Marco Cioce1, Franziska Michaela Lohmeyer2, Rossana Moroni2, Marinella Magini3, Alessandra Giraldi3, Paola Garau1, Maria Carola Gifuni1, Vezio Savoia4, Danilo Celli5, Stefano Botti6, Gianpaolo Gargiulo7, Francesca Bonifazi8, Fabio Ciceri9, Ivana Serra10, Maurizio Zega10, Simona Sica11, Andrea Bacigalupo11, Valerio De Stefano11 and Umberto Moscato12..
1 UOC
Ematologia e Trapianto di Cellule Staminali Emopoietiche, Fondazione
Policlinico Universitario Agostino Gemelli IRCCS, Roma, Italy.
2 Direzione scientifica, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Roma, Italy.
3 UOC Nutrizione clinica, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Roma, Italy.
4 Servizio di Psico-Oncologia, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Roma, Italy.
5 Facoltà di Medicina e Psicologia, Università “La Sapienza”, Roma, Italy.
6 UOC Ematologia, Azienda USL-IRCCS di Reggio Emilia, Italy.
7 UOC Ematologia, Università “Federico II”, Napoli, Italy.
8 Istituto di Ematologia “Seràgnoli”, Policlinico Universitario S.Orsola-Malpighi, Bologna, Italy.
9 IRCCS Ospedale San Raffaele, Milano, Italy.
10 Direzione SITRA, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Roma, Italy.
11 Istituto di Ematologia, Università Cattolica del Sacro Cuore, Roma, Italy.
12 Istituto di Sanità pubblica, Università Cattolica del Sacro Cuore, Roma, Italy.
Correspondence to: Marco Cioce, UOC Ematologia e Trapianto di
Cellule Staminali Emopoietiche, Fondazione Policlinico Universitario
Agostino Gemelli IRCCS, Largo Agostino Gemelli, 8 00168 Roma, Italy.
Tel.: +393472294176. E-mail:
marco.cioce@policlinicogemelli.it;
Published: September 1, 2020
Received: June 19, 2020
Accepted: August 16, 2020
Mediterr J Hematol Infect Dis 2020, 12(1): e2020067 DOI
10.4084/MJHID.2020.067
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background.
Physical and psychological factors, like wrong attitudes and
behaviours, can negatively influence the health outcomes of the
patients receiving allogeneic hematopoietic stem cell transplantation
(AHSCT). Educational interventions aiming to improve knowledge on side
effects, risks, complications and preventive behaviour can reduce
psychological distress, and improve quality of life (QoL). We aimed to
compare a standard approach with therapeutic patient education (TPE) to
analyse the impact on AHSCT patients' QoL, psychological distress and
knowledge of AHSCT side effects, risks complications and preventive
behaviour.
Material and methods.
A prospective interventional study was conducted analysing data of 36
patients who received one of two different educational approaches,
which were a standard approach (not-exposed) or TPE (exposed).
Results.
In the exposed group QoL improved 14 days after transplantation (42.2
vs 25.6; p<0.03) and at time of discharge (36.6 vs 54.4;
p<0.005). Anxiety and depression were better controlled in the
exposed group, both at hospitalisation and discharge (anxiety: 48.1 vs
53.2; 46.4 vs 51.6. p<0.04; depression: 49 vs 55.3; 48 vs 54.3,
p<0.03). Knowledge of AHSCT risks and complications improved in
exposed patients, both at admission (10.1/15 vs 8/15 correct answers;
p<0.01) and discharge (10.7/15 vs 8.8/15 correct answer; p<0.03).
Conclusions.
The TPE for AHSCT patients improved knowledge, reduced anxiety and
depression, which consequently increasing QoL. Therefore, we recommend
our approach to further engage patients in the treatment plan, which
should specifically take place prior to AHSCT initiation.
|
Introduction
Allogeneic hematopoietic stem cell transplantation (AHSCT) is the standard of care for several haematological disorders.[1]
AHSCT patients require hospitalisation in protected environments where
they follow appropriate antimicrobial prophylaxis and prevention
programs to overcome the toxic effects of the therapy minimising
associated risks. However, non-relapse mortality at two years ranges
between 15% and 40%, and it depends on the patients' age,
comorbidities, disease, status at transplant, conditioning regimen and
donor type.[2] Survival at two years ranges between 50% and 80%.[3]
AHSCT
is associated with health problems occurring in the immediate
post-transplant period including infections, bleeding, mucositis,
fever, nausea, hypotension and shock, skin rash, acute or chronic pain
and diarrhea[4] which can negatively affect patients' QoL and survival.[5]
In
addition, patients undergoing an AHSCT can present relevant
psychological distress - most common depression, anxiety and sleeping
problems - they might confront with primitive defence mechanisms such
as denial, and projection.[6] Depression is the most common manifestation of psychological distress in patients with neoplastic disease;[7-9] which is even more frequent in patients with advanced disease.[10-12]
AHSCT
requires that patients and their families change their daily life.
