Sarah Liptrott1,2,6, Mairéad NíChonghaile3,6, Liz O'Connell4,6 and Erik Aerts5,6.
1 Nursing
Development and Research Unit, Oncology Institute of Southern
Switzerland, Ente Ospedaliero Cantonale (EOC), via Gallino 12, 6500,
Bellinzona, Switzerland.
2 Department of Nursing,
Regional Hospital of Bellinzona e Valli, Ente Ospedaliero Cantonale
(EOC), via Gallino 12, 6500, Bellinzona, Switzerland.
3 HOPE Directorate, St James's Hospital, Dublin 8, Ireland.
4 Haematology Department, Tallaght University Hospital, Dublin 24, Ireland.
5 Department of Internal Medicine, Haematology, University Hospital Zurich, Rämistrasse 100, CH-8091 Zurich, Switzerland.
6 on behalf of the Haematology Nurses and Healthcare Professionals Group (HNHCP).
Correspondence to:
Sarah Liptrott, Nursing Development and Research Unit, Oncology
Institute of Southern Switzerland, Ente Ospedaliero Cantonale (EOC),
via Gallino 12, 6500, Bellinzona, Switzerland; Department of Nursing,
Regional Hospital of Bellinzona e Valli, Ente Ospedaliero Cantonale
(EOC), via Gallino 12, 6500, Bellinzona, Switzerland. Tel:+410918118957
Fax: +410918118056. Email:
sarahjayne.liptrott@eoc.ch
Published: May 1, 2023
Received: March 16, 2023
Accepted: April 20, 2023
Mediterr J Hematol Infect Dis 2023, 15(1): e2023033 DOI
10.4084/MJHID.2023.033
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
|
Abstract
Background and Objectives:The
scope of haematology nursing practice is dynamic and must respond to
advances in treatment, patients' needs and service requirements. Little
is known, however, about the different roles of haematology nurses
across the European setting. The purpose of this study was to identify
the professional practices of haematology nurses.
Method:
A cross-sectional online survey design was used to investigate practice
elements undertaken by haematology nurses. Frequencies and descriptive
statistics were calculated for demographic variables and chi-square
tests to examine relationships between practice elements, nursing role
and country.
Results:
Data is reported from 233 nurses across 19 countries, working as Staff
Nurses (52.4%), senior nurses (12.9%) and Advanced Practice Nurses
(APNs) (34.8%). Most frequently reported activities included medication
administration - oral/ intravenous (90.0%), monoclonal antibodies
(83.8%), chemotherapy (80.6%), and blood components (81.4%). APNs were
more commonly involved in nurse-led clinics and prescribing activities
(p < .001, p = .001, respectively); however, other nursing groups
also reported performing extended practice activities. Patient and
carer education was a significant part of all nurses' roles; however,
senior nurses and APNs were more often involved with the
multidisciplinary team (p < .001) and managerial responsibilities (p
< .001). Nurses' involvement in research was limited (36.3%) and
frequently reported as an out-of-work hours activity.
Conclusions:
This study describes haematology nursing care activities performed in
various contexts and within different nursing roles. It provides
further evidence of nursing activity and may contribute to a core
skills framework for haematology nurses.
|
Introduction
Across the WHO European region, there are an estimated 7.3 million nurses and midwives.[1] They are part of progressive healthcare systems responding to the needs of changing and ageing populations,[2] increasingly affected by chronic diseases.[3]
Nurses practice within a context of finite resources, where rising
healthcare costs necessitate effective and efficient service provision.[4]
The scope of nursing practice is dynamic and "describes the
competencies (knowledge, skills and judgement), professional
accountabilities and responsibilities of the nurse";[5]
however, 'nursing practice' is delineated by government legislation and
regulatory authorities, varying between countries, state and even
employing institution.[6,7] In the UK, nurses'
activities at the point of registration have broadened, including an
expected proficiency in ECG performance and interpretation and chest
auscultation.[8] Advanced practice roles have also developed in the USA initially in response to medical staff shortages.[9]
The need for improved access to care and enhanced nurse education has
facilitated their development in different settings and countries.[10]
Policy reforms in some countries have expanded nurses' clinical
practice to incorporate specialisations and activities such as
independent prescribing.[11,12]
While long-term
survival for patients affected by haematological malignancies is
increasing within the haematology setting, late morbidity and mortality
persist,[13] so survivors' healthcare needs to be
addressed. As well as improved survivorship, developments in cancer
nursing have seen several factors contributing to role changes,
including increasing use of immune-based therapies for haematological
malignancies[14] requiring new skills in nursing management, a shift in care delivery from the inpatient to outpatient setting,[15] and increasing numbers of nurse-led clinics.[16]
While literature exists investigating the practice of oncology nurses[17] and those working within advanced practice roles,[11] there is a paucity when exploring haematology nursing practice.
In 2010, Aerts et al.[18]
reported the results of a European survey of 271 nurses across 25
countries. Most common professional activities include patient
education regarding treatment and side effects, monitoring, and
administering supportive care treatment. Differences were also observed
between roles where Clinical Nurse Specialists (CNSs) were more
involved in patient and nurse education and multidisciplinary team
meetings compared to unit-based clinical nurses and Nurse Managers, and
where unit-based clinical nurses were more active in treatment
administration and side-effect management compared to CNSs.
Investigation of the specialist Haemophilia Nurse role in Europe, with
94 respondents from 14 countries, identified four main areas of
practice, treatment (preparation and administration), education and
support (telephone consultation), care coordination and research.[19] Curriculums and competencies for specialist and advanced nursing roles in haematology nursing are available;[20,21]
however, as highlighted earlier, practice application may differ
according to country and institution. Several legislation and nurse
education changes have been reported and implemented since the last
investigation of haematology nurses' practice performed in 2007.[18]
Such developments and the limited knowledge regarding the roles of
nurses working with patients affected by non-malignant haematological
conditions warrant further investigation to map current practice in the
European setting.
The purpose of this study was to identify the
professional practices of haematology nurses and examine whether
differences exist according to role and country of practice.
Methods
Design, Sample and Setting.
We used a cross-sectional survey design. All nurses registered on the
HNHCP Group (Haematology Nurses and Healthcare Professionals Group)
electronic mailing list (2295 individuals) were invited to participate
via email. Researchers were members of the HNHCP Board with access to
the mailing list. The purpose of the survey was explained, and a link
to an online survey (Survey Monkey®, San Mateo, CA, USA) was included.
It was stated that participation was voluntary, and consent was assumed
upon completing the questionnaire. Data collection was anonymous.
Results were available to researchers via password-restricted access.
Questionnaire. Items for the questionnaire were based on the literature about haematology nurses' educational priorities,[22] practice standards and competencies for paediatric non-malignant haematology care[23] and texts relating to advanced nursing practice.[24,25]
The survey questionnaire consisted of 9 subtopics investigating the
demographic details of respondents and asking about the activities
undertaken within their roles such as clinical activities, advanced
practice, education provision (for patients, informal carers and peers/
colleagues), involvement in multidisciplinary team meetings and
decision-making, management responsibilities, involvement in research
and any other areas included in the nurses' role. The questionnaire
also explored perceptions of areas of practice nurses felt should be
included in their role and barriers (including lack of time, skills,
educational opportunities, funding and support) and facilitators
(including protected time, educational courses, funding, managerial
support and medical staff support) to incorporating these into
practice. Resources were reviewed by a research team of four
experienced haematology nurses to agree with the questionnaire content.
The survey was available in the English language.
Statistical analyses.
Descriptive statistics were calculated using the Statistical Package
for Social Sciences (SPSS) version 23.0 (IBM Corp., Armonk, NY), and
data were reported as numbers and percentages. The chi-square test was
used for differences between activities undertaken and the nursing
role. Fisher's exact test was used where frequencies were valued at
less than 5. Statistical significance was set at p-values less than
0.05.
