Management of Portal Vein Thrombosis in Cirrhotic Patients
Lucio Amitrano and Maria Anna Guardascione
UOC di Gastroenterologia, Ospedale A. Cardarelli, Napoli, Italy
Correspondence
to: Lucio Amitrano, Via Morghen, 92, 80129 Naples, Tel.
081-7472453, E-mail: luamitra@tin.it
Published: November 25, 2009
Received: September 25, 2009
Accepted: October 24, 2009
Medit J Hemat Infect Dis 2009, 1(3): e2009014 DOI 10.4084/MJHID.2009.014
This article is available from: http://www.mjhid.org/article/view/5120
This is an Open Access article
distributed under the terms of the
Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited
Abstract
Portal
vein thrombosis (PVT) not associated with hepatocellular carcinoma is
considered a frequent complication of liver cirrhosis but, unlike PVT
occurring in non-cirrhotic patients, very few data are available on its
natural history and management. The reduced portal blood flow
velocity is the main determinant of PVT but, as in other venous
thromboses, multiple factors local and systemic, inherited or acquired
often can concur with. PVT has a variety of clinical presentations
ranging from asymptomatic to life-threatening diseases like
gastroesophageal bleeding or acute intestinal ischemia. It is usually
diagnosed by Doppler ultrasound but computed tomography and magnetic
resonance imaging are useful to study the extent of thrombosis and the
involvement of the abdominal organs. The risk of bleeding mainly
determined by the presence of gastroesophageal varices and clotting
alterations causes concern for the treatment of PVT in cirrhotic
patients. To date, anticoagulant therapy seems to be indicated only in
patients awaiting liver transplantation. This review focuses on the
definition of the subgroups of patients with cirrhosis that might
benefit from treatment of PVT and examines the pros and cons of the
available treatments in terms of efficacy, monitoring and safety,
providing also perspectives for future studies.
Introduction
Liver
cirrhosis is the most frequent underlying disease in patients with
non-neoplastic thrombosis occurring in the portal vein (PVT). In a
large autopsy series of patients with PVT, neoplasia was present in
67%, cirrhosis in 28% and in only 5% of patients PVT was considered
primitive [1]. In view of the recent progress
in the knowledge of
pathogenetic mechanisms, prognosis and therapeutic strategy of PVT
these three clinical conditions have to be considered separately [2-6].
Hepatocellular carcinoma (HCC) is the most frequent cause of PVT in cirrhosis, being present in up to 44% of cases [7] and it has always to be searched for when a new diagnosis of PVT is made.
This review deals with PVT occurring in patients with liver cirrhosis without HCC focusing on the necessity and/or the opportunity of management of this specific complication of liver disease.
Which is the duration of anticoagulation?
The current guidelines for the treatment of venous thromboembolism [86] can be applied to cirrhotic PVT. After an initial 3-6 month period of anticoagulant therapy patients should be separated into the following groups:
So this therapeutic approach in a cirrhotic patient with PVT should be reserved only in the case of patients with ongoing intestinal infarction not responsive to anticoagulation therapy.
Transjugular intrahepatic porto systemic shunt (TIPS) can be considered a second line treatment of PVT in patients with portal hypertensive complications not controlled by the common therapeutic approach particularly in patients awaiting liver transplantation. In preliminary experience Senzolo et al. reported a successful TIPS placement in a 69% of 13 cirrhotic patients with PVT [80]. This procedure is technically feasible also in patient with cavernomatous transformation of portal vein [91-93] unless intrahepatic portal branches are patent.
Hepatocellular carcinoma (HCC) is the most frequent cause of PVT in cirrhosis, being present in up to 44% of cases [7] and it has always to be searched for when a new diagnosis of PVT is made.
This review deals with PVT occurring in patients with liver cirrhosis without HCC focusing on the necessity and/or the opportunity of management of this specific complication of liver disease.
Prevalence
The occurrence of PVT in cirrhotic patients has been increasingly reported in recent years. This stems from the different procedures utilized for diagnosis and the different settings of cirrhotic patients studied. The presence of PVT was 0.6% when evaluated by old angiographic studies8, 4.4% by ultrasound [9] and 10%-12% when more sensitive procedures, i.e. computed tomography (CT) scan and magnetic resonance imaging (MRI) are used [10-11].
Moreover, the prevalence of PVT increases with the age and severity of liver disease reaching 15% in patients awaiting liver transplantation12-15 and 36% in explanted liver at pathological examination [16].
Few studies have focused on the incidence of PVT. The de novo thrombosis within one year, in patients with liver cirrhosis, ranges from 7.4% to 16% [10,17].
The occurrence of PVT in cirrhotic patients has been increasingly reported in recent years. This stems from the different procedures utilized for diagnosis and the different settings of cirrhotic patients studied. The presence of PVT was 0.6% when evaluated by old angiographic studies8, 4.4% by ultrasound [9] and 10%-12% when more sensitive procedures, i.e. computed tomography (CT) scan and magnetic resonance imaging (MRI) are used [10-11].
Moreover, the prevalence of PVT increases with the age and severity of liver disease reaching 15% in patients awaiting liver transplantation12-15 and 36% in explanted liver at pathological examination [16].
Few studies have focused on the incidence of PVT. The de novo thrombosis within one year, in patients with liver cirrhosis, ranges from 7.4% to 16% [10,17].
Etiopathogenesis
It is generally thought that liver cirrhosis leads to a progressive bleeding tendency because of the complex alteration of the clotting system induced by liver failure but recent studies have demonstrated that liver cirrhosis, causing a reduced synthesis of either pro-coagulant or anticoagulant proteins is still associated with a balanced equilibrium of the clotting system set at a lower level [18-22]. A series of acquired or inherited conditions can easily tilt this equilibrium towards either bleeding or thrombosis [23-27].
Epidemiological studies show a prevalence of venous thrombosis of 0.5% - 1% [28-31] in patients with liver cirrhosis is even greater than in the general population, whereas patients with PVT have an elevated risk of developing venous thrombo-embolism outside the splanchnic system [32].
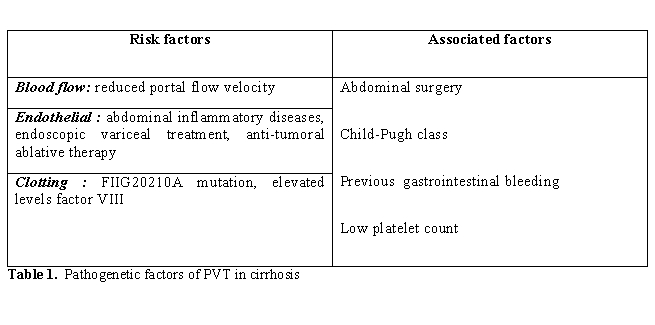
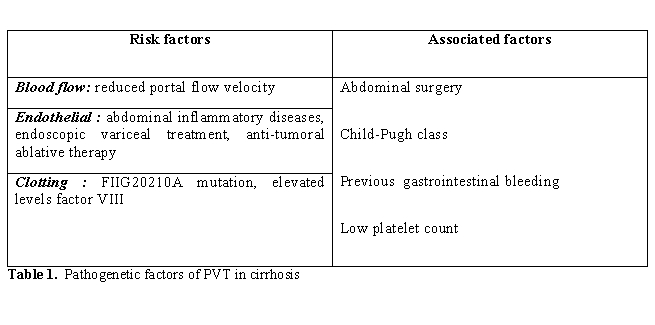
As in all venous thrombosis [33-34] the pathogenesis of PVT in non-cirrhotic [35-36] and in cirrhotic patients [37] is multifactorial, even if not all known risk factors can be studied easily in this setting due to the impaired synthetic and metabolic ability of the liver. Congenital or acquired, local or systemic factors can interact causing reduction of blood flow velocity, endothelial damage and clotting unbalance [38] (Table 1).
It is generally thought that liver cirrhosis leads to a progressive bleeding tendency because of the complex alteration of the clotting system induced by liver failure but recent studies have demonstrated that liver cirrhosis, causing a reduced synthesis of either pro-coagulant or anticoagulant proteins is still associated with a balanced equilibrium of the clotting system set at a lower level [18-22]. A series of acquired or inherited conditions can easily tilt this equilibrium towards either bleeding or thrombosis [23-27].
Epidemiological studies show a prevalence of venous thrombosis of 0.5% - 1% [28-31] in patients with liver cirrhosis is even greater than in the general population, whereas patients with PVT have an elevated risk of developing venous thrombo-embolism outside the splanchnic system [32].
As in all venous thrombosis [33-34] the pathogenesis of PVT in non-cirrhotic [35-36] and in cirrhotic patients [37] is multifactorial, even if not all known risk factors can be studied easily in this setting due to the impaired synthetic and metabolic ability of the liver. Congenital or acquired, local or systemic factors can interact causing reduction of blood flow velocity, endothelial damage and clotting unbalance [38] (Table 1).
In patients with cirrhosis the
derangement of liver architecture leads
to increased intrahepatic vascular resistance, development of
porto-systemic collateral circulation and splanchnic vasodilatation and
ultimately to a stagnation of the portal flow, which is considered the