Patients and their caregivers can reinforce their knowledge on
necessary lifestyle changes following specific therapeutic, educational
interventions, increasing patient engagement, collaboration with
healthcare-worker, knowledge of the disease and treatment, and QoL,
which can positively impact their health outcomes.[13,14]
The
use of audio-video and information material for individual learning
accompanied by verbal instructions, complemented by multidisciplinary
and interactive educational teaching tools notably improved knowledge
and practical skills.[15] Currently, no studies exist
in the literature, which systematically assessed the relationship
between therapeutic education and health outcomes in AHSCT.
This
study aimed to compare a standard with therapeutic patient education
(TPE) analysing the impact on QoL, psychological distress and knowledge
of AHSCT side effects, risk factors, complications as well as
preventive behaviour.
Materials and Methods
Study design. This is an interventional, randomised (computer-generated, 1:1), double-blind study with two groups:
• Not-exposed
group. Standard approach, printed informative material about the
transplant procedure, complications, self-care, general advice, diet
and safety issues, was delivered at the time of hospitalisation by the
primary nurse;
• Exposed group. TPE conducted by a nurse, a dietician and a psychologist.
Patients have been randomised in the two groups immediately after singing written informed consent.
The study was approved by the local ethics committee on January 18, 2018 (Prot. 46787/17 – 1143/18, ID: 1767).
Inclusion/exclusion.
Thirty-six patients undergoing AHSCT at our hospital (central Italy)
were involved in the study from May to December 2018, of them the half
came from other centres of Italy. All participants were adults (over 18
years) of both sexes and able to provide written informed consent.
Exclusion criteria were the following: patient uncooperative and/or
affected by mental disease, pregnant or breastfeeding women.
Sample size calculation.
The sample size was calculated considering a mixed model ANOVA with
repeated measures, with alpha=0.01 and power 80%, delta=0.6325 on two
groups; and variance between groups=0.0200 and a variance
"between-within groups" =0.05 for two or more repeated measures with a
correlation index rho=0.9. Considering a possible drop-out, we
recruited 36 patients (18 patients in each group).
Therapeutic patient education. The TPE, based on a WHO working group report,[16]
taking place about a week before transplant hospitalisation, including
an interview of about 60 minutes in which the patient and the caregiver
participated and verbal instructions were provided on the following
areas:
• Nursing care. During the meeting, nurses
addressed detailed AHSCT side effects, risks, complications and
preventive behaviour responding on arising questions; a video of about
10 minutes was projected explaining main complications, hand hygiene,
protective isolation and lower microbial load rooms (video
surveillance, health call etc.). Additionally, printed informative
material (mucositis, hand hygiene, access mode, recommendations and
prohibitions, multi-resistant germ brochures as well as an allogeneic
transplant guide) was handed out and explained.
• Psychological.
Most frequent psychological problems (anxiety and depression) in the
onco-haematological area and possible interventions were addressed; a
psycho-oncologist with several years of experience answered raised
questions.
• Nutritional. Educational intervention
according to guidelines of the International Agency for Research on
Cancer (IARC) and the European Society for Clinical Nutrition and
Metabolism (ESPEN) for cancer patients. Data collected in the
nutritional education area evaluating caloric-proteic malnutrition in
patients undergoing AHSCT is not part of this publication.
Outcome measures.
The 36 patients observed were evaluated for QoL with the Cancer Linear
Analogue Scale (CLAS) at time of admission (T0), day of the AHSCT (T1),
7 and 14 days after the AHSCT (T2/T3) as well as at discharge (T4).
CLAS investigates energy level, ability to perform daily activities and
overall QoL.
The Symptom Checklist-90-R (SCL-90-R) was performed
at T0 and T4, assessing symptom severity of psychological distress in
the week before checklist performance. The patient's responses are
interpreted based on nine primary symptomatological dimensions
(cut-off≥55).
The degree of knowledge regarding concepts addressed
during the TPE was assessed through a structured multiple-choice
questionnaire at T0 and T4, which was composed of 15 items, 5 for each
profession involved. The reliability of the internal consistency has
been tested through the alpha Cronbach and the validity of the content
through the Content Validity Index.[17] The internal consistency of the instrument used, measured by calculating the alpha of Cronbach, was 0.83.
Statistical analysis.
The sample was described in its socio-demographic and clinical
characteristics through descriptive statistic techniques. Qualitative
variables have been described using absolute frequencies and
percentages, while quantitative variables have been summarised through
the range, mean, median and standard deviation. Normality of data was
verified with the Shapiro-Wilk test. Comparisons were performed with
t-tests for paired data or Kruskal-Wallis, for nonparametric variables.
