Andriani A., Marchetti L., Rossi F., Perretti M.A., Raja S. and Recine U.
UO of Internal Medicina, Villa Betania Hospital, Rome.
Published: March 01, 2024
Received: January 22, 2024
Accepted: February 12, 2024
Mediterr J Hematol Infect Dis 2024, 16(1): e2024030 DOI
10.4084/MJHID.2024.030
This is an Open Access article distributed
under the terms of the Creative Commons Attribution License
(https://creativecommons.org/licenses/by-nc/4.0),
which permits unrestricted use, distribution, and reproduction in any
medium, provided the original work is properly cited.
|
To the editor
Due
to the availability of more and more new biological therapies,
outpatient/DH treatment of most hematological patients has become the
standard cure regimen. New therapeutic strategies are orally or
subcutaneously administrated and only in a few cases intravenously. For
these reasons, the majority of patients are treated at home or as an
ambulatory/Day Hospital regimen. The Hematological Department admits
for treatment in ordinary hospitalization H24 exclusively patient
candidates for intensive and high-dose or biological therapies that
need strict, continuous, and skillful supervision.
New drugs have
different toxicities, not only hematological but also cardiovascular,
pulmonary, neurological, and cutaneous. For these reasons, when a side
effect occurs, many patients are hospitalized in Internal Medicine
wards.[1,2] Often, in these departments, physicians
should have training to face hematological problems. For this reason,
we proposed to activate a section inside the Internal Medicine ward of
Villa Betania Hospital in Rome, where a team of hematologists and
hospitalists could take care of frail hematological patients with
comorbidity or complications of hematologic therapy.
Patients and
Methods
From
January 2022 to July 2023, 112 pts (53 M, 60 F, median age 77 years)
were admitted to our ward, forwarded by various Hematological
Departments or by the Emergency Departments of General Hospitals in
Rome (Policlinico Umberto I°, S. Filippo Neri, S. Spirito, S. Giovanni,
S. Eugenio, S. Andrea and Cristo Re). All patients were followed and
treated at home for their hematological disease, and they came to the
emergency room due to the complications or progression of the disease;
before being transferred to our Department, patients were evaluated by
the referring hematologist's final decision to send them back home or
to admit them into hospital. The transfer request was sent by mail or
fax to the emergency room together with the patient's clinical report.
The patient admittance in our ward has been granted within 12-72 hours
of the invoiced request.
Patient Typology
During
the study period, our hospital received 112 requests by mail or fax for
admitting patients affected by hematologic disease or complications of
hematologic therapy, such as diabetes, cardiac failure, second primary
neoplasm, sepsis, other infections, hemorrhages, etc. The main
characteristics of patients and the type of hematological disease are
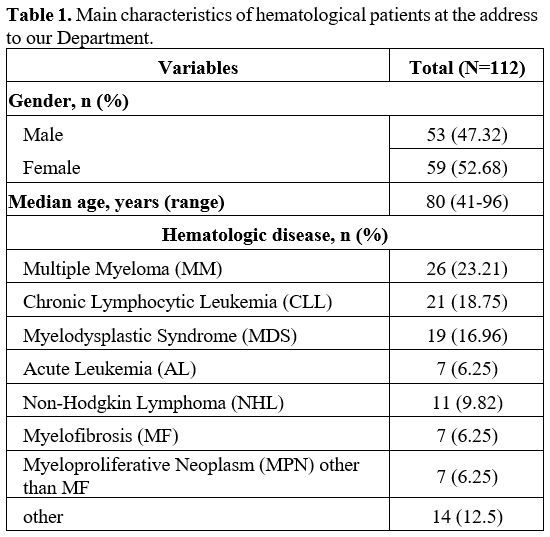
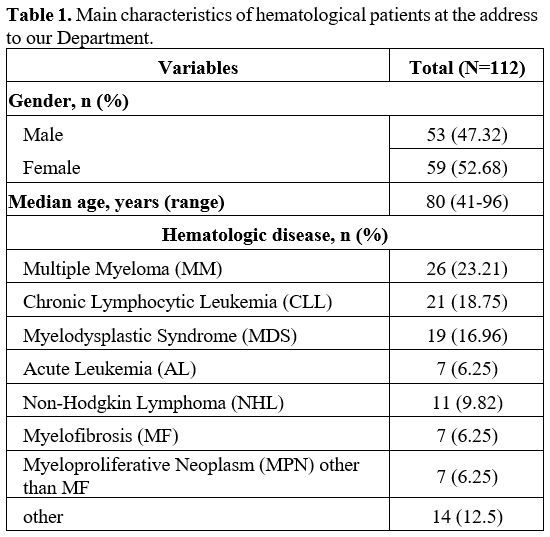
shown in Table 1.
