org/10.1016/S1473-3099(01)00170-0
- Nichols
WG, Campbell AJP, Boeckh M. Respiratory Viruses Other than Influenza
Virus: Impact and Therapeutic Advances. Clin Microbiol Rev. 2008 Apr
1;21(2):274-90. https://doi.org/10.1128/CMR.00045-07 PMid:18400797 PMCid:PMC2292575
- Mahony JB. Detection of Respiratory Viruses by Molecular Methods. Clin Microbiol Rev. 2008 Oct 1;21(4):716-47. https://doi.org/10.1128/CMR.00037-07 PMid:18854489 PMCid:PMC2570148
- Goldmann
DA. Epidemiology and prevention of pediatric viral respiratory
infections in health-care institutions. Emerg Infect Dis.
2001;7(2):249-53. https://doi.org/10.3201/eid0702.010220 PMid:11294717 PMCid:PMC2631706
- Berry
M, Gamieldien J, Fielding BC. Identification of New Respiratory Viruses
in the New Millennium. Viruses. 2015 Mar 6;7(3):996-1019. https://doi.org/10.3390/v7030996 PMid:25757061 PMCid:PMC4379558
- Nair
H, Brooks WA, Katz M, Roca A, Berkley JA, Madhi SA, et al. Global
burden of respiratory infections due to seasonal influenza in young
children: a systematic review and meta-analysis. Lancet Lond Engl. 2011
Dec 3;378(9807):1917-30. https://doi.org/10.1016/S0140-6736(11)61051-9
- Nair
H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, et al.
Global burden of acute lower respiratory infections due to respiratory
syncytial virus in young children: a systematic review and
meta-analysis. The Lancet. 2010 May 7;375(9725):1545-55. https://doi.org/10.1016/S0140-6736(10)60206-1
- Fendrick
AM, Monto AS, Nightengale B, Sarnes M. The economic burden of
non-influenza-related viral respiratory tract infection in the United
States. Arch Intern Med. 2003 Feb 24;163(4):487-94. https://doi.org/10.1001/archinte.163.4.487 PMid:12588210
- Bawage
SS, Tiwari PM, Pillai S, Dennis V, Singh SR. Recent Advances in
Diagnosis, Prevention, and Treatment of Human Respiratory Syncytial
Virus. Adv Virol [Internet]. [cited 2016 May 11];2013. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3872095/
- Hayden
F. Developing New Antiviral Agents for Influenza Treatment: What Does
the Future Hold? Clin Infect Dis. 2009 Jan 1;48(Supplement 1):S3-13. https://doi.org/10.1086/591851 PMid:19067613
- Hayden
FG. Advances in antivirals for non-influenza respiratory virus
infections. Influenza Other Respir Viruses. 2013 Nov 1;7:36-43. https://doi.org/10.1111/irv.12173 PMid:24215380 PMCid:PMC6492651
- Gill
JM, Fleischut P, Haas S, Pellini B, Crawford A, Nash DB. Use of
antibiotics for adult upper respiratory infections in outpatient
settings: A national ambulatory network study. Fam Med. 2006
May;38(5):349-54.
- Gonzales
R, Malone DC, Maselli JH, Sande MA. Excessive Antibiotic Use for Acute
Respiratory Infections in the United States. Clin Infect Dis. 2001 Sep
15;33(6):757-62. https://doi.org/10.1086/322627 PMid:11512079
- Pavia
AT. Viral Infections of the Lower Respiratory Tract: Old Viruses, New
Viruses, and the Role of Diagnosis. Clin Infect Dis. 2011 May
1;52(suppl 4):S284-9. https://doi.org/10.1093/cid/cir043 PMid:21460286 PMCid:PMC3106235
- Li
H, McCormac MA, Estes RW, Sefers SE, Dare RK, Chappell JD, et al.
Simultaneous detection and high-throughput identification of a panel of
RNA viruses causing respiratory tract infections. J Clin Microbiol.
2007 Jul;45(7):2105-9. https://doi.org/10.1128/JCM.00210-07
PMid:17507510 PMCid:PMC1932978
- Finianos
M, Issa R, Curran MD, Afif C, Rajab M, Irani J, et al. Etiology,
seasonality and clinical characterization of viral respiratory
infections among hospitalized children in Beirut, Lebanon. J Med Virol.
2016 Apr 1;n/a-n/a. https://doi.org/10.1002/jmv.24544 PMid:27061822
- Wertheim
HFL, Nadjm B, Thomas S, Agustiningsih A, Malik S, Diep NNT, et al.
Viral and atypical bacterial aetiologies of infection in hospitalised
patients admitted with clinical suspicion of influenza in Thailand,
Vietnam and Indonesia. Influenza Other Respir Viruses. 2015 May 16; https://doi.org/10.1111/irv.12326 PMid:25980749 PMCid:PMC4605413
- Regamey
N, Kaiser L, Roiha HL, Deffernez C, Kuehni CE, Latzin P, et al. Viral
Aetiology of Acute Respiratory Infections With Cough in Infancy: A
Community-Based Birth Cohort Study. Pediatr Infect Dis J [Internet].