Mixed model ANOVA and generalised linear model, where the
between-subjects factor was represented by two groups (exposed and
not-exposed) and the within-subjects factor is represented by the
time was used for repeated measurements.[18]
Bonferroni correction was applied. Data have been stored and managed in
spreadsheet (Data set created on a Microsoft Excel 2016 spreadsheet for
Mac Vers. 2016/14.5.5). Statistical analyses were carried out with
Stata7IC software[ 14.2 for Mac (64-bit Intel), Vers. January 09 2017,
800-STATAPC- Lakeway]. Statistical significance was set at p<0.05.
Results
Of
36 patients included in the study, 18 have been randomised to the
not-exposed group (50.0%), with 40% (7/18) coming from other centres,
and 18 have been randomised to the exposed group (50.0%), with 60%
(11/18) from other centres. The proportion of missing data at the end
of the study was minimal (<5%). The sample consisted mainly of male
patients (n=22, 61.1%), most of them in the not-exposed group (83.3% of
males in the group) while 61.1% of patients in the exposed group were
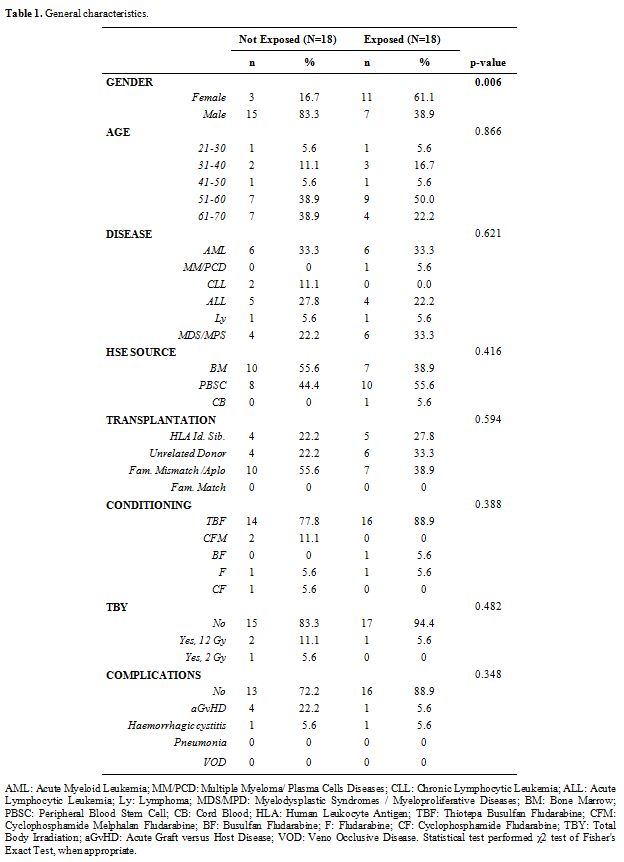
females, p=0.006. Table 1 describes the clinical and demographic characteristics of the cohort.
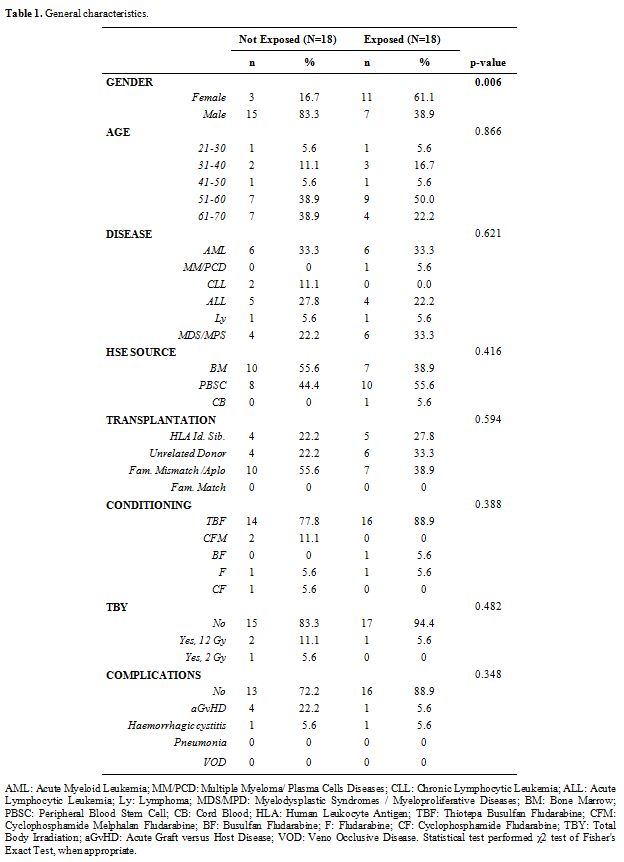 |
Table 1. General characteristics. |