All
admitted patients were assisted with specific therapies according to
the specific complications or complaints (transfusional or supportive
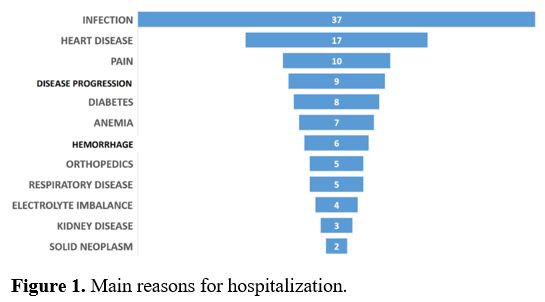
therapy as antibiotics, hydration, etc.) (Figure 1).
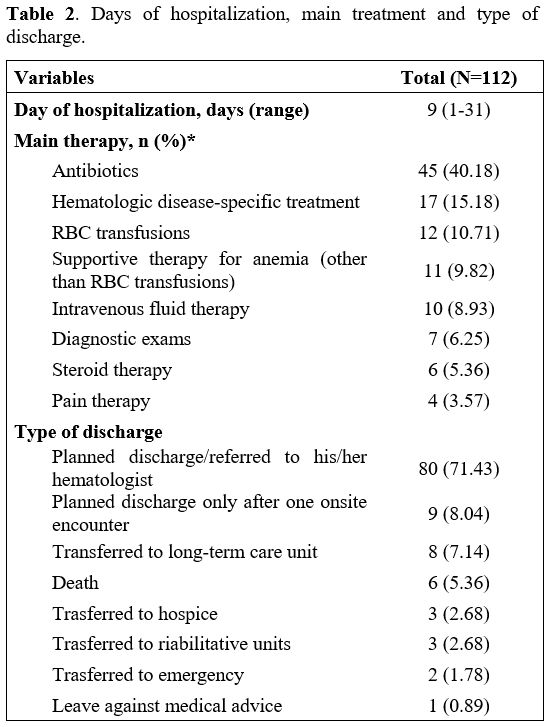
89
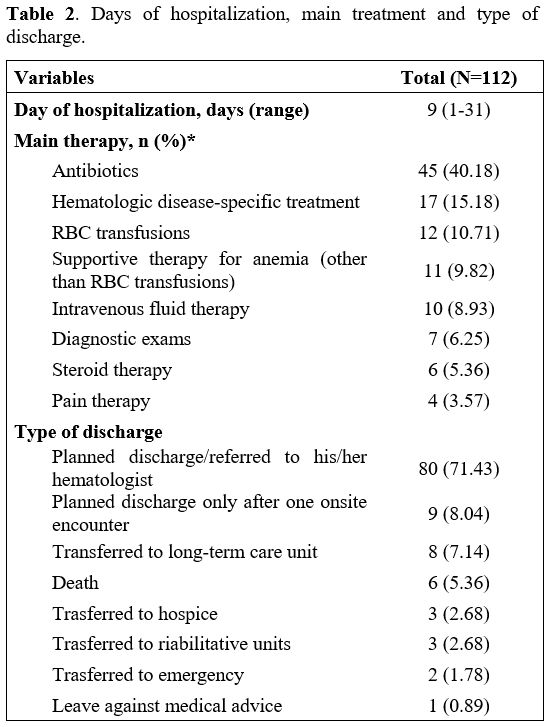
out of 112 were referred back to their hematologist; 9 patients were
followed after discharge at least once before referring back to sending
hematologists; 11 were sent to long-term or motor rehabilitation
hospitalization, 3 pts were entrusted to the hospice, 1 patient left
without medical consent and 6 pts died for complications. Only 2 pts
were sent back to the emergency room for complications during the
hospitalization (Table 2).
 |
Table
1. Main characteristics of hematological patients at the address to our Department. |
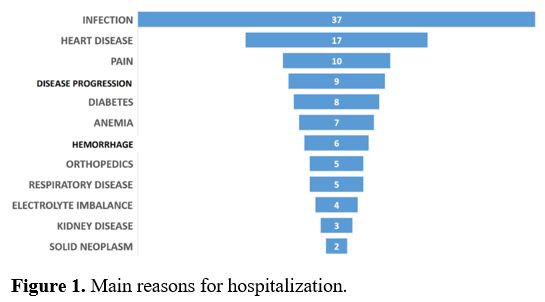 |
Figure 1. Main reasons of hospitalization. |
 |
Table
2. Days of hospitalization, main treatment and type of discharge.
|
Discussion and Conclusions
In
recent years, the treatment of hematological diseases has been
continuously evolving. New target therapies can be administered in
ambulatory or in Day-Hospital regimen. More drugs can be taken orally
or subcutaneously,[3,4] and patients can also be treated at home.[5,6] These new modalities of treatments have changed the quality of life of patients, their family, and their habits.[7]
Certainly, these new types of treatments have led to a bed number
reduction in Hematology Departments, reserving them only for the most
complex and intensive therapies. These new molecules are more effective
in terms of therapeutic results, but they can cause side effects
worsening comorbidities which require the internist skills.
