Received: January 15, 2015
Accepted: March 18, 2015
Mediterr J Hematol Infect Dis 2015, 7(1): e2015031, DOI 10.4084/MJHID.2015.031
This article is available on PDF format at:

Ludmila Mourão Xavier Gomes1, Thiago Luis de Andrade Barbosa2, Elen Débora Souza Vieira2, Lara Jhulian Tolentino Vieira2, Karla Patrícia Ataíde Nery Castro2, Igor Alcântara Pereira2, Antônio Prates Caldeira2, Heloísa de Carvalho Torres3 and Marcos Borato Viana1
1 Núcleo de Ações e Pesquisa em Apoio Diagnóstico, Federal University of Minas Gerais, Belo Horizonte, Brazil
2 Department of Medicine, State University of Montes Claros, Montes Claros, Brazil
3 Department of Applied Nursing, Federal University of Minas Gerais, Belo Horizonte, Brazil

| This is an Open Access article distributed
under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |
|
Abstract Introduction. Despite advances
in the management of sickle cell disease, gaps still exist in the
training of primary healthcare professionals for monitoring patients
with the disease. Objective. To assess the perception of community healthcare workers about the care and monitoring of patients with sickle cell disease after an educational intervention. Method. This exploratory, descriptive, and the qualitative study was conducted in Montes Claros, state of Minas Gerais, Brazil. The intervention involved the educational training of community healthcare workers from the Family Health Program of the Brazilian Unified Health System. The focus group technique was used to collect the data. The following topics were covered in the discussion: assessment of educational workshops, changes observed in the perception of professionals after training, profile of home visits, and access to and provision of basic healthcare services to individuals with sickle cell disease. The discussions were tape-recorded and transcribed verbatim. The data were subjected to content analysis and empirically organized into two categories. Results. Changes in the healthcare practices of community health workers were observed after the educational intervention. The prioritization of healthcare services for patients with sickle cell disease and monitoring of clinical warning signs in healthcare units were observed. Furthermore, changes were observed in the profile of home visits to patients, which were performed using a script provided in the educational intervention. Conclusion. The educational intervention significantly changed the work process of community health workers concerning patient monitoring in primary healthcare. |
Introduction
Sickle cell disease (SCD) is the most important hemoglobinopathy
worldwide and is associated with high morbidity and mortality.[1] In
Brazil, SCD is a relevant public health topic, considering the
epidemiological, clinical, economic, and social issues involved. The
prevalence of sickle cell trait in Brazil is estimated to be between 2%
and 8%,[2] depending on the ethnic composition of the regional
populations. The incidence of SCD in Minas Gerais, a Southeastern
state, is 1:1,400 newborns, according to the Newborn Screening Program
(NSP-MG).[3]
The results of the NSP-MG have been rewarding, but
many challenges remain regarding patient care, including the training
of healthcare professionals in educational activities and the provision
of continuous patient care to reduce morbidity and mortality.[3,4]
Research conducted in Minas Gerais showed poor knowledge of primary
care professionals about many aspects of SCD. Poor knowledge probably
reflects badly on the quality of healthcare provided to people with SCD
and their families.[5]
One study that evaluated the perception of
patients with SCD identified several limitations related to providing
primary healthcare to them. These limitations included restricted
access to healthcare services, lack of communication between primary
and secondary healthcare professionals, and lack of confidence in the
ability of primary care professionals to accurately provide information
related to the disease.[6]
Experiences of educational
interventions for primary healthcare professionals about SCD are
scanty. Additionally, they had limited goals such as communication of
newborn screening results[7] and communication skills to offer prenatal
screening for SCD and thalassemia.[8] There are no studies of
educational interventions targeting primary healthcare professionals to
address general care to patients with SCD.