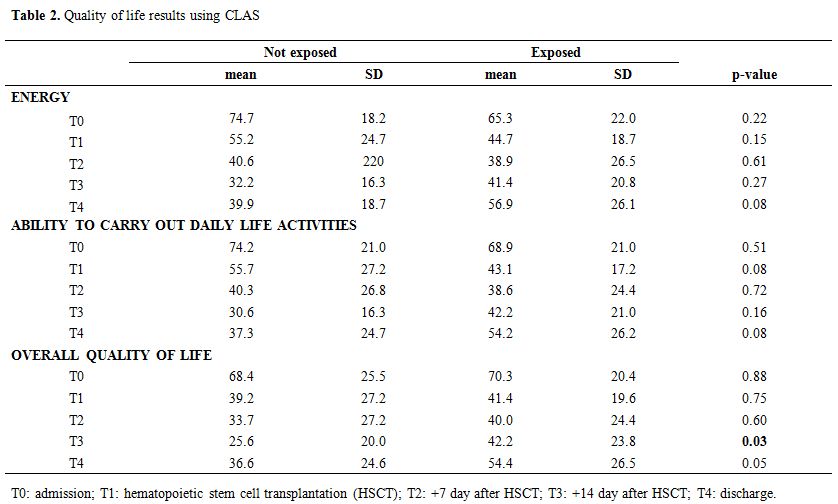
Table 2
demonstrates the results regarding QoL assessed with CLAS. The exposed
group had statistically significant (p=0.03) better scores 42.2 versus
25.6 (not-exposed group) at T3 (14 days after AHSCT) when questioned
about their general QoL. The difference between the two groups was more
significant at discharge: 36.6 (exposed) and 54.4 (not exposed),
p=0.05.
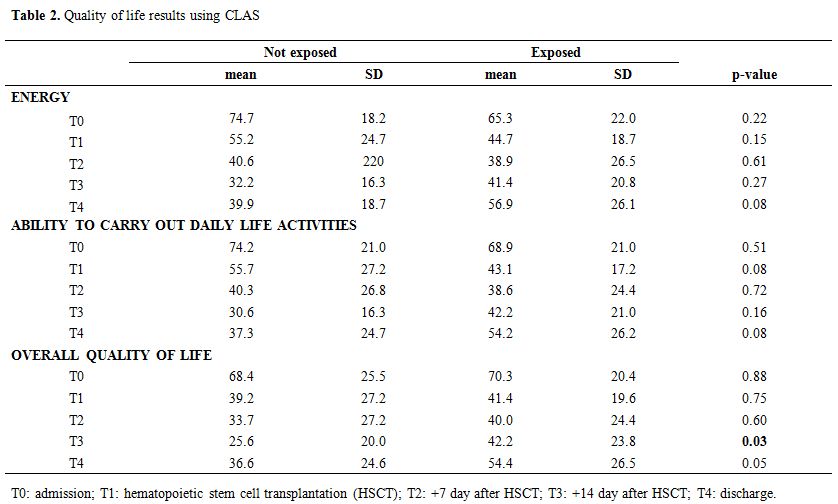 |
Table
2. Quality of life results using CLAS |
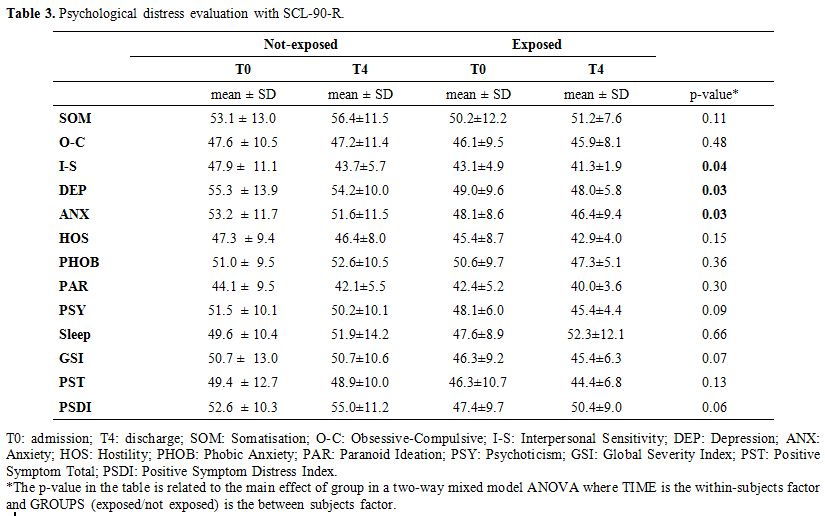
Regarding
psychological distress assessed with SCL-90-R, statistically
significant results have been highlighted in the area of interpersonal
hypersensitivity (I-S) where the main effect of group's p-value was
0.04. More detailed, in the not-exposed group, the mean discomfort
related to T0 was 47.9 (±11.1) and was 43.7 (±5.7) in T4. In the
exposed group, the mean discomfort was 43.1 (±4.9) and was 41.3 (±1.9)
in T4. For the areas anxiety (ANX) and depression (DEP), all patients,
exposed and not-exposed had symptoms at T0 and T4, whose intensity did
not deviate from the average values found in the reference sample. The
anxiety score (ANX) decreased from 53.2 to 51.6 in not-exposed patients
and from 48.1 to 46.4 in exposed patients (groups main effect p=0.03).