An
ever-increasing number of hematologic patients on therapy are forced
back toward the nearest hospital for complications. In the emergency
room only, the acute problem is usually treated. Then, the patients are
transferred to medical divisions where hematologists are rarely on
duty, and physicians are frequently not used to treating this type of
pathology. For this reason, the birth of departments of internal
medicine with hematological skills can help and support the outcome of
these frail patients.
The median life of the population has been
prolonged, so the majority of hematological diseases appear over sixty
years in patients with comorbidities, and the possibility of treating
complications and comorbidity at the same time can determine a better
outcome and survival. For this reason, we have implemented, as a pilot
section in a generalist hospital, some beds to admit and treat these
patients by a team of hematologists and hospitalists working together.
Our
results are encouraging because we have managed to ameliorate the
outcome of these particularly frail patients, referring most of them
back to their hematological team for continuing specific treatment.
Only a few patients died of complications, so almost all patients had
their acute medical complications resolved. This type of organization
can lighten the workload of hematological departments, integrating more
specialists in the treatment of these complex patients. Moreover, we
have to consider health cost reduction by employing non-specialist
departments, which are less expensive for technical resources and
medical personnel than specialist wards.[8]
In
conclusion, this new specific regimen of assistance has achieved its
expected goal of taking care of comorbid, frail patients with
complications of hematological disease or therapy. An internal medicine
department, where hematologists with knowledge of hematological
protocols and side effects of the new molecules work together with the
hospitalist, can improve the assistance and outcomes of these patients.
Our initiative is the first operating in our city, and the hematological departments have very much welcomed it.
References
- Low J, Smith A, George S, Roderick P, Davis C. How
many patients with haematological malignancy need the facilities
offered by a district general hospital? J Public Health Med. 2002
Sep;24(3):196-9. https://doi.org/10.1093/pubmed/24.3.196 PMid:12831089
- Snowden
JA, O'Connell S, Hawkins J, Dalley C, Jack A, Mannari D, McNamara C,
Scott M, Shenton G, Soilleux E, Macbeth F; Guideline Committee.
Haematological cancers: improving outcomes. A summary of updated NICE
service guidance in relation to Specialist Integrated Haematological
Malignancy Diagnostic Services (SIHMDS). J Clin Pathol. 2017
Jun;70(6):461-468. https://doi.org/10.1136/jclinpath-2016-204029 PMid:28389440
- Kim K, Phelps MA. Clinical Pharmacokinetics and Pharmacodynamics of Daratumumab. Clin Pharmacokinet. 2023 Jun;62(6):789-806. https://doi.org/10.1007/s40262-023-01240-8 PMid:37129750
- Paul
B, Hamadeh I, Atrash S, Bhutani M, Voorhees P, Usmani SZ. Daratumumab
subcutaneous formulation for the treatment of multiple myeloma. Expert
Opin Biol Ther. 2020 Nov;20(11):1253-1259. https://doi.org/10.1080/14712598.2020.1806231 PMid:32750265
- De
Angelis G., Fiorini A., Trapè G., Panichi V., Chavez M.G., Emanueli
Cippitelli E., Innocenti V., Perazzini R., Talucci R., Topini G., Di
Veroli A., Mercanti C., Natalino F., Tarnani M., Morucci M., Mastini
C., Silvestri A., Andriani A., Montanaro M., Ciambella S., Latagliata
R. Subcutaneous Daratumumab at Home Is a Safe and Effective Procedure
for Frail Patients with Multiple Myeloma: A Myelhome Project Report,
Blood (2023) 142 (Supplement 1): 7242.https://doi.org/10.1182/blood-2023-187362
- Sanguinetti
JM, Martínez D, Dimase F, Streich G, Castro P, Vega V, Batagelj E.
Patient Safety and Satisfaction in Home Chemotherapy. Home Healthc Now.
2021 May-Jun 01;39(3):139-144. https://doi.org/10.1097/NHH.0000000000000958 PMid:33955927
- Lüthi
F, Fucina N, Divorne N, Santos-Eggimann B, Currat-Zweifel C, Rollier P,
Wasserfallen JB, Ketterer N, Leyvraz S. Home care--a safe and
attractive alternative to inpatient administration of intensive
chemotherapies. Support Care Cancer. 2012 Mar;20(3):575-81. https://doi.org/10.1007/s00520-011-1125-9 PMid:21384139
- Joo
EH, Rha SY, Ahn JB, Kang HY. Economic and patient-reported outcomes of
outpatient home-based versus inpatient hospital-based chemotherapy for
patients with colorectal cancer. Support Care Cancer. 2011
Jul;19(7):971-8. https://doi.org/10.1007/s00520-010-0917-7 PMid:2049615