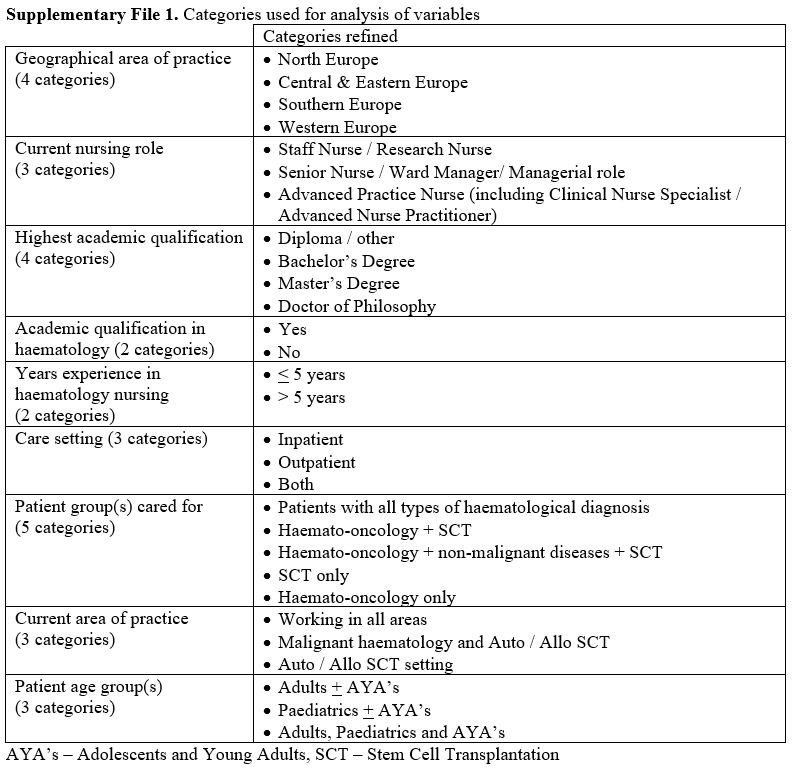
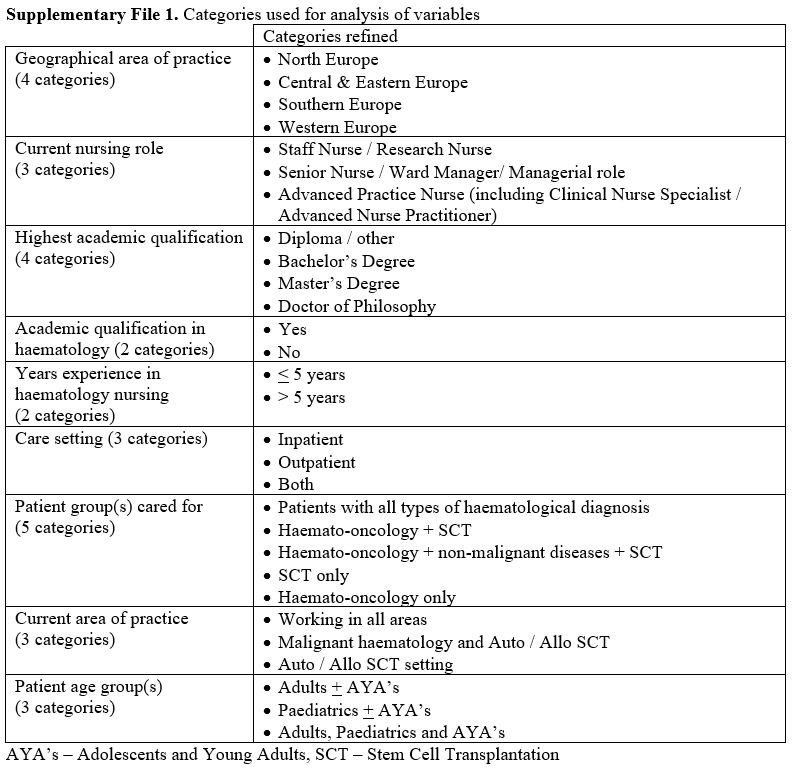
Furthermore, to give an overview of the results, data for
each subtopic has been reduced into categories, e.g. age of respondent,
geographical area of practice, highest academic qualification, patient
group(s) cared for and patient age group(s). Current nursing roles were
grouped according to the role that was predominantly clinically based
(Staff Nurse / Research Nurse), managerial roles (Senior Nurse / Ward
Manager/ Managerial role) or those working at an advanced practice
level (including Clinical Nurse Specialist / Advanced Nurse
Practitioner).
Variables regarding academic qualification in
haematology (completion of a university-recognised course in
haematology), in-house training in haematology (training by local
hospital staff/ employees) and years of experience in haematology
nursing were dichotomised (Supplementary File 1). Qualitative comments collected are summarised within each subtopic.
Results
Sample.
Two thousand two hundred ninety-five nurses were invited to respond to
the survey between January and April 2020, and 238 completed responses
were received. Three respondents from non-European countries were
excluded from the analysis (Turkey, Iraq, and Brazil). Two respondents
described their role as nurse researchers and were excluded from the
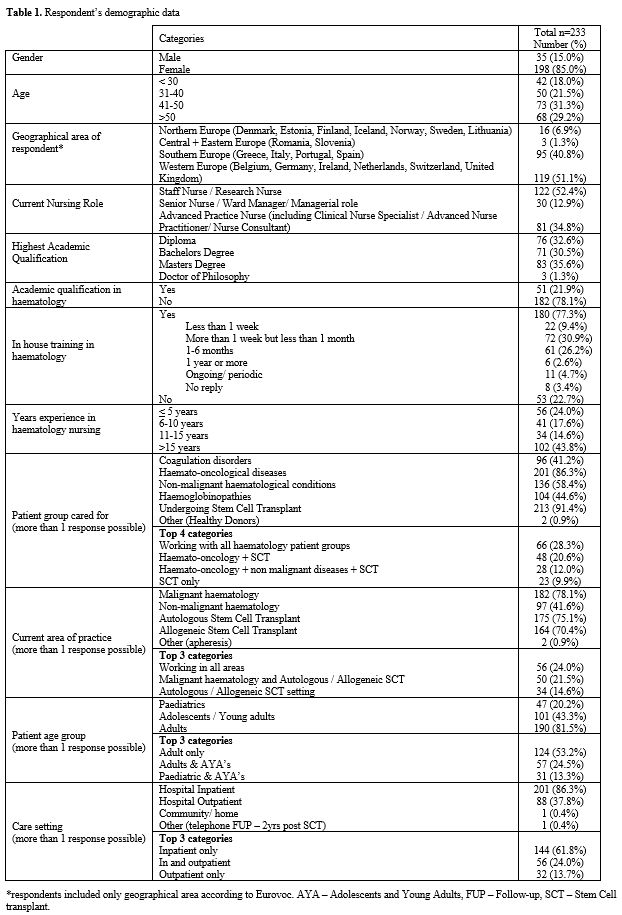
statistical analysis. Table 1
provides a summary of the 233 respondents' characteristics. Respondents
came from 19 countries, principally Western Europe and in particular
Italy, Switzerland and the United Kingdom 82 (35.2%), 47 (20.2%), and
26 (11.2%), respectively. The majority of respondents were female 198
(85.0%), aged 41-50 years of age 73 (31.3%), with the majority working
as Staff Nurses (SN) or Research Nurses (ResN) 122 (52.4%). Over a
third of respondents worked in Advanced Nursing Practice roles, 81
(34.8%), mostly from Western European countries (p = .000). One-third
were in managerial roles, 30 (12.9%).