main predisposing factor to thrombosis.
Zocco et al have recently demonstrated that the portal flow velocity, measured by Doppler ultrasound, is inversely correlated with the risk of PVT [17]. Patients with portal flow velocity less than 15cm/sec have an incidence of PVT of [47]. 8% compared to 2% of those with a velocity > 15 cm/sec. According to most recent hypotheses blood stagnation causes initiation of venous thrombosis through endothelial activation induced by hypoxia secondary to the hemoglobin desaturation [39].Nevertheless, only about 15% of patients with advanced liver disease develop PVT, so all other risk factors implicated in the pathogenesis of venous thrombosis have been searched for in these patients.
The age, sex of the patient and etiology of liver disease have not resulted as risk factors for PVT in patients with cirrhosis, even if a lower prevalence of PVT was reported in PSC and PBC candidates for liver transplantation [12].
Local risk factors may trigger thrombosis via endothelial damage as abdominal inflammatory diseases like diverticulitis, pancreatitis, cholangitis. Abdominal surgical interventions, particularly portal-caval shunts and splenectomy, are associated with PVT [40-41]. The prevalence of other surgical interventions was found higher in cirrhotic patients with PVT in one study [42] but not in others [10,43].
Previous bleeding episodes from gastroesophageal varices11 and their endoscopic treatment [42] resulted as the main endothelial risk factors for PVT and the coexistence of inherited thrombophilia increases this risk [37]. It has been hypothesized that thrombosis develops because of the direct endothelial damage or of the bacteremia induced by the procedures [45]. An increased endotoxemia and clotting activation have been demonstrated in the portal blood that may trigger thrombotic process in these patients [46].
Local ablative therapies, percutaneous ethanol injection and thermotherapy for HCC may induce thrombosis of portal branches close to the tumor [47-49].
The G20210A mutation of the prothrombin is the main inherited clotting abnormality that has been associated with PVT development in liver cirrhosis with a prevalence ranging from 21.4% to 29% and an Odds ratio of 5.910,[43-44]. In a recent study high levels of factor VIII have been found associated with the risk of PVT in patients without cirrhosis [50]. The contribution of factor VIII to PVT in patients with liver cirrhosis remains to be established since high levels of factor VIII are present in the advanced liver disease.
The contribution of FVL, and antiphospho-lipid antibodies to the pathogenesis of PVT in cirrhosis remains controversial. MTHFRTT677 mutation in the absence of hyperhomocysteinemia is not considered a risk factor of venous thromboembolism [43,51-54]. Likewise, the role of inherited natural anticoagulant deficiency (antithrombin, protein C and protein S) in PVT of patients with liver cirrhosis is difficult to establish [55]. In fact, in these patients synthetic dysfunction of the liver leads to a significant reduction of these proteins and an inherited deficiency could be suspected only in the presence of positive familial studies.
In rare cases of PVT associated with recurrent venous thrombosis, or severe presentation with intestinal infarction an underlying myeloproliferative disorder can be suspected [56].
Is it worthwhile performing a complete thrombophilic work-up in the presence of PVT in a cirrhotic patient?
The identification of one or more thrombophilic risk factors in a single patient is interesting for research purposes and it useful in the clinical setting to plan the length of anticoagulant therapy. In fact in patients with “strong” and persistent risk factors anticoagulation has to be prescribed lifelong. In the subgroups of patients with cirrhosis and PVT in which anticoagulation is indicated (see below) the presence of thrombophilia justifies a protracted therapy.
Zocco et al have recently demonstrated that the portal flow velocity, measured by Doppler ultrasound, is inversely correlated with the risk of PVT [17]. Patients with portal flow velocity less than 15cm/sec have an incidence of PVT of [47]. 8% compared to 2% of those with a velocity > 15 cm/sec. According to most recent hypotheses blood stagnation causes initiation of venous thrombosis through endothelial activation induced by hypoxia secondary to the hemoglobin desaturation [39].Nevertheless, only about 15% of patients with advanced liver disease develop PVT, so all other risk factors implicated in the pathogenesis of venous thrombosis have been searched for in these patients.
The age, sex of the patient and etiology of liver disease have not resulted as risk factors for PVT in patients with cirrhosis, even if a lower prevalence of PVT was reported in PSC and PBC candidates for liver transplantation [12].
Local risk factors may trigger thrombosis via endothelial damage as abdominal inflammatory diseases like diverticulitis, pancreatitis, cholangitis. Abdominal surgical interventions, particularly portal-caval shunts and splenectomy, are associated with PVT [40-41]. The prevalence of other surgical interventions was found higher in cirrhotic patients with PVT in one study [42] but not in others [10,43].
Previous bleeding episodes from gastroesophageal varices11 and their endoscopic treatment [42] resulted as the main endothelial risk factors for PVT and the coexistence of inherited thrombophilia increases this risk [37]. It has been hypothesized that thrombosis develops because of the direct endothelial damage or of the bacteremia induced by the procedures [45]. An increased endotoxemia and clotting activation have been demonstrated in the portal blood that may trigger thrombotic process in these patients [46].
Local ablative therapies, percutaneous ethanol injection and thermotherapy for HCC may induce thrombosis of portal branches close to the tumor [47-49].
The G20210A mutation of the prothrombin is the main inherited clotting abnormality that has been associated with PVT development in liver cirrhosis with a prevalence ranging from 21.4% to 29% and an Odds ratio of 5.910,[43-44]. In a recent study high levels of factor VIII have been found associated with the risk of PVT in patients without cirrhosis [50]. The contribution of factor VIII to PVT in patients with liver cirrhosis remains to be established since high levels of factor VIII are present in the advanced liver disease.
The contribution of FVL, and antiphospho-lipid antibodies to the pathogenesis of PVT in cirrhosis remains controversial. MTHFRTT677 mutation in the absence of hyperhomocysteinemia is not considered a risk factor of venous thromboembolism [43,51-54]. Likewise, the role of inherited natural anticoagulant deficiency (antithrombin, protein C and protein S) in PVT of patients with liver cirrhosis is difficult to establish [55]. In fact, in these patients synthetic dysfunction of the liver leads to a significant reduction of these proteins and an inherited deficiency could be suspected only in the presence of positive familial studies.
In rare cases of PVT associated with recurrent venous thrombosis, or severe presentation with intestinal infarction an underlying myeloproliferative disorder can be suspected [56].
Is it worthwhile performing a complete thrombophilic work-up in the presence of PVT in a cirrhotic patient?
The identification of one or more thrombophilic risk factors in a single patient is interesting for research purposes and it useful in the clinical setting to plan the length of anticoagulant therapy. In fact in patients with “strong” and persistent risk factors anticoagulation has to be prescribed lifelong. In the subgroups of patients with cirrhosis and PVT in which anticoagulation is indicated (see below) the presence of thrombophilia justifies a protracted therapy.
Clinical
Presentation
From a patho-physiologic standpoint, PVT aggravates portal hypertension with increasing blood flow through collateral veins, which in turn favours bleeding from the esophageal and gastric veins. Even if thrombosis mostly occurs in the main portal trunk it may extend to its intrahepatic branches, splenic vein and into the superior mesenteric vein, leading to mesenteric ischemia or infarction, often lethal in these patients [10,57]. In normal subjects the reduction of portal flow induced by PVT is compensated by the increase of hepatic arterial flow (hepatic arterial buffer response) preventing the hypoxic damage. In advanced liver cirrhosis the occurrence of thrombosis is not adequately counterbalanced by arterial buffering [58].
