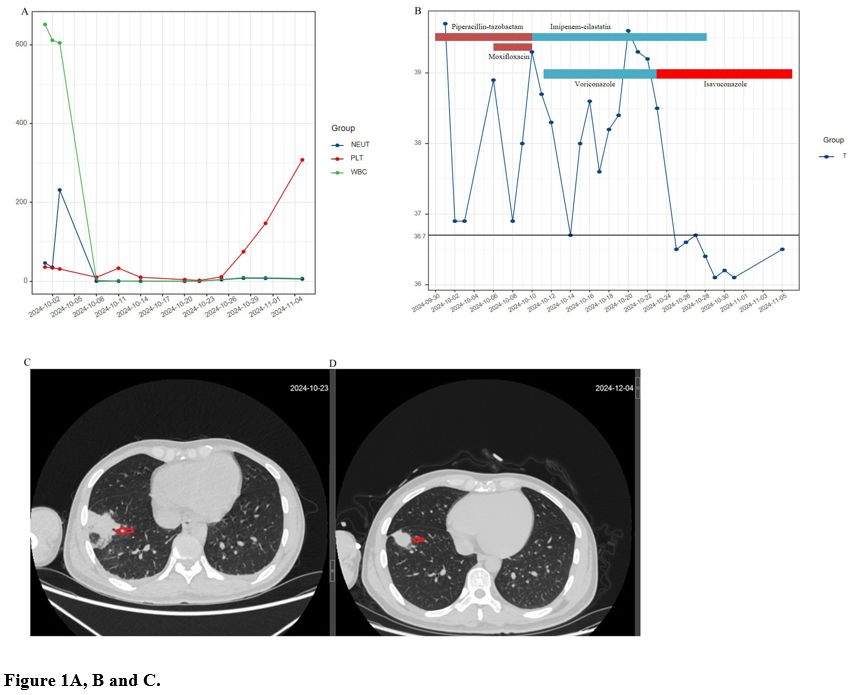
A 31-year-old Chinese male was admitted to the hematology department on September 30, 2024, with a continuous fever lasting over five days and bilateral axillary lymph node enlargement. Piperacillin-tazobactam was empirically initiated for suspected bloodstream infection. On October 1, blood tests revealed hemoglobin at 6.1 g/dL, red blood cell count at 1.71 × 10¹²/L, white blood cell count at 116.27 × 10⁹/L, absolute monocyte count at 77.32 × 10⁹/L, and platelets at 36.0 × 10⁹/L (Figure 1A). The patient’s maximum temperature was 39.7°C (Figure 1B), and interleukin-6 (IL-6) levels were 24.77 pg/mL. Bone marrow analysis confirmed acute myeloid leukemia (AML) M4 subtype with 58% myeloid blasts and mutations in FLT3, KRAS, PHF6, RUNX1, and WT1. Flow cytometry showed positivity for CD38, HLA-DR, CD13, CD33, CD11b, CD14, CD64, CD4 (partial), and cMPO (partial), while CD34, CD117, and lymphoid markers were negative. The patient was started on the DAV regimen (daunorubicin, cytarabine, venetoclax) on October 5.
Despite six days of piperacillin-tazobactam, the patient had persistent fevers, and a chest CT showed no signs of infection. The anti-infective regimen was adjusted to piperacillin-tazobactam combined with moxifloxacin on October 6 and further switched to imipenem-cilastatin with voriconazole on October 10 due to persistent fever. On October 23, chest CT revealed a patchy consolidation in the lower lobe of the right lung (Figure 1C). Peripheral blood mNGS identified Cunninghamella bertholletiae (Reads: 23; Relative abundance: 3.24%). Blood cultures and G and GM tests were repeatedly negative during treatment. A histopathologic specimen could not be obtained due to severe thrombocytopenia. Based on the 2019 EORTC/MSG criteria[6] and the mNGS findings, possible pulmonary mucormycosis was diagnosed, and the treatment regimen was changed to imipenem-cilastatin with isavuconazole. Following isavuconazole administration, the patient’s fever resolved. A chest CT on November 5 showed significant improvement in the pulmonary consolidation, and the patient was discharged on oral isavuconazole. By December 4, follow-up CT scans revealed further resolution of the lung lesion (Figure 1D). The patient continues oral isavuconazole without adverse events and is awaiting subsequent chemotherapy.
Although the patient was successfully treated, this study has limitations. Due to the patient's extremely low platelet count, a pathological examination could not be performed, preventing definitive confirmation of the fungal infection and allowing only a probable diagnosis. Additionally, the minimum inhibitory concentration of isavuconazole against Cunninghamella bertholletiae was not obtained.
In conclusion, this case highlights the diagnostic value of mNGS for pulmonary mucormycosis in hematological malignancies and supports the efficacy and tolerability of isavuconazole in treating this condition.
Ethics approval and consent to participate
The study protocol was approved by the Medical Ethics Committee of the First People’s Hospital of Zigong. The patient gave informed consent for the publication of this case report.References
- Muthu V, Agarwal R, Dhooria S, et al. Has the
mortality from pulmonary mucormycosis changed over time? A systematic
review and meta-analysis. Clinical microbiology and infection: the
official publication of the European Society of Clinical Microbiology
and Infectious Diseases. 2021;27:538-549. https://doi.org/10.1016/j.cmi.2020.12.035 PMid:33418022
- Suo
T, Xu M, Xu Q. Clinical characteristics and mortality of mucormycosis
in hematological malignancies: a retrospective study in Eastern China.
Annals of clinical microbiology and antimicrobials. 2024;23:82. https://doi.org/10.1186/s12941-024-00738-8 PMid:39210448 PMCid:PMC11363688
- Mauro
M, Lo Cascio G, Balter R, Zaccaron A, Bonetti E, Vitale V, Chinello M,
De Bortoli M, Brazzarola P, Bruno C, Cesaro S. The Diagnostic Pitfalls
of Mucormycosis. Mediterr J Hematol Infect Dis. 2020 November
1;12(1):e2020079. doi: 10.4084/MJHID.2020.079 https://doi.org/10.4084/mjhid.2020.079 PMid:33194153 PMCid:PMC7643780
- Marty
FM, Ostrosky-Zeichner L, Cornely OA, et al. Isavuconazole treatment for
mucormycosis: a single-arm open-label trial and case-control analysis.
The Lancet. Infectious diseases. 2016;16:828-837. https://doi.org/10.1016/S1473-3099(16)00071-2 PMid:26969258
- Wang
J, Liu L, Li J, et al. Clinical Characteristics, Prognosis Factors and
Metagenomic Next-Generation Sequencing Diagnosis of Mucormycosis in
patients With Hematologic Diseases. Mycopathologia. 2024;189:71. https://doi.org/10.1007/s11046-024-00875-w PMid:39088077
- Donnelly JP, Chen SC, Kauffman CA, et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease From the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America. 2020;71:1367-1376. https://doi.org/10.1093/cid/ciz1008 PMid:31802125 PMCid:PMC7486838