2008 Jan [cited 2015 Jul 20];PAP. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00006454-900000000-99976 https://doi.org/10.1097/INF.0b013e31815922c8 PMid:18174876
- Ali
SA, Williams JV, Chen Q, Faori S, Shehabi A, Jundi EA, et al. Human
metapneumovirus in hospitalized children in Amman, Jordan. J Med Virol.
2010 May 1;82(6):1012-6. https://doi.org/10.1002/jmv.21768 PMid:20419816 PMCid:PMC3347978
- Shafik
CF, Mohareb EW, Yassin AS, Amin MA, El Kholy A, El-Karaksy H, et al.
Viral etiologies of lower respiratory tract infections among Egyptian
children under five years of age. BMC Infect Dis. 2012;12:350. https://doi.org/10.1186/1471-2334-12-350 PMid:23237512 PMCid:PMC3538156
- Al-Thani
A, Azzam SB, Al-Sheik Abboubaker HM, Abdel-Hadi FG, Elsheikh M, Janahi
IA. The role of human metapneumovirus in pediatric respiratory tract
infection in Qatar. Future Virol. 2010 May;5(3):355-60. https://doi.org/10.2217/fvl.10.13
- Garcia
J, Espejo V, Nelson M, Sovero M, Villaran MV, Gomez J, et al. Human
rhinoviruses and enteroviruses in influenza-like illness in Latin
America. Virol J. 2013;10:305. https://doi.org/10.1186/1743-422X-10-305 PMid:24119298 PMCid:PMC3854537
- Laguna-Torres
VA, Sánchez-Largaespada JF, Lorenzana I, Forshey B, Aguilar P, Jimenez
M, et al. Influenza and other respiratory viruses in three Central
American countries. Influenza Other Respir Viruses. 2011 Mar
1;5(2):123-34. https://doi.org/10.1111/j.1750-2659.2010.00182.x PMid:21306576 PMCid:PMC4942008
- Diaz
J, Morales-Romero J, Pérez-Gil G, Bedolla-Barajas M, Delgado-Figueroa
N, García-Román R, et al. Viral coinfection in acute respiratory
infection in Mexican children treated by the emergency service: A
cross-sectional study. Ital J Pediatr. 2015 Apr 18;41(1):33. https://doi.org/10.1186/s13052-015-0133-7 PMid:25903455 PMCid:PMC4405868
- Tregoning
JS, Schwarze J. Respiratory Viral Infections in Infants: Causes,
Clinical Symptoms, Virology, and Immunology. Clin Microbiol Rev. 2010
Jan 1;23(1):74-98. https://doi.org/10.1128/CMR.00032-09 PMid:20065326 PMCid:PMC2806659
- Esper
FP, Spahlinger T, Zhou L. RATE AND INFLUENCE OF RESPIRATORY VIRUS
CO-INFECTION ON PANDEMIC (H1N1) INFLUENZA DISEASE. J Infect. 2011
Oct;63(4):260-6. https://doi.org/10.1016/j.jinf.2011.04.004 PMid:21546090 PMCid:PMC3153592
- Semple
MG, Cowell A, Dove W, Greensill J, McNamara PS, Halfhide C, et al. Dual
Infection of Infants by Human Metapneumovirus and Human Respiratory
Syncytial Virus Is Strongly Associated with Severe Bronchiolitis. J
Infect Dis. 2005 Feb 1;191(3):382-6. https://doi.org/10.1086/426457 PMid:15633097
- Aberle
JH, Aberle SW, Pracher E, Hutter H-P, Kundi M, Popow-Kraupp T. Single
versus dual respiratory virus infections in hospitalized infants:
impact on clinical course of disease and interferon-gamma response.
Pediatr Infect Dis J. 2005 Jul;24(7):605-10. https://doi.org/10.1097/01.inf.0000168741.59747.2d PMid:15999001
- Wilkesmann
A, Schildgen O, Eis-Hübinger AM, Geikowski T, Glatzel T, Lentze MJ, et
al. Human metapneumovirus infections cause similar symptoms and
clinical severity as respiratory syncytial virus infections. Eur J
Pediatr. 2006 Jul;165(7):467-75. https://doi.org/10.1007/s00431-006-0105-4 PMid:16607540
- Bezerra
PGM, Britto MCA, Correia JB, Duarte M do CMB, Fonceca AM, Rose K, et
al. Viral and atypical bacterial detection in acute respiratory
infection in children under five years. PloS One. 2011;6(4):e18928. https://doi.org/10.1371/journal.pone.0018928 PMid:21533115 PMCid:PMC3078930
- Shinjoh
M, Omoe K, Saito N, Matsuo N, Nerome K. In vitro growth profiles of
respiratory syncytial virus in the presence of influenza virus. Acta
Virol. 2000 Apr;44(2):91-7.