Moreover, thrombosis of the smaller branches of hepatic and portal veins, frequently found in autopsy samples of cirrhotic livers, may induce hepatocyte apoptosis, contributing to the further deterioration of liver disease [16].
Whereas theoretically the occurrence of PVT may worsen either liver function or portal hypertension [59-60] the outcome of the cirrhotic patients with PVT and the actual impact of the thrombosis on the natural history of the cirrhosis have not been investigated to date.
In clinical practice the influence of PVT has been evaluated only in the setting of liver transplantation where, even if PVT is not considered an absolute contraindication, it represents a complex challenge for the hepatic surgeon and is the cause of increased post-transplantation morbidity and mortality [11-15].
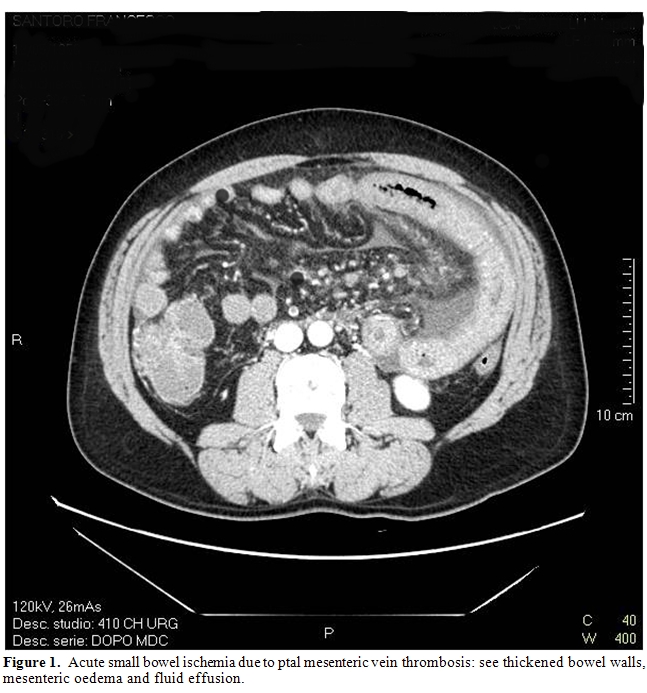
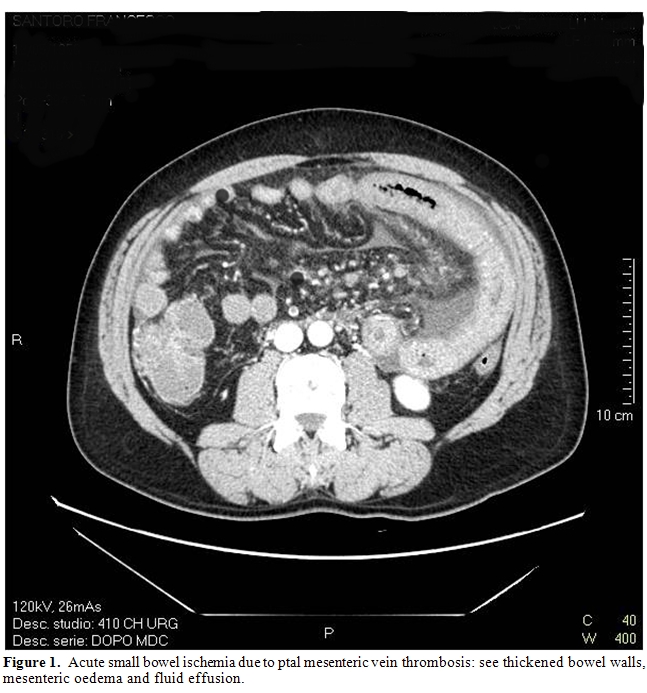
PVT can have a variable clinical onset. In a study of 79 cirrhotic patients, PVT caused gastrointestinal bleeding in 39% and abdominal pain in 18%; seventy per cent of patients, admitted
for acute abdominal pain, presented intestinal infarction due to the involvement of mesenteric vein (Figure 1).
From a patho-physiologic standpoint, PVT aggravates portal hypertension with increasing blood flow through collateral veins, which in turn favours bleeding from the esophageal and gastric veins. Even if thrombosis mostly occurs in the main portal trunk it may extend to its intrahepatic branches, splenic vein and into the superior mesenteric vein, leading to mesenteric ischemia or infarction, often lethal in these patients [10,57]. In normal subjects the reduction of portal flow induced by PVT is compensated by the increase of hepatic arterial flow (hepatic arterial buffer response) preventing the hypoxic damage. In advanced liver cirrhosis the occurrence of thrombosis is not adequately counterbalanced by arterial buffering [58].
Moreover, thrombosis of the smaller branches of hepatic and portal veins, frequently found in autopsy samples of cirrhotic livers, may induce hepatocyte apoptosis, contributing to the further deterioration of liver disease [16].
Whereas theoretically the occurrence of PVT may worsen either liver function or portal hypertension [59-60] the outcome of the cirrhotic patients with PVT and the actual impact of the thrombosis on the natural history of the cirrhosis have not been investigated to date.
In clinical practice the influence of PVT has been evaluated only in the setting of liver transplantation where, even if PVT is not considered an absolute contraindication, it represents a complex challenge for the hepatic surgeon and is the cause of increased post-transplantation morbidity and mortality [11-15].
PVT can have a variable clinical onset. In a study of 79 cirrhotic patients, PVT caused gastrointestinal bleeding in 39% and abdominal pain in 18%; seventy per cent of patients, admitted
for acute abdominal pain, presented intestinal infarction due to the involvement of mesenteric vein (Figure 1).
In 43% of cases PVT was a
fortuitous finding during the scheduled
ultrasound examination for the screening of hepatocellular carcinoma [10].
In the cirrhotic patients it may be difficult to establish the “age” of
thrombosis since the criteria commonly used in non-cirrhotics to define
acute or chronic PVT (presence of collateral circulation, presence of
signs of portal hyper-tension) are already features of the liver
disease.
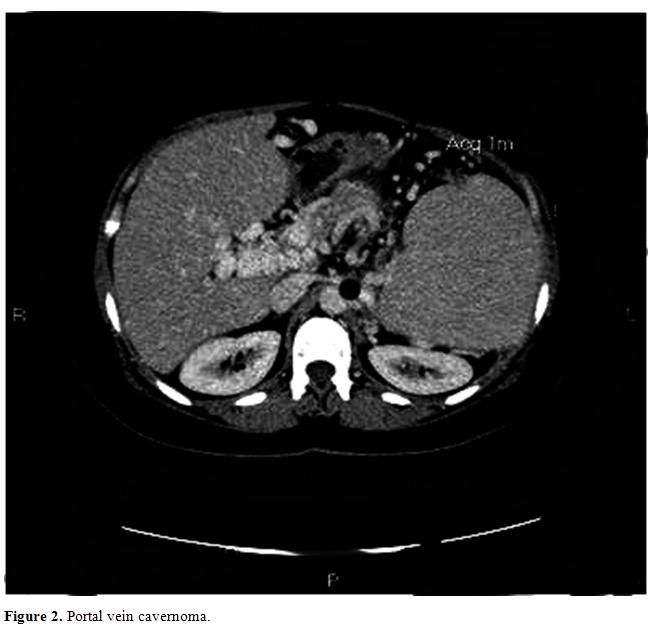
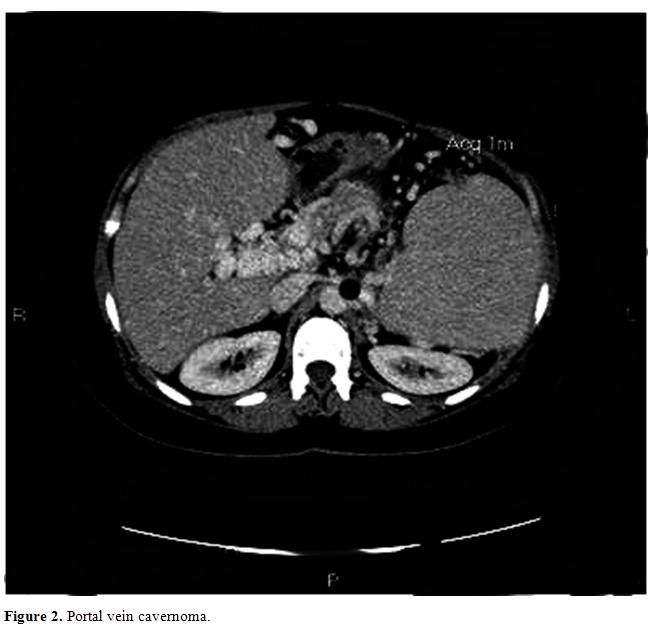
In the previous study [10] PVT developed in the portal trunk in 56% of cases and concomitant involvement of mesenteric or splenic veins occurred in 29%. Isolate thrombosis of intrahepatic portal branches or of splenic and mesenteric veins were present in less than 15% of cases. At the diagnosis, rarely is the thrombus occlusive and the features of portal cavernoma are less frequent compared to those of non-cirrhotic patients, 21% vs 50% respectively [10,61] (Figure 2).
In the previous study [10] PVT developed in the portal trunk in 56% of cases and concomitant involvement of mesenteric or splenic veins occurred in 29%. Isolate thrombosis of intrahepatic portal branches or of splenic and mesenteric veins were present in less than 15% of cases. At the diagnosis, rarely is the thrombus occlusive and the features of portal cavernoma are less frequent compared to those of non-cirrhotic patients, 21% vs 50% respectively [10,61] (Figure 2).
This is probably due to the
earlier diagnosis of PVT and the less pronounced thrombophilic state in
patients with cirrhosis.
Nonetheless, the complete occlusion of the mesenteric vein is invariably associated with intestinal ischemia or infarction and the presence of a splanchnic vein thrombosis has to be investigated in cirrhotic patients with acute abdominal pain.
PVT is usually diagnosed by abdominal ultrasound with pulsed and color Doppler examination but this procedure has sensitivity and specificity in detecting the thrombus variable from 66% to 100%, because it is affected both by operator expertise and patient characteristics [62-63]. Definitive diagnosis of PVT can be obtained by MRI and CT scan; the first provides a better evaluation of the extent of the thrombosis particularly in the mesenteric vein, reaching a sensitivity and specificity of 98% - 100% [64]. CT scan gives information not only of the extent of the thrombosis and the development of collateral circulation but also of the state of the abdominal organs and it is the procedure of choice when intestinal ischemia or hepatocellular carcinoma are suspected [65-66]. In recent studies contrast-enhanced ultrasound67 and PET CT proved useful in discriminating between benign or malignant thrombosis [68].
Overall in the presence of new diagnosis of PVT, the extent of the thrombosis and the clinical features of the patient have to be investigated for a correct evaluation of the prognosis and of the treatment.
Nonetheless, the complete occlusion of the mesenteric vein is invariably associated with intestinal ischemia or infarction and the presence of a splanchnic vein thrombosis has to be investigated in cirrhotic patients with acute abdominal pain.
PVT is usually diagnosed by abdominal ultrasound with pulsed and color Doppler examination but this procedure has sensitivity and specificity in detecting the thrombus variable from 66% to 100%, because it is affected both by operator expertise and patient characteristics [62-63]. Definitive diagnosis of PVT can be obtained by MRI and CT scan; the first provides a better evaluation of the extent of the thrombosis particularly in the mesenteric vein, reaching a sensitivity and specificity of 98% - 100% [64]. CT scan gives information not only of the extent of the thrombosis and the development of collateral circulation but also of the state of the abdominal organs and it is the procedure of choice when intestinal ischemia or hepatocellular carcinoma are suspected [65-66]. In recent studies contrast-enhanced ultrasound67 and PET CT proved useful in discriminating between benign or malignant thrombosis [68].
Overall in the presence of new diagnosis of PVT, the extent of the thrombosis and the clinical features of the patient have to be investigated for a correct evaluation of the prognosis and of the treatment.
Treatment
Studies in numerous series of patients with non-cirrhotic PVT have demonstrated that anticoagulation is safe and effective and represents the therapy of choice [61,69-72].
Despite the high frequency of PVT in patients with liver cirrhosis, there are very few data on the treatment in this setting [73-76] nor have the recent guidelines on vascular liver disorders addressed this specific issue [6,77].
The main concerns for anticoagulation in cirrhotics arise from the presence of a bleeding risk in these patients and the lack of evidence of a real clinical benefit from the therapy in patients with an advanced liver disease.
In stable conditions the bleeding risk arises mainly from the presence of portal hypertension, in fact more than 50% of these patients have gastroesophageal varices [78] and anticoagulation therapy might worsen the severity and duration of bleeding episodes.
The utility of the PVT treatment has been assessed only in patients awaiting liver transplantation in whom the presence of a partial PVT represents a cause of increased morbidity and mortality, while a complete thrombosis is a definitive contraindication to transplantation.
In a preliminary study Francoz et al.[11] demonstrated that anticoagulation therapy achieved a partial or complete portal recanalisation in 42% of 19 patients awaiting liver transplantation. In these patients the survival rate was 79% after OLT, similar to patients without PVT and significantly better than patients with complete portal vein occlusion (50%).