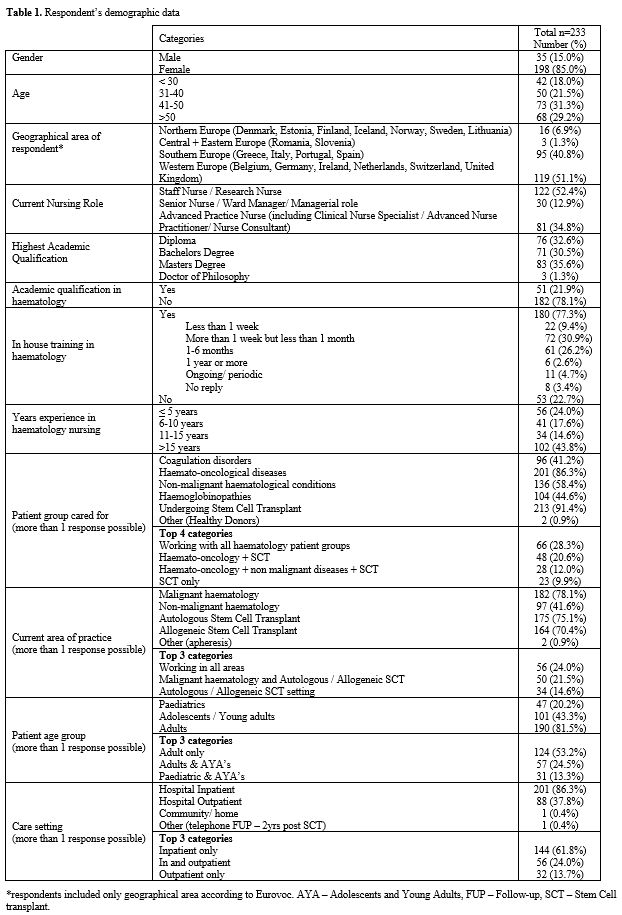 |
- Table
1. Respondent’s demographic data
|
Most
respondents were educated to Bachelor's degree level or above 157
(67.4%), with over half of Nurse Managers (NMs) and Advanced Practice
Nurses (APNs) educated to Master's degree level (p < .001). Less
than a quarter of nurses had an academic qualification in haematology
51 (21.9%), with the majority of nurses reporting this qualification,
working as APNs (p = .000). In-house training in haematology was more
common across the respondents 180 (77.3%); however, the duration of
in-house training varied, frequently described as being 'more than 1
week but less than 1 month' 72 (30.9%).
Most respondents worked
within haematology for more than 5 years 177 (76.0%). Almost half of
the respondents had worked for more than 15 years in haematology
nursing 102 (43.8%); in particular, these were NMs 18 (60.0%) and APNs
48 (59.3%) (p < .001). The majority of respondents cared for
patients affected by malignant haematological conditions 201 (86.3%) or
non-malignant conditions 136 (58.4%), and nurses caring for patients
with coagulation disorders and hemoglobinopathies were also well
represented 96 (41.2%), and 104 (44.6%). Two respondents cared for
healthy donors and worked in apheresis. Most respondents cared for
patients undergoing Stem Cell Transplant 213 (91.4%), including
autologous Stem Cell Transplant 175 (75.1%) and allogeneic Stem Cell
Transplant 104 (70.4%), and worked in autologous and/or allogeneic stem
cell transplant settings (175, 75.1%; 164, 70.4%, respectively). No
significant differences in the distribution of patients cared for were
seen between nursing role categories.
The majority of nurses
worked with adult patients, only 124 (53.2%), or adult and adolescent/
young adult (AYA) patients, 57 (24.5%). Nurses working with paediatric
and/or AYA patients represented 13.3% (39) of the sample. A greater
proportion of APNs worked with adult patients 49 (60.5%); however, the
finding was not statistically significant.
Inpatient care settings
were the most frequently reported place of work 201 (86.3%), in
particular by SN, ResN and NMs; however, 56 respondents were working
across in- and outpatient settings (24.0%), in particular, APNs 37
(45.7%) (p < .001).
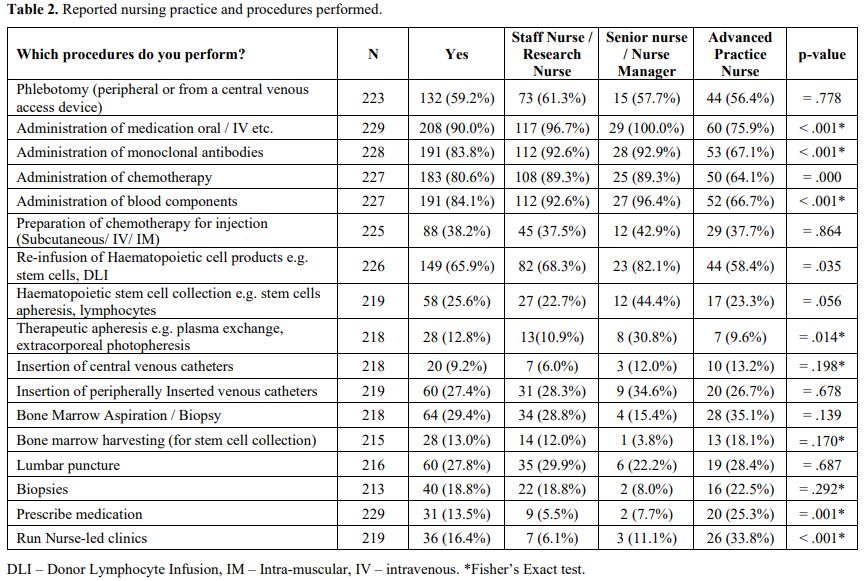
Nursing practice and procedures.
Respondents were asked to identify which activities they performed as
part of their nursing practice. Findings are summarised in Table 2.
Just over half of the sample was used to perform phlebotomy procedures
peripherally or centrally 132 (59.2%). The majority of nurses were
involved in medication administration, including oral and intravenous
(IV) treatments, monoclonal antibodies and chemotherapy 208 (90%), 191
(83.8%), and 183 (80.6%), respectively. Over half of the nurses
reported having received specialist training for drug/ treatment
administration 110 (46.2%), in particular chemotherapy, monoclonal
antibodies and Chimeric Antigen Receptor T-cells.
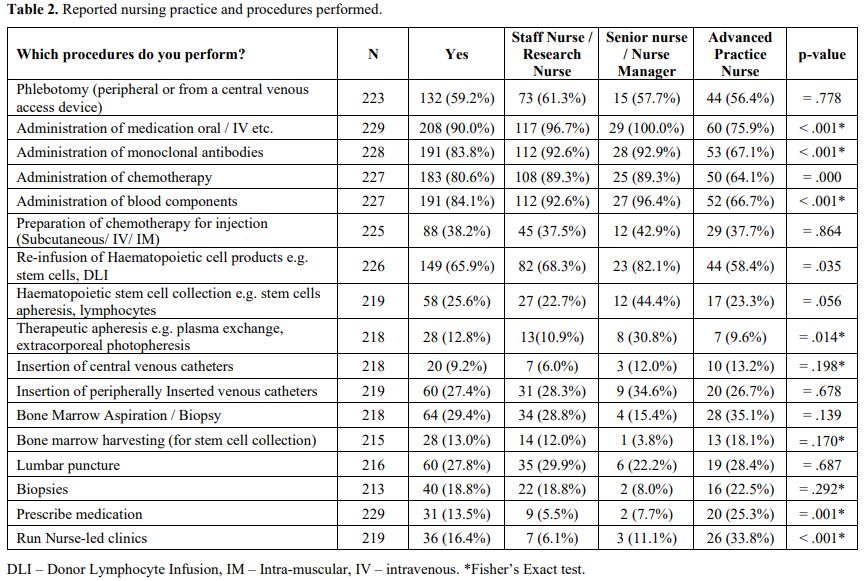 |
- Table
2. Reported nursing practice and procedures performed
|
Over
one-third of nurses reported they prepared chemotherapy for injection
88 (38.2%), the majority being respondents from Italy 36 (43.9% of all
Italian respondents) and Switzerland 17 (36.2% of all Swiss
respondents), and just six (6.8%) of those preparing chemotherapy
reported having received specific training in chemotherapy handling.
