Review Articles
Nilüfer Yeşilot Barlas, Gülşen
Akman-Demir and Sara Zarko Bahar
Published: October 24, 2011
Received: April 20, 2011
Accepted: October 13, 2011
Mediterr J Hematol Infect Dis 2011, 3(1): e2011044, DOI 10.4084/MJHID.2011.044
This article is available from: http://www.mjhid.org/article/view/8459
Abstract
Cerebral
venous and dural sinus thrombosis (CVT) is a rare condition
with a wide spectrum of clinical presentations. The epidemiology of the
disease
has evolved considerably during the recent decades with increasing oral
contraceptive use in young and
middle-aged women. CVT has various causes including genetic and
acquired
prothrombotic disorders and it usually has a favorable outcome with a
low rate
of thrombotic recurrence and mortality. Geographical and ethnic
variations
between populations may result in different distribution of CVT
etiologies
leading to different pathophysiological mechanisms and clinical
presentations.
In CVT series reported mostly from the
Cerebral
venous and dural sinus thrombosis (CVT) presents with a broad spectrum
of symptoms, and it is caused by a variety of etiologies.[1-2]
Nearly 85% of CVT cases have a prothrombotic risk factor or a direct
causative disorder. These include genetic and acquired prothrombotic
disorders, cancer, hematological diseases, pregnancy and puerperium,
systemic inflammatory diseases, neurosurgical procedures and some local
anatomical causes such as ear, head or neck infections. Around 40% of
CVT patients have more than one risk factor.[3] Among
the systemic inflammatory disorders, systemic lupus erythematotsus
(SLE), antiphospholipid syndrome, sarcoidosis and Behcet’s disease (BD)
can be listed.
CVT affects approximately 5 people per million annually.[4]
Although underlying factors may be common with other types of venous
thromboembolism, the unique way the central nervous system is affected
with CVT gives it an exceptional place under the concept of venous
thrombosis. Even though CVT can develop in the course of various
disorders, due to its clinical presentation most of the patients are
evaluated within stroke cohorts. CVT accounts for 0.5 to 1% of all
strokes.[2,4] In Istanbul Medical School Stroke
Registry CVT comprises 1% of all strokes.[5]
It is hard to estimate the number of CVT cases associated with various
etiological processes that are not included in stroke registries. The
largest information on CVT is provided by International Study on
Cerebral Vein and Dural Sinus Thrombosis (ISCVT) comprised of 624
cases. In that prospective observational study, aimed to determine
prognosis of CVT, 624 symptomatic CVT cases from 21 countries were
registered over 3 years and ample information about all characteristics
of CVT patients were obtained as well. Fifty-seven percent of
these cases are from North-western Mediterranean countries (France,
Portugal, Spain and Italy). Overall 74.5% of patients were women and in
2/3rds of them CVT was associated with pregnancy, puerperium, oral
contraceptives (OC) or hormone replacement therapy (HRT); factors
associated with gender. The second most common etiological factor was
thrombophilia with a rate of 34%. However, these figures do not reflect
the true underlying factor incidence since in more than 40 % of the
cases there was more than one risk factor.
Information on epidemiology and risk factors for cerebral venous
thrombosis (CVT) in North-western Mediterranean countries are largely
available. On the contrary, information on CVT in the South-eastern
Mediterranean region is relatively sparse. The aim of this review is to
focus on CVT and inherited and acquired causes in countries of the
South-eastern Mediterranean region.
Behcet’s disease is one of the systemic inflammatory diseases with high
risk of venous thromboembolism and it is seen more commonly along the
Silk Route that extends from the Mediterranean region to Japan.[6]
In the South-eastern Mediterranean region etiology of CVT differs
compared to Western countries, due to the higher prevalence of Behcet’s
disease in the region. Behcet’s disease is a systemic inflammatory
disorder of unknown etiology, which presents with recurrent oral
aphtae, genital ulcerations, and uveitis. Diagnostic criteria for BD
are listed on Table 1.[7] Central nervous system (CNS) involvement is seen
about in 5-10% of cases with BD.[8-9]
Besides the more commonly encountered parenchymal neurological