These data, even if necessitating confirmation in larger series of patients, indicated that PVT arising in patients listed for liver transplantation is an indication for anticoagulation therapy.
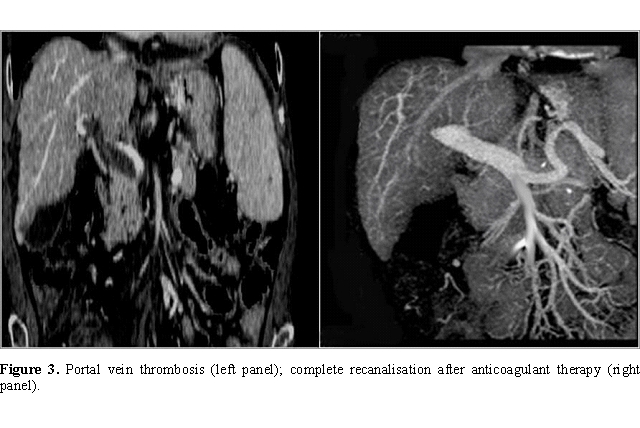
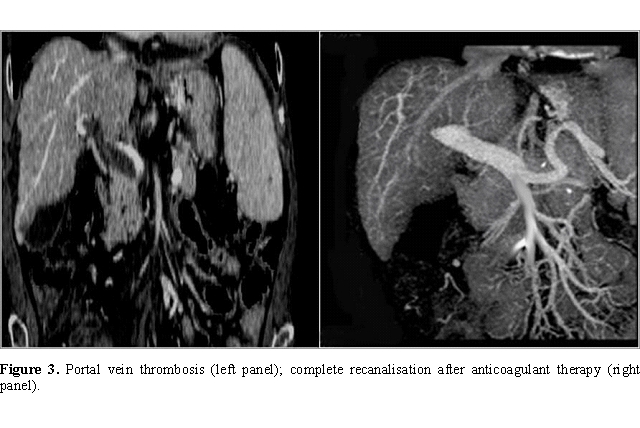
Since data available are not sufficient to make recommendation on PVT treatment, the following suggestions should be considered advice that can help in clinical practice. The choice of the best management should be evaluated case by case, at least to date (Figure 3).
Studies in numerous series of patients with non-cirrhotic PVT have demonstrated that anticoagulation is safe and effective and represents the therapy of choice [61,69-72].
Despite the high frequency of PVT in patients with liver cirrhosis, there are very few data on the treatment in this setting [73-76] nor have the recent guidelines on vascular liver disorders addressed this specific issue [6,77].
The main concerns for anticoagulation in cirrhotics arise from the presence of a bleeding risk in these patients and the lack of evidence of a real clinical benefit from the therapy in patients with an advanced liver disease.
In stable conditions the bleeding risk arises mainly from the presence of portal hypertension, in fact more than 50% of these patients have gastroesophageal varices [78] and anticoagulation therapy might worsen the severity and duration of bleeding episodes.
The utility of the PVT treatment has been assessed only in patients awaiting liver transplantation in whom the presence of a partial PVT represents a cause of increased morbidity and mortality, while a complete thrombosis is a definitive contraindication to transplantation.
In a preliminary study Francoz et al.[11] demonstrated that anticoagulation therapy achieved a partial or complete portal recanalisation in 42% of 19 patients awaiting liver transplantation. In these patients the survival rate was 79% after OLT, similar to patients without PVT and significantly better than patients with complete portal vein occlusion (50%).
These data, even if necessitating confirmation in larger series of patients, indicated that PVT arising in patients listed for liver transplantation is an indication for anticoagulation therapy.
Since data available are not sufficient to make recommendation on PVT treatment, the following suggestions should be considered advice that can help in clinical practice. The choice of the best management should be evaluated case by case, at least to date (Figure 3).
Is PVT treatment
indicated outside the setting of the patients awaiting liver
transplantation?
The presence of acute abdominal pain, due to intestinal ischemia for progression of thrombosis to the mesenteric vein, represents an absolute indication to anticoagulation in the attempt to prevent intestinal infarction. However, there remains to be evaluated whether the presence of mesenteric vein involvement in asymptomatic patients is an indication for treatment. Considering the likelihood of progression of the thrombotic process and the life threatening consequences of the complete mesenteric vein occlusion, treatment is advisable.
It is useful, for clinical purpose, to identify other specific groups of patients in whom PVT treatment needs to be evaluated:
- asymptomatic patients with a compensated liver disease
This group of patients should be treated according to the criteria of non-cirrhotic PVT either to prevent long term complications of the thrombosis or not to preclude a future liver transplantation option. Moreover, a complete assessment of risk factors is suggested in these patients since a thrombophilic state other than cirrhosis per se is likely.
- patients presented with bleeding from portal hypertension
The clinical onset with gastroesophageal bleeding of PVT should not be considered a contraindication to an anticoagulant therapy since the thrombosis may have triggered the bleeding by worsening portal hypertension. Preliminary data show that in these patients anticoagulation therapy is safe if they are adequately treated for bleeding recurrence by medical and endoscopic prophylaxis [79]. The delay in the treatment of PVT till esophageal eradication (median time 4 months) does not hamper the efficacy of the treatment.
In these patients an intrahepatic shunt (TIPS) could be considered as second line treatment because it can achieve the repermeation of the vessel and concomitant treatment of portal hypertensive complications when endoscopic therapies have failed [80].
Lastly, the treatment of PVT is not to be recommended in patients with advanced liver disease, unsuitable for liver transplantation, since the improvement of survival is unlikely in this setting. Nor it is recommended in the presence of a well established cavernomatous transformation of portal vein in the absence of well defined risk factors.
The presence of acute abdominal pain, due to intestinal ischemia for progression of thrombosis to the mesenteric vein, represents an absolute indication to anticoagulation in the attempt to prevent intestinal infarction. However, there remains to be evaluated whether the presence of mesenteric vein involvement in asymptomatic patients is an indication for treatment. Considering the likelihood of progression of the thrombotic process and the life threatening consequences of the complete mesenteric vein occlusion, treatment is advisable.
It is useful, for clinical purpose, to identify other specific groups of patients in whom PVT treatment needs to be evaluated:
- asymptomatic patients with a compensated liver disease
This group of patients should be treated according to the criteria of non-cirrhotic PVT either to prevent long term complications of the thrombosis or not to preclude a future liver transplantation option. Moreover, a complete assessment of risk factors is suggested in these patients since a thrombophilic state other than cirrhosis per se is likely.
- patients presented with bleeding from portal hypertension
The clinical onset with gastroesophageal bleeding of PVT should not be considered a contraindication to an anticoagulant therapy since the thrombosis may have triggered the bleeding by worsening portal hypertension. Preliminary data show that in these patients anticoagulation therapy is safe if they are adequately treated for bleeding recurrence by medical and endoscopic prophylaxis [79]. The delay in the treatment of PVT till esophageal eradication (median time 4 months) does not hamper the efficacy of the treatment.
In these patients an intrahepatic shunt (TIPS) could be considered as second line treatment because it can achieve the repermeation of the vessel and concomitant treatment of portal hypertensive complications when endoscopic therapies have failed [80].
Lastly, the treatment of PVT is not to be recommended in patients with advanced liver disease, unsuitable for liver transplantation, since the improvement of survival is unlikely in this setting. Nor it is recommended in the presence of a well established cavernomatous transformation of portal vein in the absence of well defined risk factors.
Which is the most
adequate bleeding prophylaxis in patients with medium-high risk varices
candidates to anticoagulation therapy?
Studies addressing the issue in patients with PVTare lacking and it is currently advisable to apply to this group of patients the guidelines for the primary prophylaxis of bleeding followed for patients without PVT3 with certain warnings. Medical prophylaxis with non selective beta-blockers is effective in only a portion of patients and has also the disadvantage of further reducing the portal flow [81]. Endoscopic treatment especially sclerotherapy is demonstrated effective as primary prophylaxis of variceal bleeding even if this procedure may be a risk factor for PVT and may induce bleeding complications.
As in non-cirrhotic PVT, anticoagulation therapy is the first line therapeutic strategy in patients with liver cirrhosis. Two main groups of drugs are available to this purpose Vitamin K antagonists (VKA), acenocoumarol and warfarin, and heparins.
Francoz et al. [11] administered five-day-therapy with low molecular weight heparin (nandroparin 5700 UI/day subcutaneously) followed by acenocoumarol at adjusted doses to achieve an INR value of 2.0 – 3.0 to 19 patients with PVT awaiting liver transplantation. Eight of them (42.1%) obtained recanalisation of portal vein and only one patient had upper gastrointestinal bleeding from post ligation ulceration.