Administration of blood components was also common practice 227
(81.4%), with fewer being APNs (p < .001).
Many nurses were
used to performing reinfusion of haematopoietic cell products 149
(65.9%), more so the SN/ ResN group and Senior/ NMs (p = .035). Stem
cell collection and therapeutic apheresis were less common practice
procedures across 58 respondents (25.6%) and 28 (12.8%), respectively,
more commonly performed by Senior/ NMs.
Regarding other advanced
practice procedures, a few nurses were used inserting Central Venous
Catheters (CVCs), 20 (9.2%), primarily APNs. Insertion of Peripherally
Inserted Central Catheters (PICCs) was more common 60 (27.4%), mostly
reported by the SNs / ResN group. Performance of bone marrow
aspiration/biopsy was reported by almost one-third of sample 64 (29.4%)
by both APNs and SNs/ ResN. In comparison, bone marrow harvesting for
stem cell collection was an uncommon procedure in this sample 28
(13.0%) performed by these same nursing groups. Some nurses also
reported performing lumbar punctures 60 (27.8%) and biopsies 40
(18.8%), mainly from Italy and Switzerland. Other activities that
nurses reported included assisting medical staff in performing
procedures such as bone marrow aspiration/ biopsy, harvesting or lumbar
puncture, clinical examination of patients, Chimeric Antigen Receptor
T-cell Therapy coordination, and vaccination.
Thirty-one (13.5%)
nurses reported prescribing medication for their patients, the majority
being from Western European Countries 20 (p = .406) and APNs (p =
.001). Three respondents described prescribing medication for CVCs and
skin problems, while the remaining covered patients with differing
haematological diagnoses, treatment and supportive care areas.
Thirty-six
(16.4%) nurses reported running nurse-led clinics, the majority being
from Western European Countries 26 (p = .007) and APNs (p < .001).
Types of clinics reported were transplant-related (donor care, pre-Stem
Cell Transplant clinics, post allogeneic Stem Cell Transplant,
myelosuppression medication, late effects), supportive care
(transfusion support, medical devices), disease-specific (haemophilia,
immune thrombocytopenia, myeloma, myeloproliferative neoplasms,
leukaemia, lymphoma), non-disease specific (oral therapies, long term
follow up, older patients).
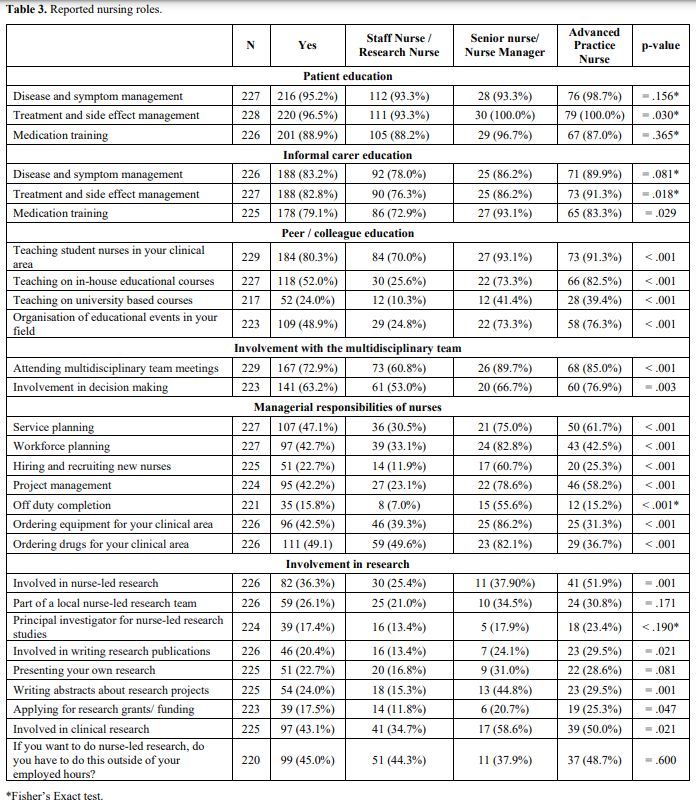
Roles in education.
Independent of their role, nurses widely acknowledged their role in
patient education regarding disease and symptom management 216 (95.2%),
treatment and side effect management 220 (96.5%), and medication
training 201 (88.9%) (Table 3).
Other educational examples were Stem Cell Transplant related (the
pathway, self-care after discharge), management of CVCs, and general
topics (nutrition, hygiene and infection prevention, lifestyle
education, sexuality, and coping).
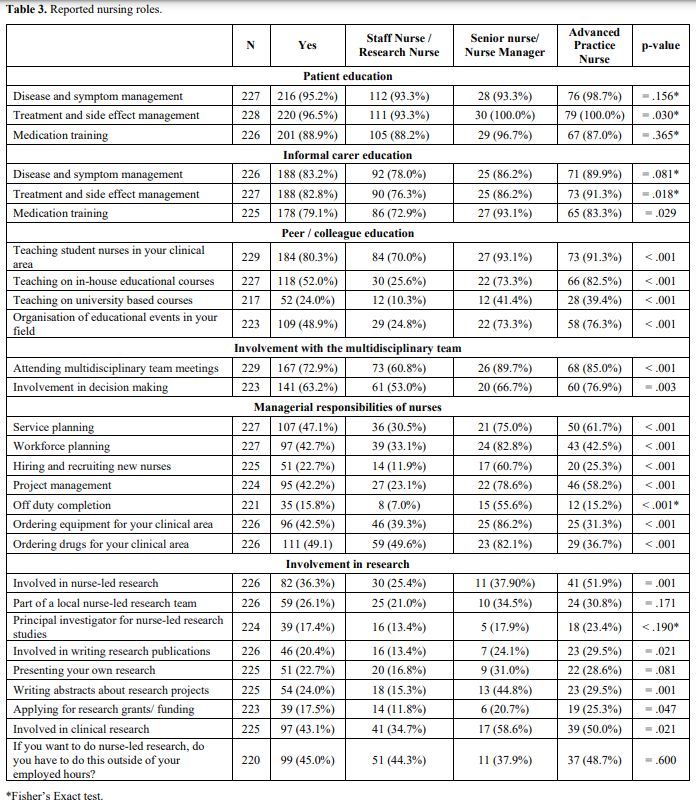 |
- Table 3. Reported nursing roles
|
Education
of informal carers was also seen as a regular part of the nurse's role,
covering disease and symptom management 188 (83.2%), treatment and side
effect management 188 (82.8%), and medication training 178 (79.1%).
Other topics reflected those described above and the performance of
subcutaneous injections.
Peer/colleague education with student
nurses in the clinical area was prevalent 184 (80.3%), mostly reported
by Senior/NMs and APNs. Nurses in these roles were also more frequently
involved in teaching in-house courses, university-based courses and
organising educational events. However, these were overall a less
common role for nurses 118 (52.0%), 52 (24.0%), and 109 (48.9%),
respectively. All findings were statistically significant (p <
.001). Other involvements in education were described, including
education for high schools and patient forums. Overall, nurses
described education to all three groups as a very high/ high priority
within their roles 216 (93.9%), 200 (88.8%), and 200 (88.5%),
respectively.
Role in the Multidisciplinary Team.
The majority of nurses gave a high/ very high priority to involvement
in the multidisciplinary team as part of their role 186 (84.6%), with
many being directly involved in meetings 167 (72.9%), but somewhat
fewer involved in the decision-making process 141 (63.2%) (Table 3). In both cases, these roles were primarily reported by Senior/NMs and APNs (p < .001, p = .003, respectively).