In Brazil, the Family
Health Program has been implemented to strengthen primary healthcare
and reorganize the assistance model in the Brazilian Health System
(Sistema Único de Saúde - SUS). Considering its principles and the
organization of its work processes, the Family Health Program provides
conditions to mitigate the indicators of suffering caused by chronic
diseases such as SCD. Moreover, the Program is characterized by the
integrated work of a multidisciplinary team comprising doctors, nurses,
nurse technicians, and community health workers.[9,10] Community health
workers are essential for the Family Health Program because they reside
in the same area where they work, conduct home visits, and so they can
fully understand the community’s health problems, way of life, and
culture.[11] Therefore, these workers require clear and objective
information from the technical–scientific area to guide community-based
activities,[12,13] and training of these professionals is crucial.
The
aim of this study was to analyze the perception of community primary
healthcare workers about the care and monitoring of individuals with
SCD after an educational intervention.
Methods
This exploratory, descriptive, and qualitative study was conducted
in basic healthcare units of Montes Claros, state of Minas Gerais,
Brazil. Montes Claros is situated in a region with a high prevalence of
SCD. The study was conducted after the educational intervention for
community health workers.
Educational intervention.
The intervention consisted of the training of community health agents
in the Family Health Program on the primary care and monitoring of
individuals with SCD. It was conducted by three nurses who were
previously trained via a 90-hour distance learning course over a
3-month period. Activities were conducted in the form of active
methodologies such as case studies, meetings, stage plays, and
parodies.
The contents and design of the program are depicted in Table 1.
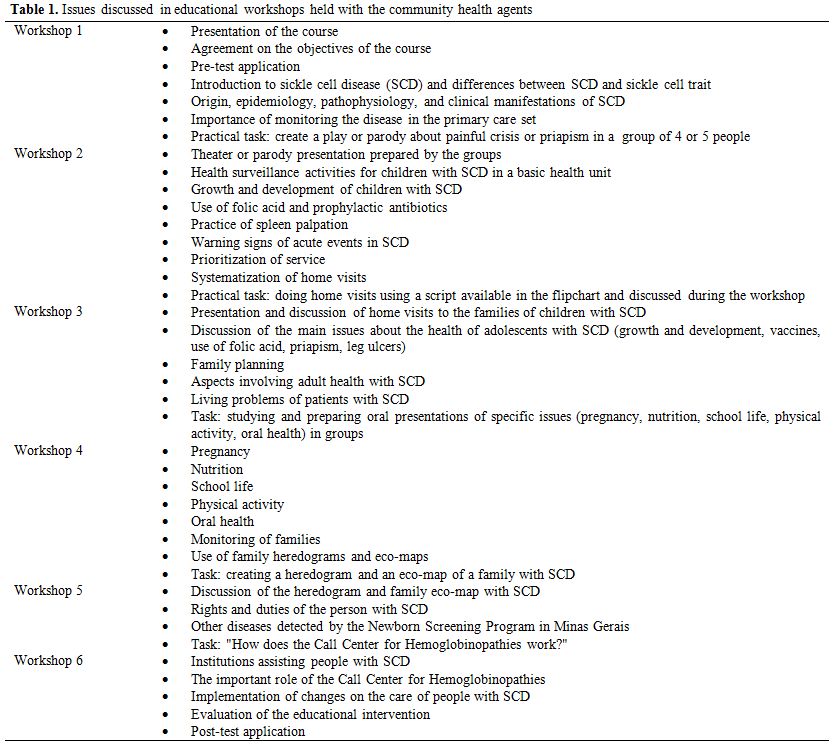 |
Table 1. Issues discussed in educational workshops held with the community health agents |
The
educational intervention lasted 40 hours: 30 hours in the classroom and
10 hours outside the classroom. Six 5-hour meetings were conducted with
healthcare professionals at intervals of 7 days. After each workshop,
the professionals were assigned homework related to the topics, which
would be addressed in the subsequent workshop.
On completion of
training, two visits were made to healthcare units and involved
discussions on the main topics and guidance on patient monitoring.