Amitrano et al.79 treated 28 cirrhotic PVT patients with enoxaparin 200/UI/Kg /day subcutaneously obtaining a complete recanalisation of portal vein after six months in 33.3%, a partial recanalisation in 50% and no response in 16.7% of patients. Further 12 patients who continued anticoagulation obtained complete recanalisation at a median time of 11 months (range 7-17 months), thus a complete response was achieved in 75% of patients. It is worth noting that half of the patients had presented variceal bleeding and had been submitted to variceal endoscopic eradication by band ligation before starting anticoagulation (Figure 3).
The number of platelets did not change significantly in any patient during anticoagulation treatment and only two patients complained of mild anemia due to portal hypertensive gastropathy.
Studies addressing the issue in patients with PVTare lacking and it is currently advisable to apply to this group of patients the guidelines for the primary prophylaxis of bleeding followed for patients without PVT3 with certain warnings. Medical prophylaxis with non selective beta-blockers is effective in only a portion of patients and has also the disadvantage of further reducing the portal flow [81]. Endoscopic treatment especially sclerotherapy is demonstrated effective as primary prophylaxis of variceal bleeding even if this procedure may be a risk factor for PVT and may induce bleeding complications.
As in non-cirrhotic PVT, anticoagulation therapy is the first line therapeutic strategy in patients with liver cirrhosis. Two main groups of drugs are available to this purpose Vitamin K antagonists (VKA), acenocoumarol and warfarin, and heparins.
Francoz et al. [11] administered five-day-therapy with low molecular weight heparin (nandroparin 5700 UI/day subcutaneously) followed by acenocoumarol at adjusted doses to achieve an INR value of 2.0 – 3.0 to 19 patients with PVT awaiting liver transplantation. Eight of them (42.1%) obtained recanalisation of portal vein and only one patient had upper gastrointestinal bleeding from post ligation ulceration.
Amitrano et al.79 treated 28 cirrhotic PVT patients with enoxaparin 200/UI/Kg /day subcutaneously obtaining a complete recanalisation of portal vein after six months in 33.3%, a partial recanalisation in 50% and no response in 16.7% of patients. Further 12 patients who continued anticoagulation obtained complete recanalisation at a median time of 11 months (range 7-17 months), thus a complete response was achieved in 75% of patients. It is worth noting that half of the patients had presented variceal bleeding and had been submitted to variceal endoscopic eradication by band ligation before starting anticoagulation (Figure 3).
The number of platelets did not change significantly in any patient during anticoagulation treatment and only two patients complained of mild anemia due to portal hypertensive gastropathy.
Which is the best
anticoagulant therapy?
In absence of comparative studies, the choice of the anticoagulant therapy has to rely on the following considerations:
-VKAs administered by mouth are more acceptable by the patients but they need periodical dose-adjustments by INR monitoring; in patients with advanced liver disease the INR value is often spontaneously close to or above 2.0 considered a therapeutic range for anticoagulation. Thus INR value as currently measured is inadequate to monitor anticoagulation for patients with severe liver disease [21,82], yet other methods are foreseen [21,83].The long duration of anticoagulant effect due to the long half life of VKAs could represent a further clinical disadvantage in the case of bleeding episode.
- LMWHs have completely replaced unfractionated heparins since they have the same efficacy and do not necessitate monitoring for dose adjustment [84]. Furthermore the fearful heparin induced thrombocytopenia is less common with LMWH and this may be useful in cirrhotic patients with low platelet count.
These disadvantages of both anticoagulation strategies may be overcome by the new oral anticoagulant drugs such as thrombin inhibitors and anti factor Xa [85].
Currently VKAs may represent a therapeutic option in patients with compensated liver disease who require long term anticoagulation. LMWHs should be given to patients awaiting liver
transplantation and to patients with a more severe liver disease.
In absence of comparative studies, the choice of the anticoagulant therapy has to rely on the following considerations:
-VKAs administered by mouth are more acceptable by the patients but they need periodical dose-adjustments by INR monitoring; in patients with advanced liver disease the INR value is often spontaneously close to or above 2.0 considered a therapeutic range for anticoagulation. Thus INR value as currently measured is inadequate to monitor anticoagulation for patients with severe liver disease [21,82], yet other methods are foreseen [21,83].The long duration of anticoagulant effect due to the long half life of VKAs could represent a further clinical disadvantage in the case of bleeding episode.
- LMWHs have completely replaced unfractionated heparins since they have the same efficacy and do not necessitate monitoring for dose adjustment [84]. Furthermore the fearful heparin induced thrombocytopenia is less common with LMWH and this may be useful in cirrhotic patients with low platelet count.
These disadvantages of both anticoagulation strategies may be overcome by the new oral anticoagulant drugs such as thrombin inhibitors and anti factor Xa [85].
Currently VKAs may represent a therapeutic option in patients with compensated liver disease who require long term anticoagulation. LMWHs should be given to patients awaiting liver
transplantation and to patients with a more severe liver disease.
Which is the duration of anticoagulation?
The current guidelines for the treatment of venous thromboembolism [86] can be applied to cirrhotic PVT. After an initial 3-6 month period of anticoagulant therapy patients should be separated into the following groups:
- patients who achieved a complete recanalisation can stop anticoagulant therapy in the absence of previous thrombotic events, or thrombopilic risk factors. They should be followed periodically for PVT recurrence.
- patients with partial recanalisation or with a stable partial thrombosis should continue anticoagulant therapy if candidates for or suitable for future OLT in order to prevent a complete portal vein occlusion.
- patients who failed to achieve any recanalisation of occlusive PVT should stop anticoagulant therapy. Nevertheless, in patients with deep vein thrombosis of the limbs, residual or persistent thrombosis is considered as a risk factor for recurrence requiring long-life anticoagulation [87-88]. If this applies to the patients with cirrhotic PVT needs to be evaluated in future follow-up studies.
- patients with recurrence of PVT should be considered for long-life anticoagulant therapy.
So this therapeutic approach in a cirrhotic patient with PVT should be reserved only in the case of patients with ongoing intestinal infarction not responsive to anticoagulation therapy.
Transjugular intrahepatic porto systemic shunt (TIPS) can be considered a second line treatment of PVT in patients with portal hypertensive complications not controlled by the common therapeutic approach particularly in patients awaiting liver transplantation. In preliminary experience Senzolo et al. reported a successful TIPS placement in a 69% of 13 cirrhotic patients with PVT [80]. This procedure is technically feasible also in patient with cavernomatous transformation of portal vein [91-93] unless intrahepatic portal branches are patent.
Perspectives:
Portal
vein thrombosis is recognized as one of the complications of liver
cirrhosis but many aspects still remain to be elucidated. The first is
the impact of PVT on the natural history of liver cirrhosis and
prospective studies addressing this issue are warranted and to identify
subgroups of patients who could benefit from PVT treatment.
The best treatment option in terms of efficacy and safety has also to be established. Furthermore, which anticoagulant treatment, the duration of therapy and the modality of monitoring need to be evaluated in future controlled trials.
The best treatment option in terms of efficacy and safety has also to be established. Furthermore, which anticoagulant treatment, the duration of therapy and the modality of monitoring need to be evaluated in future controlled trials.
References
- Ogren M, Bergquist D, Bjorck M, Acosta
S, Eriksson H, Sternby NH. Portal vein thrombosis: prevalence, patient
characteristics and lifetime risk: a population study based on 23,796
consecutive autopsies. World J Gastroenterol 2006; 12: 2115-2119.