involvement which occurs mainly as a brainstem meningoencephalitis,
intracranial hypertension due to CVT may be seen in about 15% of the
patients with neurological involvement. In our series this ratio was
17%, in another series from Tunisia it was 11%.[10-11]
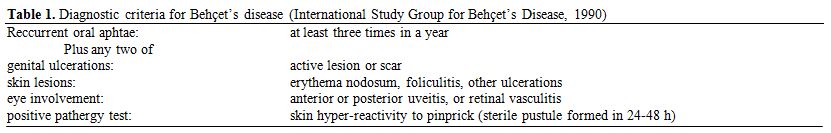
Table 1. Diagnostic criteria for Behçet’s disease (International Study Group for Behçet’s Disease, 1990)
Although population based studies are lacking from South-eastern
Mediterranean countries, a previous study comparing a series of CVT
patients with and without BD revealed that more than half of the
patients diagnosed with CVT have BD as the underlying factor. [12]
When the yearly rate of CVT patients are compared according to etiology
in this cohort 42% of the patients had BD as the causative factor
compared to all other etiologies complied as a separate group as the
underlying conditions for the remaining 58%.[12] One
point deserves further clarification because in this study, non-BD
group consisted largely of patients that were admitted to the hospital
with CVT; however, there may be another group of patients who present
with isolated ICH symptoms or only headache that were either not
diagnosed as CVT or were diagnosed but managed in the emergency room
due to relatively less serious clinical presentation and consequently
were not included in the database.
Behcet’s disease comprises a significant portion of CVT cases from many
Mediterranean countries, although the percentage varies according to
the country, and the center reporting the series. A series from France
analyzing isolated intracranial hypertension as the only sign of CVT
found that these patients consisted as high as 37% of all CVT patients
and 22% of them had BD as the underlying cause; however, this center is
one of the dedicated centers to Behcet’s disease in the country. In
this cohort other common etiological factors were coagulopathies,
unknown etiology, oral contraceptive use and other inflammatory
diseases.[13] On the other hand, data from Europe
depicts the rarity of BD as an etiological factor of CVT, there were
only 6 patients with BD among 624 patients registered in the ISCVT.[3] Interestingly, however, a small CVT series from
Lebanon did not have any patients with BD, among 16 cases.[14]
This might be reflecting a selection bias, as discussed below.
In another CVT series including only patients with cortical or deep
vein thrombosis, excluding patients with dural sinus thrombosis from
Turkey, similar frequencies of etiologies to those reported from the
West with few CVT patients with BD was reported.[15]
Albeit small in size, in this series the distribution of etiological
factors causing CVT among hormonal factors, malignancy, genetic
thrombophilia, infections, hematological disorders, vasculitis and
interventions was more or less similar to the largest cohort reported
from the rest of the world composed mostly of Nortwestern European
countries.[3,15] Most probably, the
inclusion of patients with only cortical or deep vein thrombosis was
the reason for this difference, supporting the clinical presentation
differences in CVT patients with and without BD emphasized in the
comparative study.[12] In a previous study of venous
thrombosis from Turkey, it was concluded that BD may be taking part
together with other etiologies in most of the cases;[16]
in that case when another etiology is found BD might have been
overlooked in some centers not so familiar with BD. On the other hand,
our center is a nationwide tertiary center with a specialized
multidisciplinary BD clinic and the frequency of CVT due to BD in our
center may be over-represented due to a selection bias. However, the
prevalence of BD was estimated as 42/10,000 (95% CI, 34-51/10,000) in
Istanbul, Turkey, supporting the notion that Turkey has the highest
prevalence rate of the disease in the world.[17]
Therefore it is not surprising to encounter BD as a frequent etiology
in CVT in the series reported from our center in Istanbul. Furthermore,
a recent review including CVT patients with BD mainly from countries in
the Mediterranean region showed that CVT incidence in BD was about 3
per 1000 person years.[18]
As mentioned above ¾ of the patients in ISCVT were women and the most
common risk factor was oral contraceptive use.[3]
However, in BD which is slightly more prevalent among males, serious