The DEP score increased from 55.3 to 54.2 in not-exposed patients and
decreased from 49 to 48 in exposed patients (groups main effect
p=0.03). Although the p-value was not significant, it is important to
underline that, in the area of paranoid ideation (PAR), no elements of
discomfort are highlighted at both T0 and T4; the score decreased from
44.1 to 42.1 in not-exposed patients and from 42.4 to 40 in exposed
patients (Table 3).
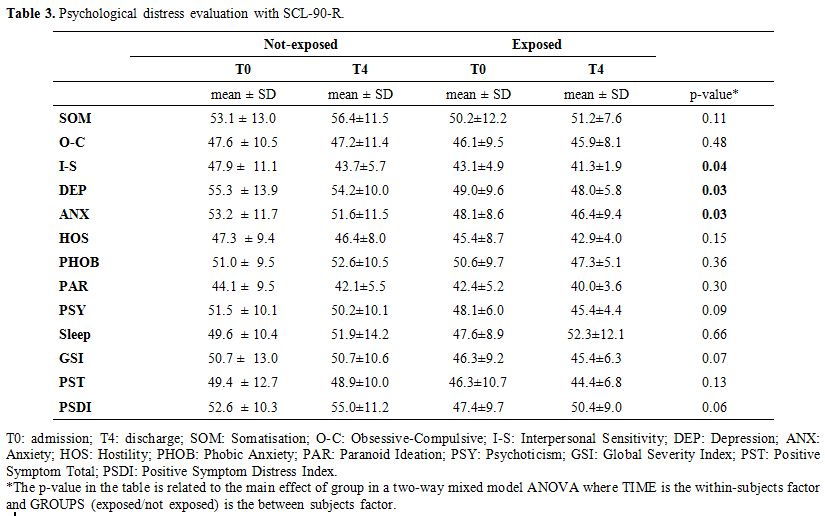 |
Table 3. Psychological distress evaluation with SCL-90-R.. |
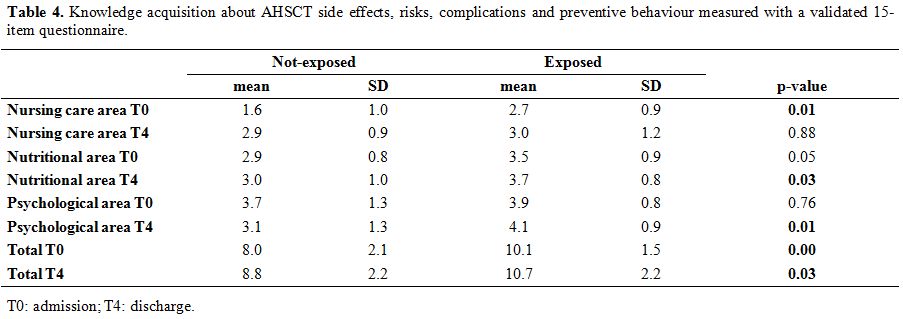
Table 4
shows the results of the 15-item questionnaire about knowledge
acquisition in the three areas (nursing care, psychological and
nutritional). Both total scores at T0 and T4 were statistically
significant, demonstrating increased awareness in the exposed group
compared with the not-exposed group. More detailed, the correct answers
given, at T0 in the exposed group were 10.1/15 compared with 8/15 in
the not-exposed group (p<0.0); instead, at T4, results were 10.7/15
in the exposed group compared with 8.8/15 in the not-exposed group
(p<0.03).
