There is a paucity of data on extended red cell phenotype from this vast country. Few studies have been done from different areas of the country at different period.[7-11] Out of these studies, only one study has been done on a tribal population of India.[10] In a tribal population of South Gujarat sickle cell anemia is common[12] but transfusion associated alloimmunization is not uncommon.[13] Unfortunately studies on transfusion associated alloimmunization in sickle cell anemia patients in India are rare.[13,14]
With this purpose in mind we serologically phenotyped 222 regular voluntary blood donors and 113 tribal populations (tribes like Adivasi, Bhil, Vasava, Gamit, Chaudhary, Dhodiya Patel, Koli Patel, Rathod, Hrijan, Halpati etc. They all speak Gujrati language now a days). There are about 0.5 million of them around the city of Surat. Samples for the blood group antigens ie. Rh (D,C,E,c,e), Kell (K, k), Duffy (Fya, Fyb), and Kidd (Jka, Jkb) blood group antigens. The study was cleared by Institutional Ethics Committee (SRKRC/RP/01/2017). Sampling of regular voluntary blood donors was conducted after taking consent from the outdoor blood donation camps organized by Surat Raktadan Kendra & Research Centre (SRKRC) whereas sampling of tribal population was from the Thalassemia and Sickle cell anemia checkup camps organized by SRKRC in and around the areas of Surat City. The blood grouping for the above antigen types was done by conventional tube technique. Anti-A, Anti B, Anti-AB, Anti-D, and Anti human Serum (AHG) were from Arkray Health Care Pvt Ltd (Gujarat India), Anti-C, Anti-c, Anti-E, Anti-e Anti-K, Anti-Jka, Anti-Jkb, were from DIAGAST (France), Anti-k, Anti-Fya, and Anti-Fyb were from Immucor Inc (U.S.A). All reagents were used as per the manufacturer’s instructions. Appropriate controls were kept. The following antigens were detected in saline phase: C, c, E, e, Jka, Jkb, K and Indirect Antiglobulin Test (IAT) was performed for Fya, Fyb, and k antigens. Before analyzing the data invalid results were repeated or discarded. Chi-square test was performed to compare the frequency distribution of clinically important blood group antigens amongst non-tribal and tribal population.
All 222 individuals tested in this study were voluntary, unrelated and unpaid blood donors. The age group of voluntary blood donors was 18-65 years and tribal student’s age group was 14-18 years. Amongst 222 voluntary blood donors, female donors were 6. Table 1 gives the phenotype frequency of important blood groups of different systems. The D antigen frequency was 96.6% and 96.5% in non-tribal and tribal population respectively. The incidence of K antigen was 2.4% in non-tribal population whereas no sample of tribal population was found positive for K antigen. There was significant difference in distribution of some of the antigens between these two groups particularly k, Fyb and Jka antigens. Fy (a+b-) and Jk (a+b-) were the common phenotype for Duffy and Kidd system respectively in both the groups. Significant variation in distribution is marked in table 2.
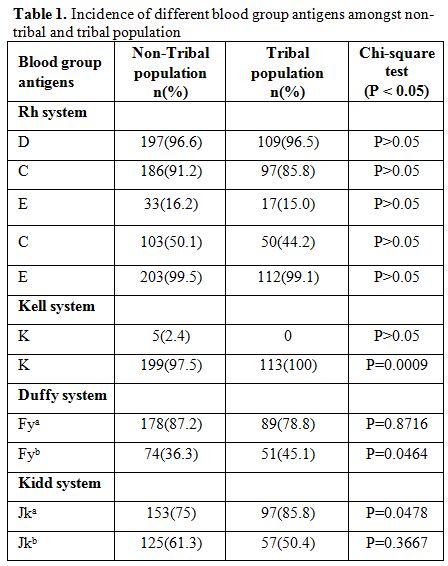 |
Table 1. Incidence of different blood group antigens amongst non-tribal and tribal population. |
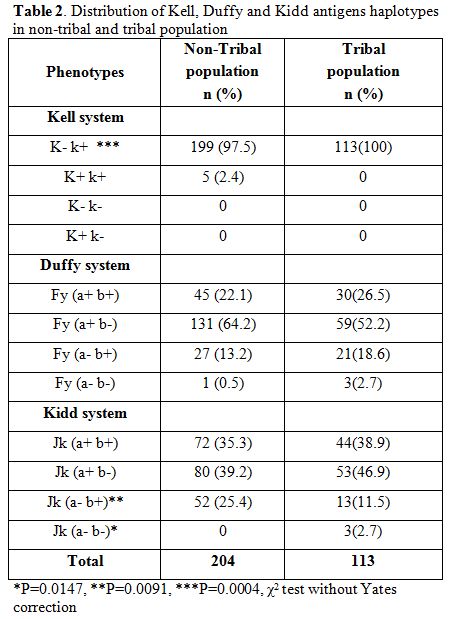 |
Table 2. Incidence of different blood group antigens amongst non-tribal and tribal population. |