Management responsibilities. Many nurses reported management responsibilities within their roles, not only those in posts of nursing management (Table 3).
Service and workforce planning activities were more common for Senior /
NMs, just one-third of SNs/ ResN reported this as part of their role (p
< .001). Hiring and recruitment primarily comprised Senior/ NMs 17
(60.7%), whereas project management involved APNs. Interestingly, only
35 (15.8%) respondents performed off-duty completion, mostly Senior/
NMs. Ordering drugs and equipment for the clinical area was also a role
reported by this group of nurses, 25 (86.2%) and 23 (82.1%),
respectively.
Research roles. Involvement in nurse-led research was much less frequent as a part of nurses' practice (Table 3).
Over one-third of nurses participated in nurse-led research 82 (36.3%),
the majority being APNs (51.9%) (p = .001). Over a quarter of nurses
said they were part of a local research team 59 (26.1%), but few nurses
were lead investigators for studies 39 (17.4%), a finding similar
across the groups of respondents. Writing and presenting research 51
(22.7%), 54 (24.0%), respectively, and applying for grants and funding
39 (17.5%), were again less common activities more often performed by
Senior/NMs and APN groups. The majority of nurse-led research
activities were reported by respondents from Western and Southern
European countries, although the findings were not statistically
significant. Of greater prevalence was nursing involvement in clinical
research 97 (43.1%).
Almost half of the nurses said that
nurse-led research had to be done outside of employed hours 99 (45.0%),
particularly for Southern European respondents 53 (56.4%) (p = 0.016).
Additional comments highlighted that nurse-led research must be done
within and outside working hours or negotiated in some cases. The
research was given a very high/ high priority by just over half of the
respondents 125 (57.6%), mainly by respondents from Southern European
Countries 72 (77.4%) (p < .001).
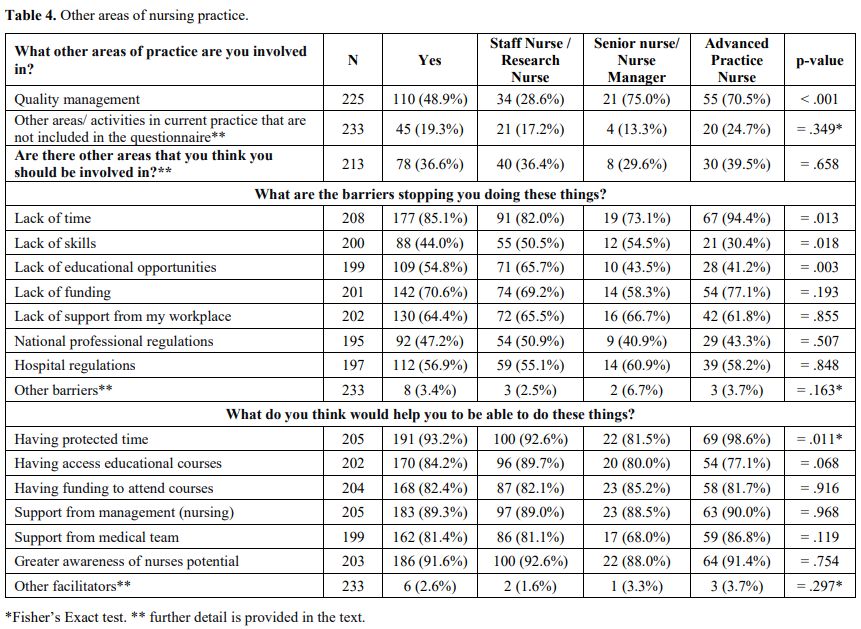
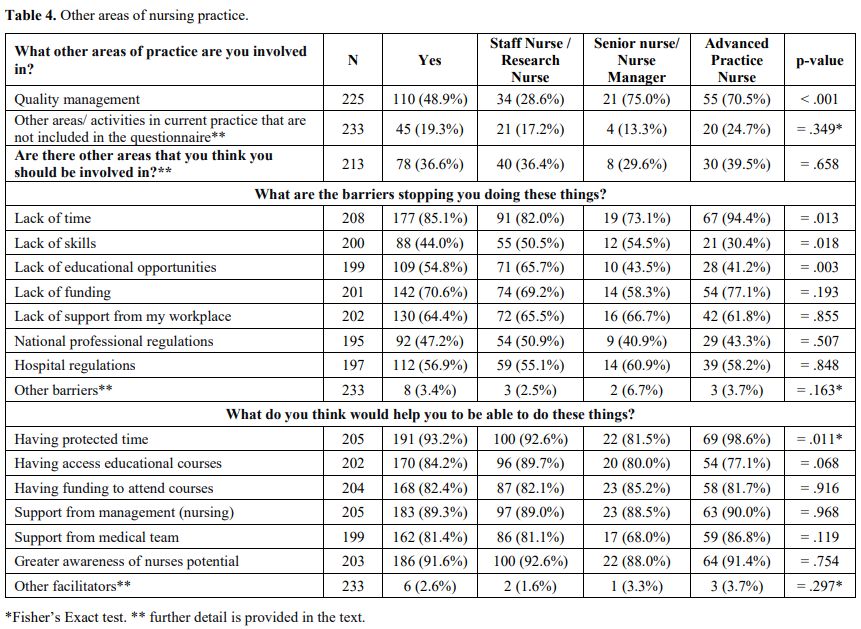
Other areas of practice.
Other areas of current practice reported as being undertaken by
respondents included hospital-wide practice development, quality
management, risk management, data management (completing Stem Cell
Transplant reporting forms), membership of Ethics Committees, and
University professors (Table 4).
One-third of nurses felt that there were other areas they should be
involved in but were not currently part of their practice, including
undertaking advanced practice roles (clinical assessment, prescribing,
nurse-led clinics, case management, virtual and telephone clinics,
performing ultrasound), direct patient care (nutrition, palliative
care, psychological care), nurse-led research and evidence-based
practice (including Stem Cell Transplant), decision making &
multidisciplinary team meeting participation (inc. advanced care
planning), managerial roles (budgeting, planning of medical staff
rotations), education (integrated courses, nurse education), and
involvement with primary care services.
 |
- Table 4. Other areas of nursing practice
|
Perceived
barriers to performing these additional roles included lack of time 177
(85.1%), lack of skills 88 (44.0%), lack of education opportunities 109
(54.8%), lack of funding 142 (70.6%), lack of workplace support 130
(64.4%), national professional regulations 92 (47.2%), hospital
regulations 112 (56.9%). Other barriers included poor managerial
support, shift allocation, and lack of administrative support and space.
Respondents
felt that they would be aided in performing these additional roles if
they had protected time 191 (93.2%), access to educational courses 170
(84.2%), funding to attend courses 168 (82.4%), support from nursing
management 183 (89.3%), support from the medical team 162 (81.4%), and
greater awareness of nurses potential 186 (91.6%). Greater
collaboration across haematology departments was also suggested.
.
Discussion
The
study provides greater comprehension of the current clinical and
non-clinical roles of nurses working within the haematology setting
across various countries. While most respondents worked in SN / ResN
roles, extended practice activities and APNs were evident.