A
total of 68 community health agents who assisted patients with SCD and
were from six basic healthcare units were trained. Medical records from
the NSP-MG were used. In addition, each healthcare team was
interrogated about the presence of individuals with SCD in each
jurisdiction.
Participants.
Three months after the intervention, the trained community health
agents were invited to participate in a meeting in a room provided by
the Health Department of Montes Claros. The professionals were selected
on the basis of the following criteria: (i) worked in the Family Health
Program during the study period, i.e. they were not on vacation or work
leave; (ii) their jurisdiction assisted patients with SCD; (iii) they
passed the course with a minimum attendance of 80%; and (iv) they
agreed to participate in the study. Among the 68 trained community
health agents, 27 worked in jurisdictions containing patients with SCD,
and two refused to participate in the study. Consequently, 25 community
health workers were selected to participate in this study.
Data
collection. The focus group technique was used, allowing interaction
and discussions of aspects related to training and changes implemented
in daily activities involving patient care and monitoring.[14] For the
focus discussion, a moderator and two observers who had not
participated in the educational intervention were present. The focus
groups sessions lasted no more than a hundred minutes and used a plan
that included the following topics: assessment of educational
workshops, changes observed in the professionals after training,
profile of home visits, access to and provision of basic healthcare to
individuals with SCD. The discussions were tape recorded and later
transcribed verbatim. The focus sessions were conducted with two
groups, one with 12 participants and the other with 13. The
professionals were allocated to each focus group on the basis of their
availability on previously scheduled dates. Each group participated in
only one focus session. The number of groups formed for the focus
sessions allowed the data to reach saturation range, ensuring that no
new or relevant data were missing when data collection was completed.
Analysis of the data.
The data were subjected to thematic content analysis according to the
following steps: preanalysis, content analysis, processing of the
results, and interpretation.[15] Subsequently, the data were organized
into two empirical categories. Statements from participants were
identified by letter codes accompanied by Arabic numerals. The two
focus groups were designated G1 and G2, and participants received a
code with the letter P.
Ethical aspects.
The confidentiality and anonymity of study participants were guaranteed
throughout the study. This study was approved by the Research Ethics
Committee and was registered in the Brazilian National Council of
Research Ethics under protocol CAAE-0683.0.203.000-11.
Results
The profile of the 25 professionals is presented in Table 2.
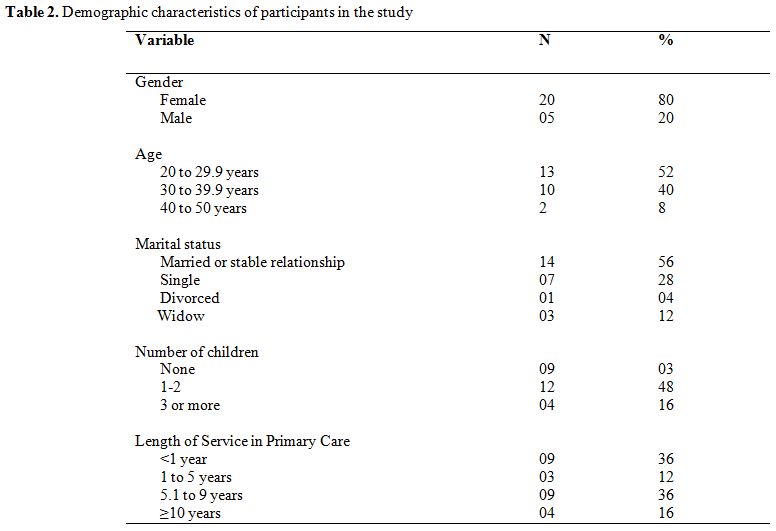 |
Table 2. Demographic characteristics of participants in the study |
In the focus group, two categories emerged based on the
participants’ statements, as follows: “perception of the educational
intervention” and “training for the promotion of changes in the work of
the professionals.”
Perception of educational intervention.