Very few studies regarding the incidence of various blood groups in the blood donor population are published from India[7-11] and only one study from the blood donor population of South Gujarat.[8] Tribal population in South Gujarat like Adivasi, Bhil, Vasava, Gamit, Chaudhary, Dhodiya Patel, Koli Patel, Rathod, Hrijan, Halpatietc are of australoid types and though there are several tribes in this area but thousands of years of living together in the same environment has led to some amount of mixing of the population. Hence we have taken them as one group for the purpose of present study. Distribution of blood group antigens amongst them supports the idea.[10,15]
The incidence of Rh antigens D, C, c, E, e differs in different ethnic population.[1,2] In present study, D antigen frequency in both the groups is more than in Whites and comparable with other Indian studies.[7-11] C antigen frequency in non-tribal and tribal group in this study is high than in Whites and in Blacks[2] while comparable with findings by Thakral et al.[7] Frequency of c antigens in non-tribal and tribal groups is less than in Whites and Blacks and comparable with other Indian studies.[7,8] Frequency of E antigen was low in both the groups compared to other Rh antigens that are comparable with other Indian studies.[7,8]
Frequency of k antigen was 100% in non-tribal and tribal population, which is comparable with other Indian studies.[7,8] Jk (a+b-) was the commonest both the groups followed by Jk (a+b+) and is comparable to that found by Nanu and Thapliyal,[11] Thakral et al,[7] and the White population (48.37, 49.21, and 49%, respectively for Jk (a+b+)). Fy(a+b-) phenotype with a frequency of 64.2% was found to be the commonest in the both the groups which is comparable to that observed in Thakral (43.85%)[7] and Nanu and Thapiyal (40.8%);[11] however, it is in contrast with the studies reported frequency of Fy(a-b-) phenotype in Blacks (68%) as well as the study done by Kahar et al (37.39%).[8]
In our population we have 4.4% beta-thalassemia trait (BTT) and 1.3% sickle cell anemia trait (SCT).[12] Patel et al reported prevalence of BTT and SCT in Gamit (15.9%, 22.7%), Vasava (13.6%, 15.2%) and more than 10% prevalence of SCT in Chaudhary. They also reported mild to moderate anemia in tribal groups.[12] In our pervious study prevalence of alloimmunization in multitransfused sickle cell disease patients is 12% compared to multitransfused thalassaemia patient of 1.2%. Majority of the antibodies were directed to c, E, Jk and Kell antigens.[14] Multi transfused patients from tribal groups rely their blood sources for transfusion from nontribal population who constitute 98% of the donor pool in this tribal dominated area.
In conclusion, present study does show significant difference in the phenotypic frequency of clinically significant red cell antigens like K (P<0.00009), Fyb (P<0.0464) and Jka (P<0.0478). Kell antigen was totally absent in tribal population and E antigen was present in 16% of the donors but was absent in 84% tribals population similarly cantigen which is present in 50% of donor population was absent in 56% recipient population explaining the distribution of alloantibodies. Moreover there were significant differences in red cell antigens in our both tribal and blood donor groups when considered against Caucasian and Afrocaribbean population.
The present study was done in a smaller number of tribal populations, and the findings need to be expanded on a larger study.
Differences of distribution of common donor red cell antigens in blood donor population from India, when contrasted with Caucasian and Afrocaribbean population, have important implication as many such patients who have sickle cell anaemia or otherwise come to India for medical tourism and they may receive several units of red cell transfusion for various surgical and organ transplantation purposes. Unless extended red cell phenotypic match is performed, many such patients will develop alloantibodies.