Results demonstrated congruence with many activities cited in haematology patient care educational programs;[23] however, there are changes in reported practice compared with a previous survey investigating haematology nurses' role.[18]
Patients
with haematological conditions often undergo blood sampling to evaluate
a range of values, including cell counts, renal and hepatic
functioning, and disease status; however, just over half of the
respondents were involved in blood sampling. This procedure is not part
of the usual activities for many nurses surveyed, and in some
countries, the procedure is often performed by non-nursing personnel.[26]
The
role of nurses in medication management includes a variety of
responsibilities, not only administration but managing therapeutic and
adverse effects, adherence, self-management, education, safety and care
transition.[27] There are continuously emerging therapies for malignant and non-malignant haematological conditions,[28,29] some requiring enhanced knowledge regarding administration techniques, side effect monitoring and management.[30]
Nearly half of the sample reported having specific training for
traditional treatment agents such as chemotherapy and innovative
monoclonal antibody treatments and Chimeric Antigen Receptor -T cell
therapy where treatment side effects include cytokine release and
neurological toxicity and nursing management may be novel.[31]
The preparation of chemotherapy in hospitals and daycare units is a nursing procedure in some centres and countries.[32,33]
While we observed few respondents preparing chemotherapy that reported
having received specific training, it should be noted that European
Parliament has provided legislation regarding the protection of workers
from risks related to exposure to carcinogens,[34,35]
and guidance is available for the safe handling of hazardous drugs for
nurses in oncology emphasising the importance of documented training
and competency.[36]
Transfusion of blood and blood products is part of routine practice due to their life-saving and therapeutic effects[37]
and is commonly performed by nurses; however, infusion of stem cells is
traditionally performed by medical staff or APNs. However, the
literature provides evidence of nurse administration,[38]
as is reported in this sample. A 2007 survey of the haematology nurses'
role highlighted the administration of cytotoxic agents, supportive
care treatments and managing related side effects as activities
performed mostly by unit-based nurses and NMs but also Clinical Nurse
Specialists,[18] reflecting findings in this study.
Apheresis
procedures were less frequently reported aspects of nurses' roles,
particularly senior nurses. This niche nursing field requires specific
training in using an apheresis machine, often in designated units with
Nurse Practitioners and Lead Nurses guiding the team.[39]
While
nurses are frequently involved in the management of venous access
devices, the insertion by nurses of central venous access devices, such
as Peripherally Inserted Central Catheters or Central Venous Catheters,
is traditionally performed by nurses within advanced practice roles;[40] however, in this sample we observed SNs performing this role.
Clinical
procedures often performed within a haematology setting, including bone
marrow aspiration and biopsy, bone marrow harvesting, lumbar puncture
and skin biopsies, are suggested to be competencies within a Nurse
Practitioner role;[21] however, we again observed
reports of SNs performing these procedures which may reflect evidence
of advanced practice without changes within a job title. However, as
many respondents also described how they assisted medical staff with
the procedures, it may be that the question was misinterpreted.
In
2019, nurse prescribing of medicines had been authorised in 13
countries across a range of nursing roles, with educational
requirements varying from being part of nurse education, to those
additional education courses, without necessarily having an APN title.[41] Results from this study reflect this finding, with just over one-third of nurse prescribers not working in APN roles.
A
small proportion of nurses in this sample reported prescribing
medicines in countries where this is not legal, which may reflect
informal prescribing practices.[12]
Nurse-led clinics for patients with haematological disorders have been reported in the literature,[42-44] including APNs running post-disease and treatment survivorship clinics with similar findings in this sample.
Many
of the clinical activities reported by nurses in this survey were not
reported in a previous survey of haematology nursing activities,[18]
which may suggest a trend towards the development of advanced clinical
skills and innovative changes in practice to address service needs.
Education is described as one of the key nursing roles[45] and recognised activity of haematology nurses.[18]
Unsurprisingly this was echoed throughout the respondents in this
sample, providing patient care and peer education. In some countries,
APNs are a standard multidisciplinary team component for patients with
haematological conditions.[46] While involvement in
multidisciplinary team meetings was evident for respondents of all
nursing roles in this study, fewer felt part of the decision-making
process. What can be classed as traditionally managerial roles for
nurses[47] were sometimes reported as being performed
by those outside a managerial role. Possible reasons may include an
approach to prepare future NMs or a redistribution of duties according
to workload.
Nursing research activities were undertaken by just
one-third of respondents, often reporting that this was 'outside
working hours'. Acceptance by managers and facilitation of resources
from both managers and the organisation are attributes of a nursing
research culture;[48] however, few clinical areas can claim to have research positions held by academically trained nurses.[49]
The importance of nursing research to inform evidence-based practice is
fundamental and should be promoted at a European level.
Respondents
in this study highlighted various other areas of practice where they
worked and also areas where they felt they should have a role,
particularly in advanced nursing practice roles, research and
evidence-based practice (EBP), management and education. Many of these
roles require specific competencies and skills, and a lack of skills
and educational opportunities were often cited as barriers to role
development. Attendance at educational conferences is a preferred
method for learning expressed by haematology nurses, allowing
interaction and networking.[22] Of concern is that
these issues impacting role development are more frequently reported
than similar research reported 10 years ago.[18]
Strategies are necessary to ensure that nurses are facilitated in
practice development to meet the complex needs of haematology patients.
The study has identified various clinical and non-clinical
professional practices performed by haematology nurses, with some
differences observed between nursing roles. Evident across all roles
was medication management, ranging from administration to symptom
management, and nurses' key role in patient and caregiver education.
Technical and advanced practice activities, as well as nurse-led
research, were more frequently performed by nurses in APN roles,
whereas both APNs and Senior / NMs had a greater managerial activity.
Although a minority of nurses responded that there were other areas of
practice they felt they should be involved in, no differences were seen
in perceived barriers or facilitators according to the role.
This
survey has provided an important overview of the professional practices
of haematology nurses; however, the study has limitations. The total
number of respondents is small in light of the overall number of nurses
working with haematology patients. As such, these findings cannot be
said to be representative of all nurses or countries. While the study
also aimed to investigate differences according to country of practice,
as two-thirds of the responses were from 3 countries, it was impossible
to make inferences regarding the country. The majority of respondents
worked with patients affected by both malignant and non-malignant
haematological disorders. Therefore, it was impossible to describe the
role of nurses working only with patients affected by non-malignant
haematological conditions. The survey was only available in the English
language, which may have limited completion by some nurses. A
convenience sample was used for the survey, accessed through a
haematology nursing organisation mailing list, aiming to capture
responses from nurses with experience in the speciality. However, it is
recognised that this may bias results towards more experienced nurses
and the tasks and roles reported. Nurses choosing to respond may be
interested in sharing details of their role and activities.
Conclusion
Differences
in haematology nursing practice are observed according to the nursing
roles and some countries' behaviours. The nursing care activities
reported in this article reflect the performance of traditional roles
such as drug administration and education, with developments in the
care of patients affected by haematological conditions, improved
survivorship and ever-evolving therapeutic strategies, requiring
adaptation of nursing care activities to support patients. New
activities reported in nursing practice may reflect new treatment
regimens, task shifting, and regulatory developments. Policy reforms in
some countries now permit expanded nursing roles supported by
supplementary education. All this was evident within the extended
practice roles in the haematology setting, often highlighting
discrepancies between the use of APN titles and activities reported.
These findings can be used to map trends in nursing activity and
contribute to the discussion of a core skills framework for nurses
working within different roles within the haematology setting.
References
- World Health Organization. Data and Statistics. https://www.euro.who.int/en/health-topics/Health-systems/nursing-and-midwifery/data-and-statistics No date. Accessed: 25 May 2021
- Eurostat. Ageing Europe - statistics on population developments. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Ageing_Europe_-_statistics_on_population_developments#:~:text=The%20population%20of%20older%20people,reach%20129.8%20million%20by%202050 2020. Accessed: 25 May 2021
- Busse
R, Blümel M, Scheller-Kreinsen D, Zenter A. Tackling Chronic Disease In
Europe: Strategies, interventions and challenges. Observatory Studies
Series No 20. World Health Organization, on behalf of the European
Observatory on Health Systems and Policies, UK. 2020.