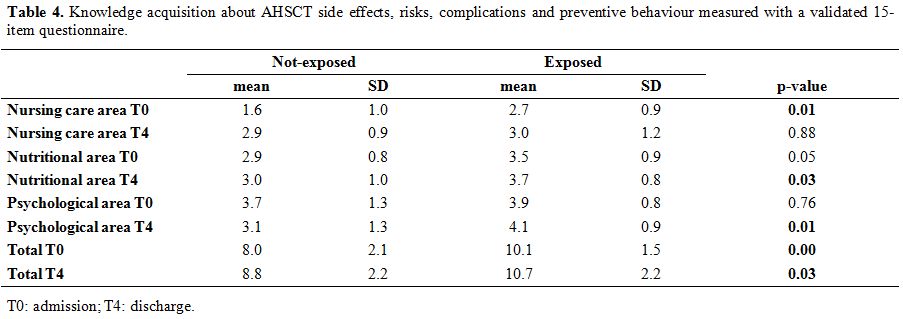 |
Table 4. Knowledge
acquisition about AHSCT side effects, risks, complications and
preventive behaviour measured with a validated 15-item
questionnaire. |
Discussion
Our
data demonstrate that the TPE, taking place about a week before
transplant hospitalisation, statistically significant improved
patients' knowledge of AHSCT side effects, risks, complications as well
as preventive behaviour. Further, we demonstrated that knowledge gain
reduced psychological distress, improving QoL in our cohort.
More
detailed, we noted statistically significantly increased knowledge in
the total scores of the exposed group compared with the not-exposed
group, both at T0 (p=0.0) and T4 (p=0.3). We based the development of
our TPE on findings by Friedman et al. (2011)[19] who
reinforced the thesis that teaching strategies using audio-video
presentations, verbal instructions and personalised information
material, assuring an appropriate level for independent study, are more
effective than traditional methods to improving knowledge and behaviour
of patients. Bennet et al. (2016)[20] evaluated
educational strategies in adult cancer patients, in a systematic review
of 14 randomised clinical trials, which showed that the integration of
different educational modalities is effective to reduce fatigue and
anxiety improving overall QoL.
Furthermore, we noted that the
nursing care score at T0 was statistically significant (p=0.01) whereas
at T4 not (p=0.88); this might be explainable with the intense training
and information the exposed group received during the TPE by nurses. To
improve our approach further, we suggest repeating parts of the
teaching during hospital admission to ensure that preventive behaviour
and attitudes will be remembered.
Likewise, we noticed that
psychological distress was significantly improved at T4 (p=0.01), but
not at T0 (p=0.76). This result can be explained that the intervention
of different health workers, during the TPE, reduces uncertainties of
the transplantation path, which positively impacts the patient's
psychological state.
Our conclusions can be further confirmed with
data on psychological distress assessed with SCL-90-R. We showed
significant differences between the two groups in the areas ANX and
DEP. Patients of the exposed group, compared to the not-exposed group,
showed that they went through the therapeutic journey with a lower
level of fear, worry and demoralisation. The TPE allows the patient an
adequate containment of potential distress such as fear, worrying and
sadness, making the state of anxiety and depression not requiring
specialist psychotherapeutic and psychiatric interventions. This result
has been obtained through description, explication and instruction of
the possible risks associated with admission to a lower microbial load
room and possible side effects of AHSCT treatment. These data are in
accordance with the results by Fawzy et al. (1993)[21]
who demonstrated that the intervention of a 6-week psychotherapeutic
group - including educational interventions as psychological support,
stress management and development of coping skill - was associated
with lower mortality in patients with malignant melanoma after six
years follow-up. Donker et al. (2019)[22] evidenced
that psychological education (information, teaching material and
advice) reduced levels of psychological distress and specifically
depression.
Related to reduced psychological distress, before
and during AHSCT, is the improvement of QoL. Data collected show that
the TPE for patients and their caregivers reduced psychological
distress and improved statistically significant QoL (p=0.03) at T3
assessed with CLAS. Several studies confirm that educational
interventions improve knowledge of AHSCT and QoL in the long term.[23] Kirsch et al. (2012)[24]
demonstrated the effectiveness of educational/therapeutic
interventions, which acted synergistically, on the strengthening of
problem-solving during treatment and follow-up. Instead, Marques et al.
(2012)[25] showed that QoL, measured with QLQ-C30,
has lower average scores in the pancytopenia compared to the
pre-transplant phase. This is probably due to the critical moments of
treatment when complications can occur, endangering patients’ lives or
interfering negatively with their QoL. Accordingly, we recorded lower
average values, which were even lower in the exposed group, both at T3
and T4. After hospitalisation, a progressive improvement to perform
daily activities and QoL, equal if not better than in the
pre-transplant phase, is usually expected between 9 to 12 months, even
if a percentage of patients suffering from late complications, such as
chronic Graft-versus-Host Disease (GvHD), reach the pre-transplant
level.[26]
Limitations
Among
our limitations is the relatively small, but notwithstanding adequate
sample size. According to our protocol, patients were randomly assigned
and which led to more women in the exposed group. Furthermore, data is
not generalisable to other contexts. Therefore, our study necessitates
confirmation on a larger cohort and replication in different settings
always in the context of AHSCT.
We do not know if the point in
time providing the two different approaches might have influenced our
results; exposed patients had one-week time in their familiar
surroundings to process the received information after they
participated on the TPE compared with the not-exposed group, which
received printed material at the time of hospitalisation. This aspect
was not investigated in our study.