organ involvement is significantly more frequent in males and this
gender predisposition is also seen in cerebral venous thrombosis
patients with BD.[12] In the study where a direct
comparison was made in CVT patients with and without BD, CVT due to BD
was significantly more common among male patients. In the same study
the mean age was 26 in the non-BD group and 39 in the BD group,
resulting in a significant difference. However in the largest CVT
series published mean age was 37 for CVT patients, comparable to that
seen in BD patients with CVT.[3]
The rarity of acute presentation with neurological deficits and
seizures in patients with BD may preclude the inclusion of these
patients in other CVT series.[7] In CVT clinical
features differ according to the location and the extent of the
occlusion in the sinuses and veins and the course of the underlying
disease process. A slowly progressing dural sinus thrombosis that does
not affect the cortical venous circulation may present with isolated
headache and normal neurological examination findings. These patients
may be misdiagnosed as pseudotumor cerebri. However an acute clinical
presentation with focal neurological deficits and seizures can be
readily diagnosed as CVT with appropriate imaging techniques. CVT in BD
patients mostly presents with signs of isolated intracranial
hypertension and venous infarction rarely develops.[12]
As a consequence in CVT due to BD patients usually have an insidious
onset, they present usually with headache as the only symptom and the
neurological examination is normal or only papilledema or lateral gaze
paresis indicative of intracranial hypertension is found.
In the past, CVT used to be considered a condition with bad prognosis,
but currently CVT is considered to be a relatively more benign
condition with mortality rates below 10%.[19-23]
According to the limited follow-up data on CVT with and without BD
there were no significant differences between the two groups on
outcome.12 A greater tendency for recurrence was found in patients with
BD.[12] A cytopathological study on BD CVT cases is
not available however former autopsy findings on pulmonary arterial
thrombosis suggests an inflammatory process underlying the thrombosis.[24]
This finding may explain the chronic course of the thrombotic process
in CVT due to BD leading to the mentioned clinical differences.
The treatment of CVT mainly comprises of anticoagulation, with
subcutaneous fractionated heparin at the acute stage, and 6 months of
oral anticoagulation, afterwards.[25] However, since
the thrombosis of BD is considered an inflammatory process rather than
a procoagulant process,[26] treatment of these cases
may vary. Although treatment of CVT due to BD is still debated and
Class I evidence is lacking[27] our approach is to
use only steroids, instead of anticoagulants, as also suggested by
EULAR task force.[28] In such cases we usually give 5
consecutive days of IV methylprednisolone followed by a slow oral
taper.[29]
In recent years we also tend to add long-term azathioprine to prevent
recurrences or other vascular complications that could be seen in those
patients.[27] In intractable cases or repetitive CVTs
due to BD, anticoagulants may be added to steroids; but anticoagulants
should never be used alone.[29] It should be kept in
mind that pulmonary aneurysms should be ruled out before initiating any
anticoagulant treatment in patients with BD.
Due to the scarcity of data on CVT and inherited and acquired causes in
countries of the south-eastern Mediterranean region a comparison with
northwestern Mediterranean region is quite difficult to make. However,
one report emphasized the occurrence of CVT due to BD in Turkey which
deserves attention both in terms of the differences in demographic and
clinical features and possibly the treatment options. Therefore, in
patients with CVT from southeast Mediterranean region, BD should be
kept in mind especially if the patient is male, and if no other risk
factor can be identified. BD should always be questioned since
multi-etiology cases are not very rare. A multi-national and
multi-center prospective analysis of the CVT cases in south-east
Mediterranean region seems to be worthwhile in the near future.
References
- Stam J. Thrombosis of the cerebral veins and sinuses. N
Engl J Med. 2005 Apr 28;352(17):1791-8. http://dx.doi.org/10.1056/NEJMra042354
PMid:15858188