- De Franchis R. Evolving consensus in
portal hypertension. Report of the Baveno IV consensus workshop on
methodology of diagnosis and therapy in portal hypertension. J Hepatol
2005; 43: 167-176.

- Sarin SK, Sollano JD, Chawla YK,
Amarapurkar D, Hamid S, Hashizumer M, et al. Consensus on extrahepatic
portal vein obstruction. Liver Int 2006; 26:512-519.

- Janssen HL, Wijnhoud A, Haagsma EB,
van Uum SH, van Nieuwkerk CM, Adang RP, et al. Extrahepatic portal vein
thrombosis: aetiology and determinants of survival. Gut 2001;
49:720-724.

- Garcia-Pagan JC, Hernandez-Guerra M,
Bosch J. Extrahepatic portal vein thrombosis. Semin Liv Dis 2008;
28:282-292.

- DeLeve LD, Valla DC, Garcia-Tsao G.
Vascular disorders of the liver. Hepatology 2009; 49: 1729- 1764.

- Pirisi M, Avellini C, Fabris C. Portal
vein thrombosis in hepatocellular carcinoma: age and sex distribution
in an autopsy study. J Cancer Res Clin Oncol 1998; 124:398-400.

- Okuda K, Ohnishi K, Kimura K,
Matsutani S, Sumida M, Goto N, et al. Incidence of portal vein
thrombosis in liver cirrhosis. An angiographic study in 708 patients.
Gastroenterology 1985; 89:279-286.

- Gaiani S, Bolondi L, Li Bassi S,
Zironi G, Siringo S, Barbara L. Prevalence of spontaneous hepatofugal
portal flow in liver cirrhosis. Clinical and endoscopic correlation in
228 patients. Gastroenterology 1991;100:160-167.

- Amitrano L, Guardascione MA,
Brancaccio V, Margaglione M, Manguso F, Iannaccone L, et al. Risk
factors and clinical presentation of portal vein thrombosis in patients
with liver cirrhosis. J Hepatol 2004; 40: 736-741.

- Francoz C, Belghiti J, Vilgrain V,
Sommacale D, Paradis V, Condat B,et al. Splanchnic vein
thrombosis in candidates for liver transplantation: usefulness of
screening and anticoagulation. Gut 2005; 54:691-697.

- Nonami T, Yokoyama I, Iwatsuki S,
Starzl TE. The incidence of portal vein thrombosis at liver
transplantation. Hepatology 1992; 16:1195-1198.

- Yerdel MA, Gunson B, Mirza D,
Karayalcin K, Olliff S, Buckels J, et al. Portal vein thrombosis in
adults undergoing liver transplantation. Transplantation 2000;
69:1873-1881.

- Charco R, Fuster J, Fondevila C,
Ferrer J, Mans E, Garcia-Valdecasas JC. Portal vein thrombosis in liver
transplantation. Transpl Proc 2005; 37: 3904-3905.

- Manzanet G, Sanjuan F, Orbis P, Lopez
R, Moya A, Juan M, et al. Liver transplantation in patients with portal
vein thrombosis. Liver Transpl 2001; 7:125-131.

- Wanless IR, Wong F, Blendis LM, Greig
P, Heathcote EJ, Levy G. Hepatic and portal vein thrombosis in
cirrhosis: possible role in development of parenchymal extinction and
portal hypertension. Hepatology 1995; 21: 1238-1247.

- Zocco MA, Di Stasio E, De
Cristofaro R, Movi MR, Ainora ME, Ponziani F, et al. Thrombotic risk
factors in patients with liver cirrhosis: correlation with MELD scoring
system and portal vein thrombosis development. J Hepatol. 2009 Oct;51(4):682-9

- Caldwell SH, Hoffman M, Lisman T,
Macik BG, Northrup PG, Reddy KR, et al. Coagulation disorders and
hemostasis in liver disease: pathophysiology and critical assessment of
current management. Hepatology 2006; 44: 1039-1046.

- Mannucci PM. Abnormal hemostasis
tests and bleeding in chronic liver disease: are they related? No. J
Thromb Haemost 2006; 4: 721-723.

- Bosch J, Reverter JC. The coagulopathy of
cirrhosis: Myth or reality? Hepatology 2005; 41: 434-435.

- Tripodi A, Salerno F, Chantarangkul
V, Clerici M, Cazzaniga M, Primignani M, et al. Evidence of
normal thrombin generation in cirrhosis despite abnormal
conventional coagulation tests. Hepatology 2005; 41: 553-558.

- Northup PG. Hypercoagulation in liver
disease.Clin Liv Dis 2009;109-116.

- Tripodi A, Mannucci PM. Abnormalities
of hemostasis in chronic liver disease: reappraisal of their clinical
significance and need for clinical and laboratory research. J Hepatol
2007; 46;727-733.

- Ben-Ari Z, Osman E, Hutton RA,
Burroughs AK. Disseminated intravascular coagulation in liver
cirrhosis: fact or fiction? Am J Gastroenterol 1999; 94:2977-2982.

- Montalto P, Vlachogiannakos J, Cox
DJ, Pastacaldi S, Patch D, Burroughs AK. Bacterial infection in
cirrhosis impairs coagulation by a heparin effect: a prospective study.
J Hepatol 2002;37:463-470.