Conclusions
In
conclusion, therapeutic education is a relevant aspect of clinical
pathways. Although several studies describe its usefulness in some
areas, evidence to support its effectiveness in AHSCT is lacking.
Obtaining information through educational interventions is a
fundamental right for patients undergoing AHSCT. We hope this approach
will spread widely as an educational methodology structured in a
multidisciplinary development perspective of real patient care and its
centrality in the care processes. The results of this study show that a
TPE before AHSCT improved knowledge on AHSCT side effects, risks,
complications and preventive behaviour, which reduced in our cohort
anxiety and depression positively affecting QoL. Based on our data, we
recommend engaging patients in AHSCT treatment as much and as early as
possible, allowing an active role in decision-making processes, which
improves adequate self-care. Furthermore, we believe that it might be
positive if the AHSCT topics addressed before hospitalisation are
repeated during admission, based on individual needs and capacities.
The
effectiveness of TPE in AHSCT should be confirmed in future multicentre
study in the GITMO group (Gruppo Italiano per il Trapianto di Midollo
Osseo, cellule staminali emopoietiche e terapia cellulare).
References
- Tura S. Corso di malattie del sangue e degli organi emolinfopoietici. 6 Ed., Bologna, Società Editrice Esculapio. 2015;377-387. https://doi.org/10.15651/978-88-748-8884-9
- Tanaka
Y, Kurosawa S, Tajima K, Tanaka T, Ito R, Inoue Y, Okinaka K, Inamoto
Y, Fuji S, Kim SW, Tanosaki R, Yamashita T, Fukuda T. Analysis of
non-relapse mortality and causes of death over 15 years following
allogeneic hematopoietic stem cell transplantation. Bone Marrow
Transplantation. 2016;51:553-559. https://doi.org/10.1038/bmt.2015.330 PMid:26752142
- Mosesso
K. Adverse Late and Long- Term Treatment Effects in Adult Allogeneic
Hematopoietic Stem Cell Transplant Survivors. American Jurnal of
Nursing. 2015;115(11):22-34. https://doi.org/10.1097/01.NAJ.0000473311.79453.64 PMid:26473441
- Cioce
M, Moroni R, Gifuni MC, Botti S, Orlando L, Soave S, Serra I, Zega M,
Gargiulo G. Relevance of NANDA-I diagnoses in patients undergoing
haematopoietic stem cell transplantation: a Delphi study. Professioni
Infermieristiche. 2019;72(2):120-128.
- Kim
I, Koh Y, Shin D, Hong J, Jae Do H, Kwon SH, Sik Seo K. Importance of
Monitoring Physical Function for Quality of Life Assessments in
Hematopoietic Stem Cell Transplantation Patients: A Prospective Cohort
Study. In vivo;34:771-777. https://doi.org/10.21873/invivo.11837 PMid:32111783 PMCid:PMC7157879
- Holland JC. Psychological Care of Patients. Psycho-Oncology's Contribution. J Clin Oncol, 2003;21:253s-265s. https://doi.org/10.1200/JCO.2003.09.133 PMid:14645405
- Akechi
T, Nakano T, Okamura H, Ueda S, Akizuki N, Nakanishi T, Uchitomi Y.
Psychiatric disorders in cancer patients: Descriptive analysis of 1721
psychiatric referrals at two Japanese cancer center hospitals. Japanese
Journal of Clinical Oncology. 2001;31:188 - 194. https://doi.org/10.1093/jjco/hye039 PMid:11450992
- Kugaya
A, Akechi T, Okuyama T, Nakano T, Mikami I, Okamura H, Uchitomi Y.
Prevalence, predictive factors, and screening for psychologic distress
in patients with newly diagnosed head and neck cancer. Cancer.
2000;88:2817-2823. https://doi.org/10.1002/1097-0142(20000615)88:12<2817::AID-CNCR22>3.0.CO;2-N
- Okamura
H, Watanabe T, Narabayashi M, Katsumata N, Ando M, Adachi I, Uchitomi
Y. Psychological distress following fi rst recurrence of disease in
patientswith breast cancer: Prevalence and risk factors. Breast Cancer
Research and Treatment. 2000;61:131 - 137. https://doi.org/10.1023/A:1006483214678 PMid:10942100
- Bukberg J, Penman D, Holland JC. Depression in hospitalised cancer patients. Psychosomatic Medicine. 1984;46:199 - 212. https://doi.org/10.1097/00006842-198405000-00002 PMid:6739680
- Longobardi
Y, Savoia V, Bussu F, Morra L, Mari G, Nesci DA, Parrilla C, D'Alatri
L. Integrated rehabilitation after total laringectomy: a pilot trial
study. Support Care Cancer. 2019;27(9):3537-3544. https://doi.org/10.1007/s00520-019-4647-1 PMid:30685792
- Carlson
LE. Screening alone is not enough: The importance of appropriate
triage, referral, and evidence-based treatment of distress and common
problems. J Clin Oncol, 2013;31:3616-3617. https://doi.org/10.1200/JCO.2013.51.4315 PMid:24002494
- Assal JP, Golay A. Patient education in Switzerland: from diabetes to chronic diseases. Patient Educ Couns. 2001;44(1):65-9. https://doi.org/10.1016/S0738-3991(01)00105-7
- Bevans
M, Castro K, Prince P, Shelburne N, Prachenko O, Loscalzo M, Zabora J.