In this category, the professionals discussed the topics and evaluated
training performed. The educational intervention received a positive
assessment from participants, and they gained deeper knowledge about
different aspects of patient care and monitoring:
“Training
was great, since I had the freedom to play, role play, relax, and
clarify many topics. On our own, we were looking for knowledge about
the disease through the problems we encounter in our daily lives.” G2P4
“We
didn't know about priapism, wounds, the natural history of the disease,
the age of each medication, electrophoresis, and enlarged spleen.”
G2P10 and G2P8
Community health workers covered many topics
related to SCD that they were unaware of; these topics were addressed
in workshops. Negative experiences prior to training were mentioned by
the professionals. Among these, the most important was the lack of
awareness about priapism:
“I had
a very bad negative experience, I went to the house of a young man with
SCD who had an erection at the time of the visit. I left in a hurry
because I didn't know what priapism was. Today I know how to handle
this situation.” G2P10
It was noted that before the
intervention, some professionals stated that they were unaware on how
to manage patients with SCD in healthcare units. The course taught them
how to monitor patients, and the professionals considered the
educational intervention to be relevant to their everyday practice:
“This
course was very important to our practice. By knowing all these
aspects, now we can take better care of the person who has this
disease. Now we pay more attention when a person with SCD arrives in
our unit.” G1P1 and G1P7
“The
course made me think about my own work. I didn't pay much attention to
my patients SCD, but the course awakened my interest in caring.” GP1P2
Training to promote changes in the routine work of professionals. Of note, this category included changes implemented by community health agents in their practice after training (Table 3).
They discussed changes in areas such as the prioritization of services,
treatment of new patients, home visit routines, and monitoring of
specific outcomes of patients with SCD. These changes are described
below as subunits of this thematic category.
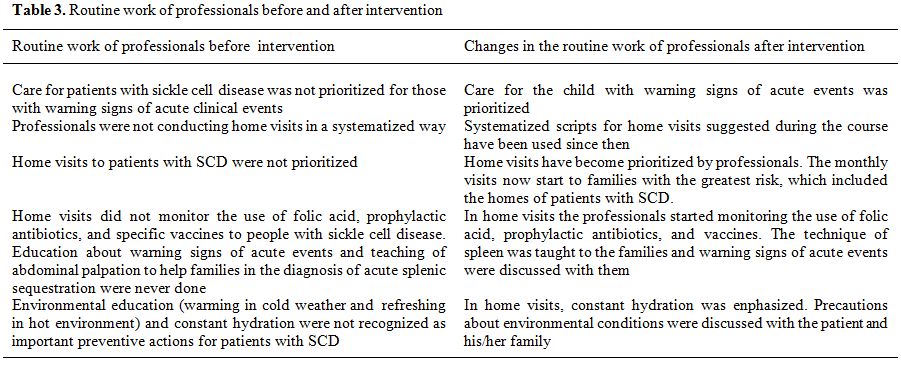 |
Table 3. Routine work of professionals before and after intervention |
Subtopic: Prioritizing care and treating new patients in the health unit.
Prior to training, healthcare professionals lacked knowledge regarding
the need for prioritizing the care for patients with SCD. They were not
able to understand why mothers of children with the disease were so
critical regarding delays in care for their children and kept insisting
on it to be prioritized:
“It was
in the course that I understood the issue of priority of care. I
started thinking about the mother in my area who has two boys with SCD,
and who comes to the unit and requests her children to be assisted
quickly, unlike other mothers of children who do not have SCD.” G1P10
After
training, the professionals stated that they prioritized care for the
child visiting their unit with warning signs. Furthermore, they
promptly provided humanized care services to individuals with SCD.
“When
the mother comes in, I inquire whether the child has fever, because it
is a risk situation. I also note if the child has pain in the belly,
which can be a problem in the spleen.” GP2P12, G2P8.