- Bousser MG, Ferro JM. Cerebral venous
thrombosis: an update. Lancet Neurol. 2007 Feb;6(2):162-70. http://dx.doi.org/10.1016/S1474-4422(07)70029-7

- Ferro JM, Canhao P, Stam J, Bousser MG,
Barinagarrementeria F. Prognosis of cerebral vein and dural sinus
thrombosis: results of the International Study on Cerebral Vein and
Dural Sinus Thrombosis (ISCVT). Stroke. 2004 Mar;35(3):664-70. http://dx.doi.org/10.1161/01.STR.0000117571.76197.26
PMid:14976332

- Saposnik G, Barinagarrementeria F, Brown
RD, Jr., Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and
Management of Cerebral Venous Thrombosis: A Statement for Healthcare
Professionals From the American Heart Association/American Stroke
Association. Stroke. 2011 Feb 3.

- N. Yesilot BAK, R. Tuncay, O. Coban and S.
Z. Bahar. Gender differences in acute stroke: Istanbul Medical School
Stroke Registry. Neurology India. [Original Article].
2011;59(2):24-9.

- Siva A, Altintas A, Saip S. Behcet's
syndrome and the nervous system. Curr Opin Neurol. 2004
Jun;17(3):347-57. http://dx.doi.org/10.1097/00019052-200406000-00017
PMid:15167071

- Criteria for diagnosis of Behcet's disease.
International Study Group for Behcet's Disease. Lancet. 1990 May
5;335(8697):1078-80. PMid:1970380

- Serdaroglu P, Yazici H, Ozdemir C, Yurdakul
S, Bahar S, Aktin E. Neurologic involvement in Behcet's syndrome. A
prospective study. Arch Neurol. 1989 Mar;46(3):265-9.
PMid:2919979

- Siva A, Kantarci OH, Saip S, Altintas A,
Hamuryudan V, Islak C, et al. Behcet's disease: diagnostic and
prognostic aspects of neurological involvement. J Neurol. 2001
Feb;248(2):95-103. http://dx.doi.org/10.1007/s004150170242
PMid:11284141

- Akman-Demir G, Serdaroglu P, Tasci B.
Clinical patterns of neurological involvement in Behcet's disease:
evaluation of 200 patients. The Neuro-Behcet Study Group. Brain. 1999
Nov;122 (Pt 11):2171-82. http://dx.doi.org/10.1093/brain/122.11.2171
PMid:10545401

- Houman MH, Neffati H, Braham A, Harzallah
O, Khanfir M, Miled M, et al. Behcet's disease in Tunisia. Demographic,
clinical and genetic aspects in 260 patients. Clin Exp Rheumatol. 2007
Jul-Aug;25(4 Suppl 45):S58-64.

- Yesilot N, Bahar S, Yilmazer S, Mutlu M,
Kurtuncu M, Tuncay R, et al. Cerebral venous thrombosis in Behcet's
disease compared to those associated with other etiologies. J Neurol.
2009 Jul;256(7):1134-42. http://dx.doi.org/10.1007/s00415-009-5088-4
PMid:19280104

- Biousse V, Ameri A, Bousser MG. Isolated
intracranial hypertension as the only sign of cerebral venous
thrombosis. Neurology. 1999 Oct 22;53(7):1537-42. PMid:10534264

- Otrock ZK, Taher AT, Shamseddeen WA,
Mahfouz RA. Thrombophilic risk factors among 16 Lebanese patients with
cerebral venous and sinus thrombosis. J Thromb Thrombolysis. 2008
Aug;26(1):41-3. http://dx.doi.org/10.1007/s11239-007-0093-x
PMid:17823778

- Sagduyu A, Sirin H, Mulayim S, Bademkiran
F, Yunten N, Kitis O, et al. Cerebral cortical and deep venous
thrombosis without sinus thrombosis: clinical MRI correlates. Acta
Neurol Scand. 2006 Oct;114(4):254-60. http://dx.doi.org/10.1111/j.1600-0404.2006.00595.x
PMid:16942545