- Organisation
for Economic Cooperation and Development. Caring for Quality in Health:
Lessons Learnt from 15 Reviews of Health Care Quality, OECD Reviews of
Health Care Quality, OECD Publishing, Paris. https://doi.org/10.1787/9789264267787-en 2017. Accessed: 20 May 2021
- International Council of Nurses. Scope of Nursing Practice: Position Statement. https://www.icn.ch/sites/default/files/inline-files/B07_Scope_Nsg_Practice.pdf 2013. Accessed: 25 May 2021
- Mackey
H, Noonan K, Kennedy Sheldon L, Singer M, Turner T. Oncology Nurse
Practitioner Role: Recommendations From the Oncology Nursing Society's
Nurse Practitioner Summit. Clin J Oncol Nurs. 2018 Oct 1;22(5):516-522.
doi: 10.1188/18.CJON.516-522. https://doi.org/10.1188/18.CJON.516-522 PMid:30239518
- Park
J, Athey E, Pericak A, Pulcini J, Greene J. To What Extent Are State
Scope of Practice Laws Related to Nurse Practitioners' Day-to-Day
Practice Autonomy? Med Care Res Rev. 2018 Feb;75(1):66-87. doi:
10.1177/1077558716677826. https://doi.org/10.1177/1077558716677826 PMid:29148318
- Nursing
and Midwifery Council. Future nurse: standards of proficiency for
registered nurses.
https://www.nmc.org.uk/globalassets/sitedocuments/education-standards/future-nurse-proficiencies.pdf
2018. Accessed: 27 May 2021
- Wilson D. Nurse Practitioners: The Early Years (1965-1974). Maine Nurse Practitioner Association, Maine. 2003.
- Sheer
B, Wong FK. The development of advanced nursing practice globally. J
Nurs Scholarsh. 2008;40(3):204-11. doi:
10.1111/j.1547-5069.2008.00242.x. https://doi.org/10.1111/j.1547-5069.2008.00242.x PMid:18840202
- Kelly
D, Lankshear A, Wiseman T, Jahn P, Mall-Roosmäe H, Rannus K,
Oldenmenger W, Sharp L. The experiences of cancer nurses working in
four European countries: A qualitative study. Eur J Oncol Nurs. 2020
Dec;49:101844. doi: 10.1016/j.ejon.2020.101844. https://doi.org/10.1016/j.ejon.2020.101844 PMid:33166924 PMCid:PMC7556264
- Maier
CB, Köppen J, Busse R; MUNROS team. Task shifting between physicians
and nurses in acute care hospitals: cross-sectional study in nine
countries. Hum Resour Health. 2018 May 25;16(1):24. doi:
10.1186/s12960-018-0285-9. https://doi.org/10.1186/s12960-018-0285-9 PMid:29801452 PMCid:PMC5970499
- Pulte
D, Jansen L, Brenner H. Changes in long term survival after diagnosis
with common hematologic malignancies in the early 21st century. Blood
Cancer J. 2020 May 13;10(5):56. doi: 10.1038/s41408-020-0323-4. https://doi.org/10.1038/s41408-020-0323-4 PMid:32404891 PMCid:PMC7221083
- Einsele
H, Briones J, Ciceri F, García-Cadenas I, Falkenburg F, Bolaños N,
Heemskerk HMM, Houot R, Hudecek M, Locatelli F, Morgan K, Morris CE,
O'Dwyer M, Gil JS, van den Brink M, van de Loosdrecht AA. Immune-based
Therapies for Hematological Malignancies: An Update by the EHA SWG on
Immunotherapy of Hematological Malignancies. Hemasphere. 2020 Jun
29;4(4):e423. doi: 10.1097/HS9.0000000000000423. https://doi.org/10.1097/HS9.0000000000000423 PMid:32904089 PMCid:PMC7448369
- Bertucci
F, Le Corroller-Soriano AG, Monneur-Miramon A, Moulin JF, Fluzin S,
Maraninchi D, Gonçalves A. Outpatient Cancer Care Delivery in the
Context of E-Oncology: A French Perspective on "Cancer outside the
Hospital Walls". Cancers (Basel). 2019 Feb 14;11(2):219. doi:
10.3390/cancers11020219. https://doi.org/10.3390/cancers11020219 PMid:30769858 PMCid:PMC6406853
- Farrell
C, Walshe C, Molassiotis A. Are nurse-led chemotherapy clinics really
nurse-led? An ethnographic study. Int J Nurs Stud. 2017 Apr;69:1-8.
doi: 10.1016/j.ijnurstu.2017.01.005. https://doi.org/10.1016/j.ijnurstu.2017.01.005 PMid:28113082
- Lemonde
M, Payman N. Perceived roles of oncology nursing. Can Oncol Nurs J.
2015 Fall;25(4):422-42. doi: 10.5737/23688076254422431. https://doi.org/10.5737/23688076254422431 PMid:26897865
- Aerts
E, Fliedner M, Redmond K, Walton A. Defining the scope of haematology
nursing practice in Europe. Eur J Oncol Nurs. 2010 Feb;14(1):55-60.
doi: 10.1016/j.ejon.2009.06.008. https://doi.org/10.1016/j.ejon.2009.06.008 PMid:19734088
- Schrijvers
L, Bedford M, Elfvinge P, Andritschke K, Leenders B, Harrington C. The
role of the European haemophilia nurse. J Haem Pract. 2013. 1(1):24-7.
doi: 10.17225/jhp.00008 https://doi.org/10.17225/jhp.00008
- EAHAD
Nurses Committee; Harrington C, Bedford M, Andritschke K, Barrie A,
Elfvinge P, Grønhaug S, Mueller-Kagi E, Leenders B, Schrijvers LH. A
European curriculum for nurses working in haemophilia. Haemophilia.
2016 Jan;22(1):103-9. doi: 10.1111/hae.12785. https://doi.org/10.1111/hae.12785 PMid:26278710
- Knopf
KE. Core competencies for bone marrow transplantation nurse
practitioners. Clin J Oncol Nurs. 2011 Feb;15(1):102-5. doi:
10.1188/11.CJON.102-105 https://doi.org/10.1188/11.CJON.102-105 PMid:21278047
- Liptrott
S, NíChonghaile M, Aerts E; Haematology Nurses and Healthcare
Professionals Group (HNHCP). Investigating the self-perceived
educational priorities of haematology nurses. Eur J Oncol Nurs. 2019
Aug;41:72-81. doi: 10.1016/j.ejon.2019.05.010. https://doi.org/10.1016/j.ejon.2019.05.010 PMid:31358261
- Atlantic
Provinces Pediatric Hematology Oncology Network (APPHON)/ Réseau
d'Oncologie et Hématologie Pédiatrique des Provinces Atlantiques
(ROHPPA). Practice Standards and Competencies for Nurses Providing
Pediatric Non Malignant Hematology Care in Atlantic Canada https://www.apphon-rohppa.com/en/system/files/u5/Final.hem_nursing.practice_standards_and_competencies.July%202008.pdf 2008. Accessed: 20 October 2019
- Bruinooge
SS, Pickard TA, Vogel W, Hanley A, Schenkel C, Garrett-Mayer E,
Tetzlaff E, Rosenzweig M, Hylton H, Westin SN, Smith N, Lynch C, Kosty
MP, Williams SF. Understanding the Role of Advanced Practice Providers
in Oncology in the United States. J Oncol Pract. 2018
Sep;14(9):e518-e532. doi: 10.1200/JOP.18.00181. https://doi.org/10.1200/JOP.18.00181 PMid:30133346
- Canadian Nursing Association. Advanced Practice Nursing: a Pan-Canadia Framework. https://www.cna-aiic.ca/-/media/cna/page-content/pdf-en/advanced-practice-nursing-framework-en.pdf?la=en&hash=76A98ADEE62E655E158026DEB45326C8C9528B1B 2019. Accessed: 15 October 2019
- Simundic
A. Who is Doing Phlebotomy in Europe?. In: Guder W, Narayanan S, eds.
Pre-Examination Procedures in Laboratory Diagnostics: Preanalytical
Aspects and their Impact on the Quality of Medical Laboratory Results.