An Individualized Dyadic Problem-Solving Education Intervention for
Patients and Family Caregivers During Allogeneic HSCT: A Feasibility
Study. Cancer nursing. 2010;33(2):24-33. https://doi.org/10.1097/NCC.0b013e3181be5e6d PMid:20142739 PMCid:PMC2851241
- Foltz
A, Sullivan J. Reading level, learning presentation preference, and
desire for information among cancer patients. Journal of Cancer
Education. 1996;11:32-38.
- World Health
Organization. Europe Report Therapeutic Patient Education - Continuing
Education Programmes for Health Care Providers in the Field of Chronic
Disease. Copenhagen, Denmark: WHO; 1998. [Google Scholar]
- Fain AJ. La ricerca infermieristica: leggerla, comprenderla e applicarla. 2 Ed., Milano: McGraw-Hill. 2004;125.
- Moscato
U, Poscia A, Gargaruti R, Capelli G, Cavaliere F. Normal values of
exhaled carbon monoxide in healthy subjects: comparison between two
methods of assessment. BMC Pulm Med. 2014;16(14):204. https://doi.org/10.1186/1471-2466-14-204 PMid:25515007 PMCid:PMC4275957
- Friedman
AJ, Cosby R, Boyko S, Hatton-Bauer J, Turnbull G. Effective teaching
strategies and methods of delivery for patient education: a systematic
review and practice guideline recommendations. J Cancer Educ. 2011;
26(1):12-21. https://doi.org/10.1007/s13187-010-0183-x PMid:21161465
- Bennett
S, Pigott A, Beller EM, Haines T, Meredith P, Delaney C. Educational
interventions for the management of cancer-related fatigue in adults.
Cochrane Database of Systematic Reviews. 2016;11: Art. No.: CD008144. https://doi.org/10.1002/14651858.CD008144.pub2 PMCid:PMC6464148
- Fawzy
FI, Fawzy NW, Hyun CS, Elashoff R, Guthrie D, Fahey J, Morton DL.
Malignant melanoma: Effects of an early structural psychiatric
intervention, coping and affective state on recurrence and survival 6
years later. Archives of General Psychiatry. 1993;50:681-689. https://doi.org/10.1001/archpsyc.1993.01820210015002 PMid:8357293
- Donker
T, Griffiths KM, Cuijpers P, Christensen H. Psychoeducation for
depression, anxiety and psychological distress: a meta-analysis. BMC
Medicine. 2009;7:79. https://doi.org/10.1186/1741-7015-7-79 PMid:20015347 PMCid:PMC2805686
- Pidala
J, Anasetti C, Jim H. Health-related quality of life following
haematopoietic cell transplantation: patient education, evaluation and
intervention. British Journal of Haematology. 2009;148:373-385. https://doi.org/10.1111/j.1365-2141.2009.07992.x PMid:19919651 PMCid:PMC2810350
- Kirsch,
M., Crombez, P., Calza, S., Eeltink, C. & Johansson E. (2012).
Patient information in stem cell transplantation from the perspective
of health care professionals: A survey from the Nurses Group of the
European Group for Blood and Marrow Transplantation. Bone Marrow
Transplantation 47, 1131-1133. https://doi.org/10.1038/bmt.2011.223 PMid:22139070
- Marques
ADCB, Szczepanik AP, Machado CAM, Santos PND, Guimarães PRB, Kalinke
LP. Hematopoietic stem cell transplantation and quality of life during
the first year of treatment. Rev Lat Am Enfermagem. 2018; 25(26):e3065.
https://doi.org/10.1590/1518-8345.2474.3065 PMid:30379249 PMCid:PMC6206822
- Grulke
N, Albani C, BailerH. Quality of life in patients before and after
haematopoietic stem cell transplantation measured with the European
Organization for Research and Treatment of Cancer (EORTC) Quality of
Life Core Questionnaire QLQ-C30. Bone Marrow Transplantation.
2012;47:473-482. https://doi.org/10.1038/bmt.2011.107 PMid:21602898
[TOP]