- Gul A, Aslantas AB, Tekinay T, Konice M,
Ozcelik T. Procoagulant mutations and venous thrombosis in Behcet's
disease. Rheumatology (Oxford). 1999 Dec;38(12):1298-9. http://dx.doi.org/10.1093/rheumatology/38.12.1298
PMid:10587567

- Azizlerli G, Kose AA, Sarica R, Gul A,
Tutkun IT, Kulac M, et al. Prevalence of Behcet's disease in Istanbul,
Turkey. Int J Dermatol. 2003 Oct;42(10):803-6. http://dx.doi.org/10.1046/j.1365-4362.2003.01893.x
PMid:14521694

- Aguiar de Sousa D, Mestre T, Ferro JM.
Cerebral venous thrombosis in Behcet's disease: a systematic review. J
Neurol. 2011 Jan 6.

- Dentali F, Ageno W. Cerebral vein
thrombosis. Intern Emerg Med. 2010 Feb;5(1):27-32. http://dx.doi.org/10.1007/s11739-009-0329-1
PMid:19949894

- Dentali F, Gianni M, Crowther MA, Ageno W.
Natural history of cerebral vein thrombosis: a systematic review.
Blood. 2006 Aug 15;108(4):1129-34. http://dx.doi.org/10.1182/blood-2005-12-4795
PMid:16609071

- Breteau G, Mounier-Vehier F, Godefroy O,
Gauvrit JY, Mackowiak-Cordoliani MA, Girot M, et al. Cerebral venous
thrombosis 3-year clinical outcome in 55 consecutive patients. J
Neurol. 2003 Jan;250(1):29-35. http://dx.doi.org/10.1007/s00415-003-0932-4
PMid:12527989

- Preter M, Tzourio C, Ameri A, Bousser MG.
Long-term prognosis in cerebral venous thrombosis. Follow-up of 77
patients. Stroke. 1996 Feb;27(2):243-6. http://dx.doi.org/10.1161/01.STR.27.2.243
PMid:8571417

- Deschiens MA, Conard J, Horellou MH, Ameri
A, Preter M, Chedru F, et al. Coagulation studies, factor V Leiden, and
anticardiolipin antibodies in 40 cases of cerebral venous thrombosis.
Stroke. 1996 Oct;27(10):1724-30. http://dx.doi.org/10.1161/01.STR.27.10.1724
PMid:8841318

- Hamuryudan V, Er T, Seyahi E, Akman C,
Tuzun H, Fresko I, et al. Pulmonary artery aneurysms in Behcet
syndrome. Am J Med. 2004 Dec 1;117(11):867-70. http://dx.doi.org/10.1016/j.amjmed.2004.05.027
PMid:15589493

- Einhaupl K, Stam J, Bousser MG, De Bruijn
SF, Ferro JM, Martinelli I, et al. EFNS guideline on the treatment of
cerebral venous and sinus thrombosis in adult patients. Eur J Neurol.
2010 Oct;17(10):1229-35. http://dx.doi.org/10.1111/j.1468-1331.2010.03011.x
PMid:20402748

- Yazici H. Behcet's syndrome: an update.
Curr Rheumatol Rep. 2003 Jun;5(3):195-9. http://dx.doi.org/10.1007/s11926-003-0066-9
PMid:12744810

- Saadoun D, Wechsler B, Resche-Rigon M,
Trad S, Le Thi Huong D, Sbai A, et al. Cerebral venous thrombosis in
Behcet's disease. Arthritis Rheum. 2009 Apr 15;61(4):518-26. http://dx.doi.org/10.1002/art.24393

- Hatemi G, Silman A, Bang D, Bodaghi B,
Chamberlain AM, Gul A, et al. EULAR recommendations for the management
of Behcet disease. Ann Rheum Dis. 2008 Dec;67(12):1656-62. http://dx.doi.org/10.1136/ard.2007.080432
PMid:18245110

- Akman-Demir G SS, Siva A. Behcet’s
disease. Current Treatment Options in Neurology. 2011
Jun;13(3):290-310.