Disease
surveillance was performed for every child who visited the healthcare
unit to have anthropometric measurements. In cases where the child had
any health problems or warning signs, health services were performed
promptly:
“The child came to
get weighed and was complaining of fever. So I went and talked to the
doctor. Then the child was examined promptly and the problem was
solved.” GP2P4
Subtopic: changes in the home visit routine.
The main changes referred to by the professionals occurred in home
visits, which were performed using systematized scripts introduced in
the course. Community health agents reported that home visits to
patients with SCD became more time consuming because these
professionals were concerned about evaluating other health aspects and
providing targeted orientation. In addition, the visits became
prioritized, i.e., the professionals made their monthly visits starting
with families with the greatest risk, which included the homes of
patients with SCD:
“The visit
takes much longer. I see if the child in my area is taking folic acid
and antibiotics to prevent complications and remember of the
vaccination programs. I teach them about palpating the spleen and
warning signs. I didn't do this prior to the course.” G1P11
According
to the professionals, the primary change in home visits after training
was monitoring the use of folic acid, prophylactic antibiotics, and
vaccines in patients as well as teaching them how to palpate the spleen
and diagnose warning signs.
In home visits, orientations on
precautions about environmental conditions were conducted, and the need
for constant hydration was also taught, improving care for her child:
“In
one case, the mother worked by selling door-to-door and used to take
the child with her, exposing the child to the sun, which in turn led to
bouts of pain. So I told the mother about the risk of dehydration, and
now she is avoiding taking the child with her, and always hydrates her,
and this is the result of the course. G1P9
Discussion
The educational intervention received a positive evaluation from
community health agents. In addition, the intervention produced changes
in the daily work of these professionals.
Because of its dialectic
and problem-based approach as well as the use of various educational
resources that allowed participants to interact, the educational
intervention increased awareness of community health agents about the
care and monitoring of individuals with SCD. During training workshops,
the professionals reflected on their role in patient care. The
dialectic approach of educational activities provided individuals with
the opportunity of self-reflection and to consider themselves as
promoters of change. In this sense, the educational intervention aimed
to contribute to the pursuit of transformation, and changes were
produced following training.[16]
The experiences
and problems described by healthcare workers during professional life
in the health team redirected their attention to training with the
purpose of improving care. In this context, continuing education is
considered important and is understood as “learning at work, in which
learning and teaching are incorporated into the daily lives of
organizations and work”.[17] The aim of continuing
education is the training of health workers, considering their own
experiences and the problems they face.
In the perception of
these professionals, the educational intervention led to changes in
their healthcare practices. One of these changes was the prioritization
of care for patients with SCD showing warning signs of acute events,
such as fever, pain, sudden increase in pallor, worsening jaundice,
abdominal distension, enlarged spleen or liver, cough or difficulty in
breathing, priapism, neurological changes, inability to swallow
liquids, dehydration, vomiting, and hematuria.
The
professionals’ statements indicated that mothers of children with SCD
were more demanding and required immediate care for their children.
This fact can be explained by the occurrence of vaso-occlusive
phenomena that can lead to serious complications such as stroke when a
child showing warning signs is not treated quickly. Knowledge derived
from the educational intervention allowed the provision of better care
because it changed the professionals' perception of the mothers who
demand immediate care for their children during emergencies. In their
daily work, community health agents alerted other team members to
expedite care as soon as they detected warning signs.
A relevant
point in the professionals’ statements was related to patient
monitoring. The professionals were aware of the warning signs and
always interrogated the responsible parties about these signs. This
happened, for example, when the child visited to the clinic for
anthropometric measurements and any complaints were noted by the
professionals or reported by the mother or guardian. A routine
appointment can then become an urgent situation for community health
workers.