- Amitrano L, Brancaccio V,
Guardascione MA, Margaglione M, Iannacone L, D’AndreaG, et al.
Inherited coagulation disorders in cirrhotic patients with portal
vein thrombosis. Hepatology 2000; 31: 345-348.

- Amitrano L, Guardascione MA, Ames
PRJ, Margaglione M, Iannaccone L, Brancaccio V, et al. Increased plasma
prothrombin concentration in cirrhotic patients with portal vein
thrombosis and prothrombin G20210A mutation. Thromb Haemost 2006; 95;
221-223.

- Northup PG, McMahon MM, Parker Ruhl
A, Altschuler SE, Volk-Bednarz A, Caldwell SH, et al.
Coagulopathy does not fully protect hospitalized cirrhosis patients
from peripheral venous thromboembolism. Am J Gastroenterol 2006; 101:
1524-1528.

- Gulley D, Teal E, Suvannasankha A,
Chalasani N, Liangpunsakul S. Deep vein thrombosis and pulmonary
embolism in cirrhosis patients. Dig Dis Sci 2008;53:3012-3017.

- Garcia-Fuster MJ, Abdilla N, Fabia
MJ, Fernandez C, Oliver V, Forner MJ. Venous thromboembolism and liver
cirrhosis. Rev Esp Enferm Dig 2008;100:259-262.

- Sogaard KK, Horvath-Puho E, Gronbaek
H, Jepsen P, Volstrup H, Sorensen HT. Risk of venous thromboembolism in
patients with liver disease: a nationwide population-based case-control
study. Am J Gastroenterol 2009; 104:96-101.

- Ogren M, Bergqvist D, Bjorck M,
Acosta S, Sternby NH. High incidence of concomitant venous
thromboembolism in patients with portal vein thrombosis: a population
study based on 23,796 consecutive autopsies. J Thromb Haemost 2007;
5:198-200.

- Lopez JA, Kearon C, Lee AYY. Deep venous thrombosis. Am Soc Hematol Educ Program 2004; 439-456.
- Rosendaal FR. Venous thrombosis: a
multicausal disease. Lancet 1999; 353: 1167-1173.

- Denninger MH, Chait Y, Casadevall N,
Hillaire S, Guillin MC, Bezeaud A, et al. Cause of portal vein
thrombosis in adults: the role of multiple concurrent factors.
Hepatology 2000; 32: 587-591.

- Primignani M, Martinelli I,
Bucciarelli P, Battaglioli T, Reati R, Fabris F, et al. Risk factors
for thrombophilia in extrahepatic portal vein obstruction. Hepatology
2005; 41: 603-608.

- Amitrano L, Brancaccio V,
Guardascione MA, Margaglione M, Sacco M, Martino R, et al. Portal vein
thrombosis after variceal endoscopic sclerotherapy in cirrhotic
patients: role of genetic thrombophilia. Endoscopy 2002; 34: 535-538.

- Virchow RLK (translated by: Matzdorff, et al.). Thrombose und Embolie. Canton, MA: Science History Publications; 1998.
- Closse C, Seigneur M, Renard M,
Pruvost A, Dumain P, Belloc F, et al. Influence of hypoxia and
hypoxia-reoxygenation on endothelial P-selectin expression. Thromb Res
1997; 85: 159-164.

- Ikeda M, Sekimoto M, Takiguchi S,
Kubota M, Ikenaga M, Yamamoto H, et al. High incidence of thrombosis of
the portal venous system after laparoscopic splenectomy: a prospective
study with contrast-enhanced CT scan. Ann Surg 2005; 241:208-216.

- Baijal SS, Mohan S, Singh JR, Verma
A. Thrombosed mesocaval shunt: salvage by mechanical thrombolysis. Case
report e review of the literature. Cardiovasc Intervent Radiol 2008; 31
(suppl 2): S161-S165.

- Mangia A, Villani MR, Cappucci G,
Santoro R, Ricciardi R, Facciorusso D, et al. Causes of portal venous
thrombosis in cirrhotic patients: the role of genetic and acquired
factors. Eur J Gastroenterol Hepatol 2005; 17: 745-751.

- Erkan O, Bozdayi AM, Disibeyaz
S, Oguz D, Ozcan M, Bahar K, et al. Thrombophilic gene mutations
in cirrhotic patients with portal vein thrombosis. Eur J Gastroenterol
Hepatol 2005; 17: 339-343.

- Dentali F, Galli M, Gianni M, Ageno
W. Inherited thrombophilic abnormalities and risk of portal vein
thrombosis: a meta-analysis. Thromb Haemost 2008; 99:675-682.

- Chang CJ, Shiau YT,Chen TL, Hou MC,
Sun CH, Liao WC, et al. Pyogenic portal vein thrombosis as a reservoir
of persistent septicaemia after cyanoacrylate injection for bleeding
gastric varices. Digestion 2008;78:139-143.

- Violi F, Ferro D, Basili S, Lionetti
R, Rossi E, Merli M, et al. Ongoing prothrombotic state in
the portal circulation of cirrhotic patients. Thromb Haemost
1997;77:44-47.

- Habu D, Nishiguchi S, Shiomi S,
Tamori A, Sakaguchi H, Takeda T, et al. Portal vein thrombosis
following percutaneous ethanol injection therapy for
hepatocellular carcinoma. Indian J Gastroenterol 2002 ; 21:162-163.

- Lencioni R, Caramella D, Sanguinetti
F, Battolla L, Falaschi F, Bartolozzi C. Portal vein thrombosis after
percutaneous ethanol injection for hepatocellular carcinoma: value of
color Doppler sonography in distinguishing chemical and tumor
thrombi. Am J Roentgenol. 1995 ;164:1125-1130.

- Francica G, Marone G, Solbiati L,
D'Angelo V, Siani A. Hemobilia, intrahepatic hematoma and acute
thrombosis with cavernomatous transformation of the portal vein after
percutaneous thermoablation of a liver metastasis. Eur Radiol
2000;10:926-929.

- Martinelli I, Primignani M, Aghemo A,
Reati R, Bucciarelli P, Fabris F, et al. High levels of factor VIII and
risk of extra-hepatic portal vein obstruction. J Hepatol 2009;50:916-922

- Bosy-Westphal A, Petersen S,
Hinrichsen H, Czech N, J Muller M. Increased plasma homocysteine in
liver cirrhosis. Hepatol Res 2001; 20: 28-38.

- Mangia A, Margaglione M, Cascavilla
I, Gentile R, Cappucci G, Facciorusso D, et al. Anticardiolipin
antibodies in patients with liver disease. Am J Gastroenterol
1999; 94: 2983-2987.

- Romero Gomez M, Suarez Garcia E,
Lopez Lacomba D, Marchante I, Grande L, Castro Fernandez M.
Antiphospholipid antibodies are related to portal vein thrombosis in
patients with liver cirrhosis. J Clin Gastroenterol 2000; 31: 237-240.

- Bezemer ID, Doggen CJM,
Vos HL, Rosendaal FR. No Association Between the Common MTHFR 677C T
Polymorphism and Venous Thrombosis. Results From the MEGA Study. Arch
Intern Med 2007;167:497-501 .

- Fischer NC, Wilde JT, Roper J, Elias.
Deficiency of natural anticoagulant proteins C,S, and antithrombin in
portal vein thrombosis: a secondary phenomenon? Gut 2000; 46: 534-539.

- Colaizzo D, Amitrano L, Guardascione
MA, Balzano A, Margaglione M. Janus kinase-2 mutation, cirrhosis
and splanchnic vein thrombosis. Eur J Gastroenterol Hepatol. 2008;
20:245-246.

- Amitrano L, Guardascione MA,
Brancaccio V, Iannaccone L, Ames PRJ, Balzano A. Portal and mesenteric
venous thrombosis in cirrhotic patients. Gastroenterology 2002;123:
1409-1410.

- Sacerdoti D, Merkel C, Bolognesi M,
Amodio P, Angeli P, Gatta A. Hepatic arterial resistance in
cirrhosis with and without portal vein thrombosis: relationships with
portal hemodynamics. Gastroenterology 1995; 108: 1152-1158.

- Romero-Gomez M, Gutierrez-Tous R,
Delgado-Mije D. Anticoagulant therapy for recent portal vein thrombosis
in a patient with liver cirrhosis suffering from variceal rebleeding.
Gastroenterology 2002; 122: 2095.

- D’Amico G, de Franchis R. Upper
digestive bleeding in cirrhosis. Post-therapeutic outcome and
prognostic indicators. Hepatology 2003;38;599-612.