Berlin, München, Boston: De Gruyter, 2015; 90-94. https://doi.org/10.1515/9783110334043-015
- De
Baetselier E, Dilles T, Feyen H, Haegdorens F, Mortelmans L, Van
Rompaey B. Nurses' responsibilities and tasks in pharmaceutical care: A
scoping review. Nurs Open. 2022 Nov;9(6):2562-2571. doi:
10.1002/nop2.984. https://doi.org/10.1002/nop2.984 PMid:34268910 PMCid:PMC9584497
- Hou
JZ, Ye JC, Pu JJ, Liu H, Ding W, Zheng H, Liu D. Novel agents and
regimens for hematological malignancies: recent updates from 2020 ASH
annual meeting. J Hematol Oncol. 2021 Apr 21;14(1):66. doi:
10.1186/s13045-021-01077-3. https://doi.org/10.1186/s13045-021-01077-3 PMid:33879198 PMCid:PMC8059303
- Neumayr
LD, Hoppe CC, Brown C. Sickle cell disease: current treatment and
emerging therapies. Am J Manag Care. 2019 Nov;25(18 Suppl):S335-S343.
- Szoch
S, Boord C, Duffy A, Patzke C. Addressing Administration Challenges
Associated With Blinatumomab Infusions: A Multidisciplinary Approach. J
Infus Nurs. 2018 Jul/Aug;41(4):241-246. doi:
10.1097/NAN.0000000000000283. https://doi.org/10.1097/NAN.0000000000000283 PMid:29958260
- Beaupierre
A, Kahle N, Lundberg R, Patterson A. Educating Multidisciplinary Care
Teams, Patients, and Caregivers on CAR T-Cell Therapy. J Adv Pract
Oncol. 2019 May-Jun;10(Suppl 3):29-40. doi:
10.6004/jadpro.2019.10.4.12. https://doi.org/10.6004/jadpro.2019.10.4.12 PMid:33520344 PMCid:PMC7521122
- Koulounti
M, Roupa Z, Charalambous C, Noula M. Assessment of Nurse's Safe
Behavior Towards Chemotherapy Management. Mater Sociomed. 2019
Dec;31(4):282-285. doi: 10.5455/msm.2019.31.282-285. https://doi.org/10.5455/msm.2019.31.282-285 PMid:32082094 PMCid:PMC7007613
- Ulas
A, Silay K, Akinci S, Dede DS, Akinci MB, Sendur MA, Cubukcu E, Coskun
HS, Degirmenci M, Utkan G, Ozdemir N, Isikdogan A, Buyukcelik A, Inanc
M, Bilici A, Odabasi H, Cihan S, Avci N, Yalcin B. Medication errors in
chemotherapy preparation and administration: a survey conducted among
oncology nurses in Turkey. Asian Pac J Cancer Prev.
2015;16(5):1699-705. doi: 10.7314/apjcp.2015.16.5.1699. https://doi.org/10.7314/APJCP.2015.16.5.1699 PMid:25773812
- Directive
(EU) 2022/431 of the European Parliament and of the Council of 9 March
2022 amending Directive 2004/37/EC on the protection of workers from
the risks related to exposure to carcinogens or mutagens at work. 2022.
Official Journal L88/1. http://data.europa.eu/eli/dir/2022/431/oj Accessed: 12 Mar 2023
- Directive
2004/37/EC of the European Parliament and of the Council of 29 April
2004 on the protection of workers from the risks related to exposure to
carcinogens or mutagens at work (Sixth individual Directive within the
meaning of Article 16(1) of Council Directive 89/391/EEC) (codified
version) (Text with EEA relevance). 2004. Official Journal L158/50. http://data.europa.eu/eli/dir/2004/37/oj Accessed: 12 Mar 2023.
- Oncology Nursing Society. Toolkit for Safe Handling of Hazardous Drugs for Nurses in Oncology. https://www.ons.org/sites/default/files/2018-06/ONS_Safe_Handling_Toolkit_0.pdf 2018. Accessed: 25 May 2021
- World Health Organization. 2020, Blood Transfusion. Geneva, Switzerland: World Health Organization, https://www.who.int/news-room/facts-in-pictures/detail/blood-transfusion 2020. Accessed: 10 February 2021
- de
Vera MR, Malick L. Stem Cell Infusion: Changing Practice Through
Education and Collaboration. Biol Blood Marrow Transplant. 2018; 24(3):
S473-S474. https://doi.org/10.1016/j.bbmt.2017.12.753
- Wilson
S, Chauhan A, Morris C, Manton A. Therapeutic apheresis services: a
unique field of nursing within NHSBT. Br J Nurs. 2020 Jun
11;29(11):639-641. doi: 10.12968/bjon.2020.29.11.639. https://doi.org/10.12968/bjon.2020.29.11.639 PMid:32516039
- Ostrowski
AM, Morrison S, O'Donnell J. Development of a Training Program in
Peripherally Inserted Central Catheter Placement for Certified
Registered Nurse Anesthetists Using an N-of-1 Method. AANA J. 2019
Feb;87(1):11-18.
- Maier
CB. Nurse prescribing of medicines in 13 European countries. Hum Resour
Health. 2019 Dec 9;17(1):95. doi: 10.1186/s12960-019-0429-6. https://doi.org/10.1186/s12960-019-0429-6 PMid:31815622 PMCid:PMC6902591
- Overend
A, Khoo K, Delorme M, Krause V, Avanessian A, Saltman D. Evaluation of
a nurse-led telephone follow-up clinic for patients with indolent and
chronic hematological malignancies: a pilot study. Can Oncol Nurs J.
2008 Spring;18(2):64-73. English, French. doi: 10.5737/1181912x1826468.
https://doi.org/10.5737/1181912x1826468 PMid:18649698
- Taylor
K, Chivers P, Bulsara C, Joske D, Bulsara M, Monterosso L. Care After
Lymphoma (CALy) trial: A phase II pilot pragmatic randomised controlled
trial of a nurse-led model of survivorship care. Eur J Oncol Nurs. 2019
Jun;40:53-62. doi: 10.1016/j.ejon.2019.03.005. https://doi.org/10.1016/j.ejon.2019.03.005 PMid:31229207
- Thompson
R, Tonkin J, Francis Y, Pattinson A, Peters T, Taylor M, Wallis L.
Nurse-led clinics for haematological disorders. Cancer Nursing
Practice. 2012. 11(10): 14-20. doi: 10.7748/cnp2012.12.11.10.14.c9472 https://doi.org/10.7748/cnp2012.12.11.10.14.c9472
- International Council of Nurses. The ICN definition of nursing. https://www.icn.ch/nursing-policy/nursing-definitions. 2002. Accessed: 25 May 2021
- National Institute for Clinical Excellence. Haematological cancers: improving outcomes. https://www.nice.org.uk/guidance/ng47 2016. Accessed: 25 May 2021
- American Organization of Nurse Executives. Nurse Manager Competencies. https://www.aonl.org/system/files/medi/file/2019/04/ nurse-manager-competencies.pdf. 2015. Accessed: 12 October 2021
- Berthelsen
CB, Hølge-Hazelton B. 'Nursing research culture' in the context of
clinical nursing practice: addressing a conceptual problem. J Adv Nurs.
2017 May;73(5):1066-1074. doi: 10.1111/jan.13229. https://doi.org/10.1111/jan.13229 PMid:27906467
- Hølge-Hazelton
B, Kjerholt M, Berthelsen CB, Thomsen TG. Integrating nurse researchers
in clinical practice - a challenging, but necessary task for nurse
leaders. J Nurs Manag. 2016 May;24(4):465-74. doi: 10.1111/jonm.12345. https://doi.org/10.1111/jonm.12345 PMid:26667268
Supplementary File 1
 |
- Supplementary File 1. Categories used for analysis of variables.y setting.
|
[TOP]