Surveillance activities undertaken by community agents
are not restricted to the health units. A study of primary healthcare
professionals in Brazil found that community workers have acted more
intensely in the areas of education and coordination of information
between the healthcare team and service users. Moreover, they performed
various outdoor activities in streets, homes, and reference points in
the community. Home visits were the main activity of these
professionals.[18] Another study found that home
visit procedures conducted by community health workers were not
standardized and were defined by each professional. Moreover, home
visits are scheduled on the basis of their experience and physical
location within each service region. Home visits, therefore, become
bureaucratic reproductions of medical consultations, where forms are
completed and routine updates are provided, limiting the establishment
of a relationship between the healthcare team and service users.[19]
In
patients with SCD, patient monitoring through regular, targeted home
visits is essential to achieve more effective therapeutic results. The
results of the present study showed that home visits became
systematized and targeted to patients with SCD after adoption of a
script provided in the educational intervention. Moreover, changes were
observed in the prioritization of home visits to patients with SCD
because these families are at a greater risk. In this respect, the
prioritization of home visits benefited not only individuals with SCD
but also families that constituted risk groups. In the systematized
home visits, the professionals guided patients on the use of folic
acid, prophylactic antibiotics, and vaccines and taught family members
how to palpate the child’s spleen. Monitoring the use of folic acid in
home visits is necessary to cope with accelerated erythropoiesis, a
specific feature of the disease.[20] Adherence to drug therapy is a relevant issue in patient monitoring, as previously reported.[21,22]
When community health agents noted poor adherence to the recommended
drug therapy in home visits, these visits became more time consuming
because of the constant need to explain the importance of preventive
healthcare measures to families.
The vaccination status should be
monitored during visits both in relation to the basic vaccination
schedules and the vaccines recommended for SCD. Previous studies
indicated that vaccination coverage in relation to the basic calendar
varied between 65% and 100%.[4,23]
However, this is not the reality for all vaccines. In Brazil, vaccines
for pneumococcus and meningococcus were included in the basic
immunization schedule in 2010. Prior to this date, two studies in the
Brazilian states of Minas Gerais and Espírito Santo showed that 43.8%
and 50% of children with SCD, respectively, had incomplete immunization
against pneumococcus.[4,24] A study
in London found that immunization against encapsulated bacteria and the
flu virus was also precarious among adults and children with SCD.[25] In Madrid, the regular vaccine coverage was 85%. It was 50% for flu virus and 15% for hepatitis A.[26]
Home
visits are also conducive to teaching parents how to palpate the spleen
for the early diagnosis of acute splenic sequestration. Instructing
parents on this technique can decrease mortality, considering that this
outcome can quickly lead to death. Other educational activities
conducted by these professionals also cover environmental education and
the perception of warning signs. Families are instructed to keep
patients hydrated and away from adverse environmental conditions, such
as extreme heat and cold. The diagnosis of warning signs allows parents
to identify changes that demand emergency care considering the level of
complexity required. This information may help reduce patient mortality
and prevent sickle cell crises.
The limitations of the present
study are related to data collection. The focus group has limited
ability to make inferences about large population groups and cannot
test hypotheses in experiments.[14] Another
limitation derives from the lack of interviews with the same
participants to compare individualized results of the focus
discussions. In this respect, participants may change their opinions
during the focus discussions because of the positioning of the
researchers about sensitive issues. In addition, the effects of
training community agents on patients' health were not assessed because
these effects were not included in the study objectives.
Conclusion
The educational intervention on SCD produced changes in the
attitudes of healthcare professionals to improve the quality of care
provided to individuals with SCD. Knowledge acquired in training
changed attitudes and improved their skills.
Based on these
results, we suggest the widespread training of community health workers
who treat SCD patients in their service area. The educational
intervention studies that include higher-level primary healthcare
professionals are also recommended.
Considering the limited
knowledge about SCD and primary healthcare, further studies are
recommended, particularly those that directly assess the effects of
training on the health of patients with SCD.
Acknowledgements
References
 .
. .
.  .
. .
.  .
. .
.  .
.  .
. .
. .
. .
. .
. .
.  .
. .
.  .
. .
. .
. .
. .
. .
. .
.[TOP]