- Amitrano L, Guardascione MA,
Scaglione M, Pezzullo L, Sangiuliano N, Armellino MF, et al. Prognostic
factors in non-cirrhotic patients with splanchnic vein thrombosis. Am J
Gastroenterol 2007;102:2464-2470.

- Tessler FN, Gehring AS, Gomes AS,
Perrella RR, Ragavendra N, Busuttil RW, et al. Diagnosis of portal vein
thrombosis: value of color Doppler imaging. AIR Am J Roentgenol. 1991;
157; 765-766.

- Rossi S, Rosa L, Ravetta V, Cascina
A, Quaretti P, Azzaretti A, et al. Contrast-enhanced versus
conventional and color Doppler sonography for the detection of
thrombosis of the portal and hepatic venous systems. AJR Am J
Roentgenol 2006;186:763-773.

- Shah TU, Semelka RC, Voultsinos V,
Elias J Jr, Altun E, Pamuklar E, et al. Accuracy of magnetic resonance
imaging for preoperative detection of portal vein thrombosis in liver
transplant candidates. Liver Transpl 2006;12:1682-1688.

- Tublin ME, Dodd GD 3rd, Baron RL.
Benign and malignant portal vein thrombosis: differentiation by CT
characteristics. AJR Am Roentgenol 1997; 168:719-723.

- Lee HK, Park SJ, YI BH, Yeon EK, Kim
JH, Hong HS. Portal vein thrombosis: CT features. Abdom Imaging
2008;33:72-79.

- Song ZZ, Huang M, Jiang TA, Zhao QY,
Yao L, Mou Y, et al. Diagnosis of portal vein thrombosis discontinued
with liver tumors in patients with liver cirrhosis and tumors by
contrast-enhanced US: a pilot study. Eur J Radiol 2009;
doi:10.1016/j.ejrad.2009.04.021

- Sun L, Guan YS, Pan WM, Chen GB, Luo
ZM, Wai JH et al. Highly metabolic thrombus of the portal vein:
18F fluorodeoxyglucose positron emission tomo-graphy/computer
tomography demonstration and clinical significance in hepatocellular
carcinoma. World J Gastroenterol. 2008;14:1212-1217.

- Condat B, Pessione F, Hillaire S,
Denninger MH, Guillin MC, Poliquin M, et al. Current outcome of portal
vein thrombosis in adults: risk and benefit of anticoagulant therapy.
Gastroenterology 2001;120:490-497.

- Condat B, Pessione F, Denninger MH,
Hillaire S, Valla D. Recent portal and mesenteric venous thrombosis:
Increased recognition and frequent recanalization on anticoagulant
therapy. Hepatology 2000;32:466-470.

- Plessier A, Murad SD, Hernandez-Guerra M, Consigny Y, Fabris F, Heller J, et al. A prospective multicentric follow-up study on 105 patients with acute portal vein thrombosis(PVT) : results from the European network for vascular disorders of the liver (EN-VIE). Hepatology 2007;46(suppl 1):310A.
- Turnes J, Garcia-Pagan JC, Gonzalez
M, Aracil C,Calleja JL, Ripoll C, et al. Portal hypertension-related
complications after acute portal vein thrombosis: impact of early
anticoagulation. Clin Gastroenterol Hepatol 2008;6:1412-1417.

- Garcia-Pagan JC, Valla DC.
Portal vein thrombosis: a predictable milestone in cirrhosis? J Hepatol
2009; doi:10.1016/j.jhep.2009.06.009.

- Fimognari FL, Violi F. Portal vein
thrombosis in liver cirrhosis. Intern Emerg Med 2008;3:213-218

- Ageno W, Galli M, Squizzato A. Is
there a role for timely diagnosis and early anticoagulant treatment of
portal vein thrombosis in patients with liver cirrhosis? Intern Emerg
Med 2008;3:195-196.

- Senzolo M, Ferronato C, Burra P,
Sartori MT. Anticoagultion for portal vein thrombosis in cirrhotic
patients should be always considered. Intern Emerg Med 2009:4: 161-162.

- Valla DC. Thrombosis and anticoagulation
in liver disease. Hepatology 2008;47:1384-1393.

- Prediction of the first variceal
hemorrhage in patients with cirrhosis of the liver and esophageal
varices. A prospective multicenter study. The North Italian Endoscopic
Club for the Study and Treatment of Esophageal Varices. N Engl J Med
1988;319:983-989.

- Amitrano L, Guardascione MA, Menchise
A, Martino R, Scaglione M, Giovine S, et al. Safety and Efficacy of
Anticoagulation Therapy With Low Molecular Weight Heparin for Portal
Vein Thrombosis in Patients With Liver Cirrhosis. J Clin Gastroenterol
2009: doi: 10.1097/MCG.0b013e3181b3ab44.

- Senzolo M, Tibbals J, Cholongitas E,
Triantos CK, Burroughs AK, Patch D. Transjugular intrahepatic
portosystemic shunt for portal vein thrombosis with and without
cavernous transformation. Aliment Pharmacol Ther 2006;15:767-775.

- Bosch J, Mastai R, Kravetz D, Bruix
J, Gaya J, Rigau J et al. Effects of propranolol on azygos venous blood
flow and hepatic and systemic hemodynamics in cirrhosis. Hepatology
1984;4:1200-1205.

- Deitcher SR. Interpretation of the
international normalised ratio in patients with liver disease. Lancet
2002;359:47-48.

- Mancuso A, Fung K, Cox D, Mela M,
Patch D, Burroughs AK. Assessment of blood coagulation in severe liver
disease using thromboelastography: use of citrate storage versus native
blood. Blood Coagul Fibrinolysis 2003; 14: 211-216.

- Dolovich LR, Ginsberg JS, Douketis
JD, Holbrook AM, Cheah G. A meta-analysis comparing
low-molecular-weight heparins with unfractionated heparin in the
treatment of venous thromboembolism: examining some unanswered
questions regarding location of treatment, product type, and dosing
frequency. Arch Intern Med 2000; 160: 181-188.

- Bauer KA. New anticoagulants: antiIIa vs
antiXa. Is one better? J Thromb Thrombolysis 2006;21:67-72.

- Kearon C, Kahn SR, Agnelli G,
Goldhaber S, Raskob GE, Comerota AJ. American College of Chest
Physicians. Antithrombotic therapy for venous thromboembolic disease:
American College of Chest Physicians Evidence-Based Clinical Practice
Guidelines (8th Edition). Chest 2008;133 (6 suppl):454S-545S .

- Prandoni P, Prins MH, Lensing AW,
Ghirarduzzi A, Ageno W, Imberti D, et al. Residual thrombosis on
ultrasonography to guide the duration of anticoagulation in patients
with deep venous thrombosis: a randomized trial. Ann Intern Med 2000;
150: 577-585.

- Siragusa S, Malato A, Anastasio
R, Cigna V, Milio C, Amato C.Residual vein thrombosis to establish
duration of anticoagulation after a first episode of deep vein
thrombosis: the Duration of Anticoagulation based on Compression
UltraSonography (DACUS) study. Blood 2008;112: 511-515.

- Hollingshead M, Burke CT, Mauro MA,
Weetis SM, Dixon RG, Jaugus PF. Transcatheter thrombolytic therapy for
acute mesenteric and portal vein thrombosis. J Vasc Inter Radiol
2005;16:651-661.

- Smalberg JH, Spaander MV, Jie KS,
Pattynama PM, van Buuren HR, van den Berg B, et al. Risks and benefits
of transcatheter thrombolytic therapy in patients with splanchnic
venous thrombosis. Thromb Haemost. 2008 ; 100: 1084-1088.

- Blum U, Haag K, Rossle M, Ochs A,
Gabelmann A, Boos S et al. Non cavernomatous portal vein thrombosis in
hepatic cirrhosis: treatment with transjugular intrahepatic
portosystemic shunt and local thrombolysis. Radiology
1995;195:153-157.

- Bauer J, Johnson S, Durham J,
Ludkowski M, Trotter J, Bak T et al. The role of TIPS for portal vein
patency in liver transplant patients with portal vein thrombosis. Liver
Transpl 2006;12:1544-1551.

- Van Ha TG, Hodge J, Funaki B, Lorenz
J, Rosenblum J, Straus C, et al. Transjugular intrahepatic
portosystemic shunt placement in patients with cirrhosis and
concomitant portal vein thrombosis. Cardiovasc Intervent Radiol
2006;29: 785-790.
